Wound healing refers to a living organism's replacement of destroyed or damaged tissue by newly produced tissue.
In undamaged skin, the
epidermis
The epidermis is the outermost of the three layers that comprise the skin, the inner layers being the dermis and hypodermis. The epidermis layer provides a barrier to infection from environmental pathogens and regulates the amount of water rele ...
(surface,
epithelial layer) and
dermis
The dermis or corium is a layer of skin between the epidermis (with which it makes up the cutis) and subcutaneous tissues, that primarily consists of dense irregular connective tissue and cushions the body from stress and strain. It is divided i ...
(deeper,
connective layer) form a protective barrier against the external environment. When the barrier is broken, a regulated sequence of biochemical events is set into motion to repair the damage.
This process is divided into predictable phases: blood clotting (
hemostasis),
inflammation, tissue growth (
cell proliferation
Cell proliferation is the process by which ''a cell grows and divides to produce two daughter cells''. Cell proliferation leads to an exponential increase in cell number and is therefore a rapid mechanism of tissue growth. Cell proliferation re ...
), and tissue remodeling (maturation and
cell differentiation
Cellular differentiation is the process in which a stem cell alters from one type to a differentiated one. Usually, the cell changes to a more specialized type. Differentiation happens multiple times during the development of a multicellula ...
). Blood clotting may be considered to be part of the inflammation stage instead of a separate stage.
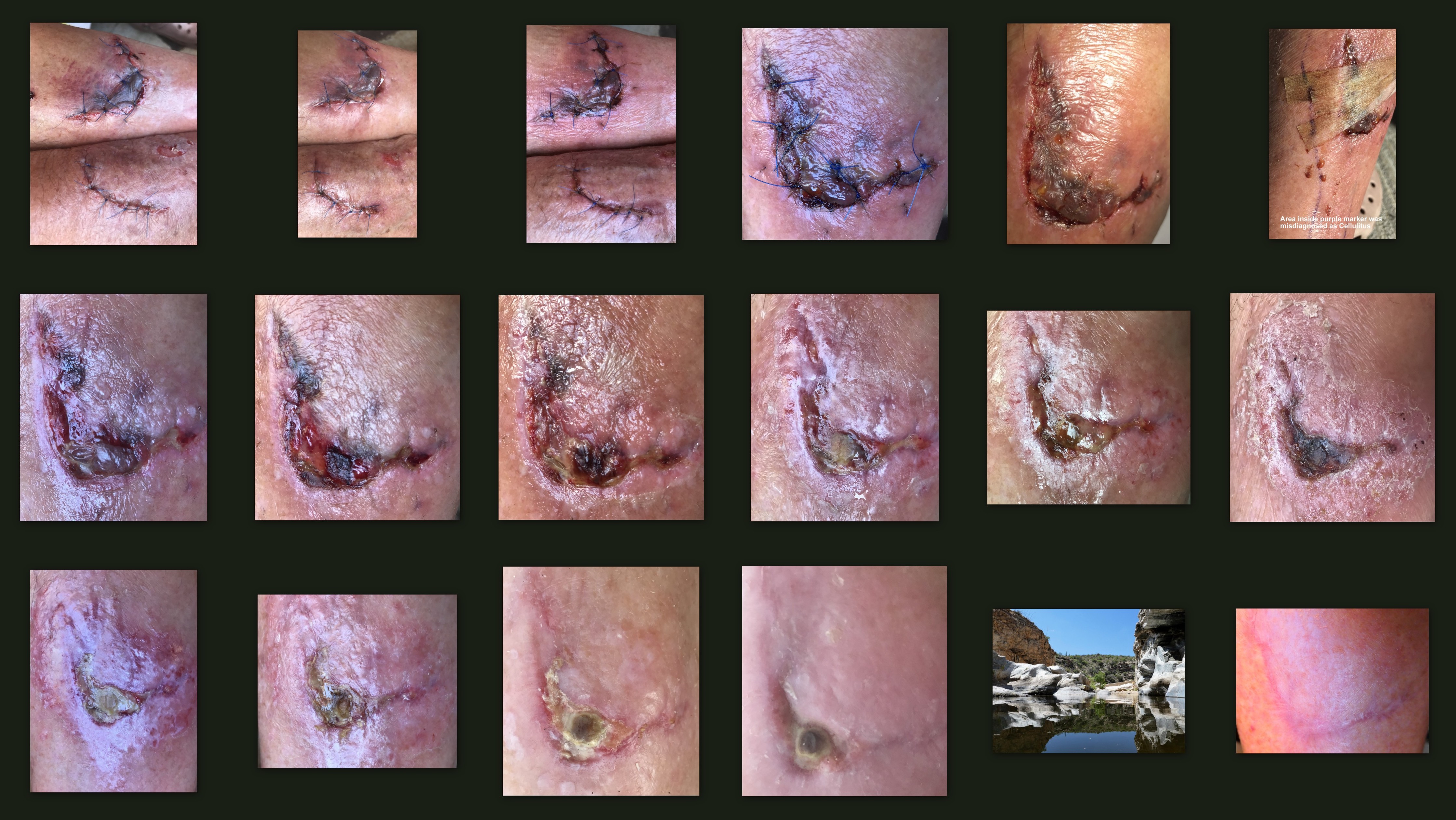
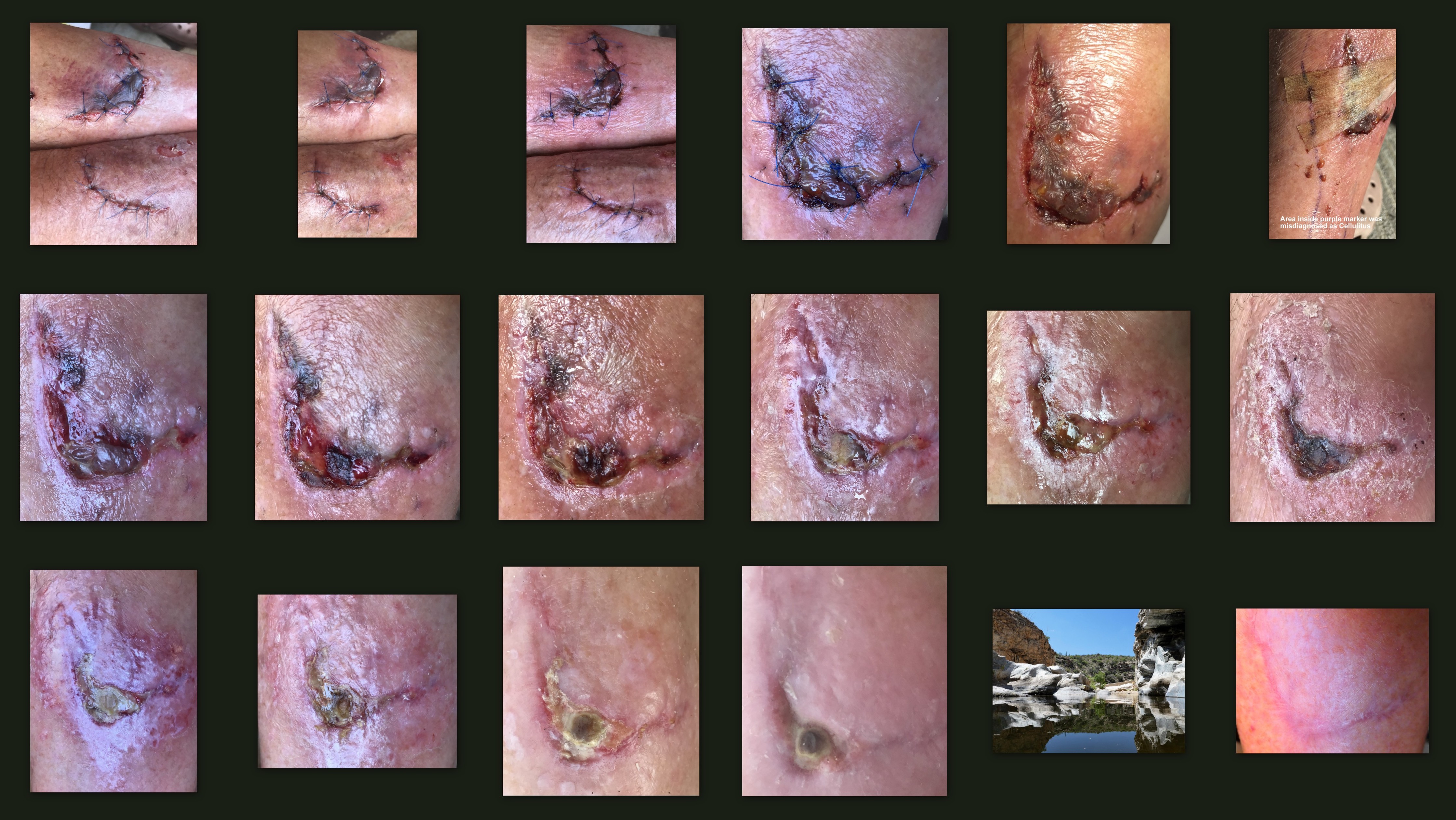
The wound healing process is not only complex but fragile, and it is susceptible to interruption or failure leading to the formation of non-healing
chronic wounds. Factors that contribute to non-healing chronic wounds are diabetes, venous or arterial disease, infection, and metabolic deficiencies of old age.
[Enoch, S. Price, P. (2004)]
''Cellular, molecular and biochemical differences in the pathophysiology of healing between acute wounds, chronic wounds and wounds in the elderly''
.
Wound care encourages and speeds wound healing via cleaning and protection from reinjury or infection. Depending on each patient's needs, it can range from the simplest
first aid to entire nursing specialties such as
wound, ostomy, and continence nursing and
burn center care.
Stages
* Hemostasis (blood clotting): Within the first few minutes of injury,
platelets
Platelets, also called thrombocytes (from Greek θρόμβος, "clot" and κύτος, "cell"), are a component of blood whose function (along with the coagulation factors) is to react to bleeding from blood vessel injury by clumping, thereby ini ...
in the blood begin to stick to the injured site. They change into an amorphous shape, more suitable for clotting, and they release chemical signals to promote clotting. This results in the activation of
fibrin
Fibrin (also called Factor Ia) is a fibrous, non-globular protein involved in the clotting of blood. It is formed by the action of the protease thrombin on fibrinogen, which causes it to polymerize. The polymerized fibrin, together with platele ...
, which forms a mesh and acts as "glue" to bind platelets to each other. This makes a
clot that serves to plug the break in the blood vessel, slowing/preventing further bleeding.
* Inflammation: During this phase, damaged and dead cells are cleared out, along with bacteria and other pathogens or debris. This happens through the process of
phagocytosis, where white blood cells engulf debris and destroy it.
Platelet-derived growth factors are released into the wound that cause the migration and division of cells during the proliferative phase.
* Proliferation (growth of new tissue): In this phase,
angiogenesis
Angiogenesis is the physiological process through which new blood vessels form from pre-existing vessels, formed in the earlier stage of vasculogenesis. Angiogenesis continues the growth of the vasculature by processes of sprouting and splitting ...
,
collagen
Collagen () is the main structural protein in the extracellular matrix found in the body's various connective tissues. As the main component of connective tissue, it is the most abundant protein in mammals, making up from 25% to 35% of the whole ...
deposition,
granulation tissue formation, epithelialization, and wound contraction occur.
In angiogenesis, vascular endothelial cells form new blood vessels.
In fibroplasia and granulation tissue formation,
fibroblast
A fibroblast is a type of cell (biology), biological cell that synthesizes the extracellular matrix and collagen, produces the structural framework (Stroma (tissue), stroma) for animal Tissue (biology), tissues, and plays a critical role in wound ...
s grow and form a new, provisional
extracellular matrix (ECM) by excreting collagen and
fibronectin.
Concurrently, re-epithelialization of the epidermis occurs, in which
epithelial cell
Epithelium or epithelial tissue is one of the four basic types of animal tissue, along with connective tissue, muscle tissue and nervous tissue. It is a thin, continuous, protective layer of compactly packed cells with a little intercellula ...
s proliferate and 'crawl' atop the wound bed, providing cover for the new tissue.
[Garg, H.G. (2000). ''Scarless Wound Healing''. New York Marcel Dekker, Inc. Electronic book.] In wound contraction,
myofibroblasts decrease the size of the wound by gripping the wound edges and contracting using a mechanism that resembles that in smooth muscle cells. When the cells' roles are close to complete, unneeded cells undergo
apoptosis
Apoptosis (from grc, ἀπόπτωσις, apóptōsis, 'falling off') is a form of programmed cell death that occurs in multicellular organisms. Biochemical events lead to characteristic cell changes (morphology) and death. These changes incl ...
.
* Maturation (remodeling): During maturation and remodeling, collagen is realigned along tension lines, and cells that are no longer needed are removed by programmed cell death, or
apoptosis
Apoptosis (from grc, ἀπόπτωσις, apóptōsis, 'falling off') is a form of programmed cell death that occurs in multicellular organisms. Biochemical events lead to characteristic cell changes (morphology) and death. These changes incl ...
.

Timing and re-epithelialization
Timing is important to wound healing. Critically, the timing of wound re-epithelialization can decide the outcome of the healing.
If the epithelization of tissue over a denuded area is slow, a scar will form over many weeks, or months;
[ If the epithelization of a wounded area is fast, the healing will result in regeneration.]
Early vs cellular phase
Wound healing is classically divided into hemostasis, inflammation, proliferation, and remodeling. Although a useful construct, this model employs considerable overlapping among individual phases. A complementary model has recently been describedMacrophage
Macrophages (abbreviated as M φ, MΦ or MP) ( el, large eaters, from Greek ''μακρός'' (') = large, ''φαγεῖν'' (') = to eat) are a type of white blood cell of the immune system that engulfs and digests pathogens, such as cancer cel ...
s and inflammatory components (within 1–2 days)
# Epithelial- mesenchymal interaction: re-epithelialization ( phenotype change within hours, migration begins on day 1 or 2)
# Fibroblasts and myofibroblasts: progressive alignment, collagen production, and matrix contraction (between day 4 and day 14)
# Endothelial cell
The endothelium is a single layer of squamous endothelial cells that line the interior surface of blood vessels and lymphatic vessels. The endothelium forms an interface between circulating blood or lymph in the lumen and the rest of the vessel ...
s and angiogenesis (begins on day 4)
# Dermal matrix: elements of fabrication (begins on day 4, lasting 2 weeks) and alteration/remodeling (begins after week 2, lasting weeks to months—depending on wound size).
Inflammatory phase
Just before the inflammatory phase is initiated, the clotting cascade occurs in order to achieve hemostasis, or the stopping of blood loss by way of a fibrin clot. Thereafter, various soluble factors (including chemokines and cytokines) are released to attract cells that phagocytise debris, bacteria, and damaged tissue, in addition to releasing signaling molecules that initiate the proliferative phase of wound healing.
Clotting cascade
When tissue is first wounded, blood comes in contact with collagen
Collagen () is the main structural protein in the extracellular matrix found in the body's various connective tissues. As the main component of connective tissue, it is the most abundant protein in mammals, making up from 25% to 35% of the whole ...
, triggering blood platelets to begin secreting inflammatory factors.[Rosenberg L., de la Torre J. (2006)]
Wound Healing, Growth Factors
. Emedicine.com. Accessed January 20, 2008. Platelets also express sticky glycoprotein
Glycoproteins are proteins which contain oligosaccharide chains covalently attached to amino acid side-chains. The carbohydrate is attached to the protein in a cotranslational or posttranslational modification. This process is known as glycos ...
s on their cell membranes that allow them to aggregate
Aggregate or aggregates may refer to:
Computing and mathematics
* collection of objects that are bound together by a root entity, otherwise known as an aggregate root. The aggregate root guarantees the consistency of changes being made within the ...
, forming a mass.Fibrin
Fibrin (also called Factor Ia) is a fibrous, non-globular protein involved in the clotting of blood. It is formed by the action of the protease thrombin on fibrinogen, which causes it to polymerize. The polymerized fibrin, together with platele ...
and fibronectin cross-link together and form a plug that traps proteins and particles and prevents further blood loss.serotonin
Serotonin () or 5-hydroxytryptamine (5-HT) is a monoamine neurotransmitter. Its biological function is complex and multifaceted, modulating mood, cognition, reward, learning, memory, and numerous physiological processes such as vomiting and vas ...
, bradykinin, prostaglandin
The prostaglandins (PG) are a group of physiologically active lipid compounds called eicosanoids having diverse hormone-like effects in animals. Prostaglandins have been found in almost every tissue in humans and other animals. They are derive ...
s, prostacyclins, thromboxane, and histamine,macrophage
Macrophages (abbreviated as M φ, MΦ or MP) ( el, large eaters, from Greek ''μακρός'' (') = large, ''φαγεῖν'' (') = to eat) are a type of white blood cell of the immune system that engulfs and digests pathogens, such as cancer cel ...
s and mast cells exposed to microbial molecular signatures in infection: they become activated, and secrete molecular mediators – vasoactive amines, eicosanoids, and cytokines – that initiate the inflammatory process.
Vasoconstriction and vasodilation
Immediately after a blood vessel is breached, ruptured cell membranes release inflammatory factors like thromboxanes and prostaglandin
The prostaglandins (PG) are a group of physiologically active lipid compounds called eicosanoids having diverse hormone-like effects in animals. Prostaglandins have been found in almost every tissue in humans and other animals. They are derive ...
s that cause the vessel to spasm to prevent blood loss and to collect inflammatory cells and factors in the area.edema
Edema, also spelled oedema, and also known as fluid retention, dropsy, hydropsy and swelling, is the build-up of fluid in the body's Tissue (biology), tissue. Most commonly, the legs or arms are affected. Symptoms may include skin which feels t ...
tous because proteins from the bloodstream leak into the extravascular space, which increases its osmolar load and draws water into the area.leukocyte
White blood cells, also called leukocytes or leucocytes, are the cells of the immune system that are involved in protecting the body against both infectious disease and foreign invaders. All white blood cells are produced and derived from mult ...
s into the wound site from the bloodstream.[Dealey C. (1999). ''The care of wounds: A guide for nurses''. Oxford; Malden, Mass. Blackwell Science. Electronic book.]
Polymorphonuclear neutrophils
Within an hour of wounding, polymorphonuclear neutrophils (PMNs) arrive at the wound site and become the predominant cells in the wound for the first two days after the injury occurs, with especially high numbers on the second day.[de la Torre J., Sholar A. (2006)]
Wound healing: Chronic wounds
. Emedicine.com. Accessed January 20, 2008. They are attracted to the site by fibronectin, growth factors, and substances such as kinins. Neutrophils phagocytise debris and kill bacteria by releasing free radicals in what is called a respiratory burst.macrophage
Macrophages (abbreviated as M φ, MΦ or MP) ( el, large eaters, from Greek ''μακρός'' (') = large, ''φαγεῖν'' (') = to eat) are a type of white blood cell of the immune system that engulfs and digests pathogens, such as cancer cel ...
s.cytokines
Cytokines are a broad and loose category of small proteins (~5–25 kDa) important in cell signaling. Cytokines are peptides and cannot cross the lipid bilayer of cells to enter the cytoplasm. Cytokines have been shown to be involved in autocrin ...
to cause more T cells to divide and to increase inflammation and enhance vasodilation and vessel permeability.
Macrophages
One of the roles of macrophages is to phagocytize other expended phagocytes,angiogenesis
Angiogenesis is the physiological process through which new blood vessels form from pre-existing vessels, formed in the earlier stage of vasculogenesis. Angiogenesis continues the growth of the vasculature by processes of sprouting and splitting ...
Decline of inflammatory phase
As inflammation dies down, fewer inflammatory factors are secreted, existing ones are broken down, and numbers of neutrophils and macrophages are reduced at the wound site.dermal equivalent The dermal equivalent, also known as dermal replacement or neodermis, is an ''in vitro'' model of the dermal layer of skin. There is no specific way of forming a dermal equivalent, however the first dermal equivalent was constructed by seeding derma ...
model, suggests that the presence of macrophages actually delays wound contraction and thus the disappearance of macrophages from the wound may be essential for subsequent phases to occur.
Proliferative phase
About two or three days after the wound occurs, fibroblasts begin to enter the wound site, marking the onset of the proliferative phase even before the inflammatory phase has ended.[Falanga V. (2005). Wound Healing. American Academy of Dermatology (AAD).] As in the other phases of wound healing, steps in the proliferative phase do not occur in a series but rather partially overlap in time.
Angiogenesis
Also called neovascularization, the process of angiogenesis occurs concurrently with fibroblast proliferation when endothelial cells migrate to the area of the wound.[Kuwahara R.T. and Rasberry R. 2007.]
Chemical Peels
. Emedicine.com. Accessed September 15, 2007. Because the activity of fibroblasts and epithelial cells requires oxygen and nutrients, angiogenesis is imperative for other stages in wound healing, like epidermal and fibroblast migration. The tissue in which angiogenesis has occurred typically looks red (is erythematous) due to the presence of capillaries.Stem cell
In multicellular organisms, stem cells are undifferentiated or partially differentiated cells that can differentiate into various types of cells and proliferate indefinitely to produce more of the same stem cell. They are the earliest type o ...
s of endothelial cell
The endothelium is a single layer of squamous endothelial cells that line the interior surface of blood vessels and lymphatic vessels. The endothelium forms an interface between circulating blood or lymph in the lumen and the rest of the vessel ...
s, originating from parts of uninjured blood vessels, develop pseudopodia and push through the ECM
ECM may refer to:
Economics and commerce
* Engineering change management
* Equity capital markets
* Error correction model, an econometric model
* European Common Market
Mathematics
* Elliptic curve method
* European Congress of Mathematics
...
into the wound site to establish new blood vessels.Endothelial cell
The endothelium is a single layer of squamous endothelial cells that line the interior surface of blood vessels and lymphatic vessels. The endothelium forms an interface between circulating blood or lymph in the lumen and the rest of the vessel ...
s are attracted to the wound area by fibronectin found on the fibrin scab and chemotactically by angiogenic factors released by other cells,[Romo T. and Pearson J.M. 2005.]
Wound Healing, Skin
. Emedicine.com. Accessed December 27, 2006. e.g. from macrophages and platelets when in a low-oxygen environment. Endothelial growth and proliferation is also directly stimulated by hypoxia
Hypoxia means a lower than normal level of oxygen, and may refer to:
Reduced or insufficient oxygen
* Hypoxia (environmental), abnormally low oxygen content of the specific environment
* Hypoxia (medical), abnormally low level of oxygen in the tis ...
, and presence of lactic acid in the wound.transactivate In the context of gene regulation: transactivation is the increased rate of gene expression triggered either by biological processes or by artificial means, through the expression of an intermediate transactivator protein.
In the context of rece ...
a set of proliferative genes including vascular endothelial growth factor (VEGF) and glucose transporter 1 (GLUT1).
To migrate, endothelial cells need collagenases and plasminogen activator to degrade the clot and part of the ECM.basement membrane
The basement membrane is a thin, pliable sheet-like type of extracellular matrix that provides cell and tissue support and acts as a platform for complex signalling. The basement membrane sits between Epithelium, epithelial tissues including mesot ...
and ECM to allow cell migration, proliferation and angiogenesis.apoptosis
Apoptosis (from grc, ἀπόπτωσις, apóptōsis, 'falling off') is a form of programmed cell death that occurs in multicellular organisms. Biochemical events lead to characteristic cell changes (morphology) and death. These changes incl ...
.
Fibroplasia and granulation tissue formation
Simultaneously with angiogenesis, fibroblast
A fibroblast is a type of cell (biology), biological cell that synthesizes the extracellular matrix and collagen, produces the structural framework (Stroma (tissue), stroma) for animal Tissue (biology), tissues, and plays a critical role in wound ...
s begin accumulating in the wound site. Fibroblasts begin entering the wound site two to five days after wounding as the inflammatory phase is ending, and their numbers peak at one to two weeks post-wounding.elastin
Elastin is a protein that in humans is encoded by the ''ELN'' gene. Elastin is a key component of the extracellular matrix in gnathostomes (jawed vertebrates). It is highly elastic and present in connective tissue allowing many tissues in the bod ...
, glycoprotein
Glycoproteins are proteins which contain oligosaccharide chains covalently attached to amino acid side-chains. The carbohydrate is attached to the protein in a cotranslational or posttranslational modification. This process is known as glycos ...
s and proteoglycan
Proteoglycans are proteins that are heavily glycosylated. The basic proteoglycan unit consists of a "core protein" with one or more covalently attached glycosaminoglycan (GAG) chain(s). The point of attachment is a serine (Ser) residue to whic ...
s.hyaluronan
Hyaluronic acid (; abbreviated HA; conjugate base hyaluronate), also called hyaluronan, is an anionic, nonsulfated glycosaminoglycan distributed widely throughout connective, epithelial, and neural tissues. It is unique among glycosaminoglycans ...
, which create a very hydrated matrix and facilitate cell migration.
Collagen deposition
One of fibroblasts' most important duties is the production of collagen
Collagen () is the main structural protein in the extracellular matrix found in the body's various connective tissues. As the main component of connective tissue, it is the most abundant protein in mammals, making up from 25% to 35% of the whole ...
.[Fig. 9-1. The cellular, biochemical, and mechanical phases of wound healing. ] and 3 days,
Epithelialization
The formation of granulation tissue into an open wound allows the reepithelialization phase to take place, as epithelial cells migrate across the new tissue to form a barrier between the wound and the environment.Basal
Basal or basilar is a term meaning ''base'', ''bottom'', or ''minimum''.
Science
* Basal (anatomy), an anatomical term of location for features associated with the base of an organism or structure
* Basal (medicine), a minimal level that is nec ...
keratinocytes from the wound edges and dermal appendage
The hair follicle is an organ found in mammalian skin. It resides in the dermal layer of the skin and is made up of 20 different cell types, each with distinct functions. The hair follicle regulates hair growth via a complex interaction between ho ...
s such as hair follicle
The hair follicle is an organ found in mammalian skin. It resides in the dermal layer of the skin and is made up of 20 different cell types, each with distinct functions. The hair follicle regulates hair growth via a complex interaction between h ...
s, sweat glands and sebacious (oil) glands are the main cells responsible for the epithelialization phase of wound healing.[ and nerves do not form. With the lack of hair follicles, nerves and sweat glands, the wound, and the resulting healing scar, provide a challenge to the body with regards to temperature control.][Mulvaney M. and Harrington A. 1994.]
Chapter 7: Cutaneous trauma and its treatment
In, ''Textbook of Military Medicine: Military Dermatology''. Office of the Surgeon General, Department of the Army. Virtual Naval Hospital Project. Accessed through web archive on September 15, 2007. Thus the time of onset of migration is variable and may occur about one day after wounding.[Larjava H., Koivisto L., and Hakkinen L. 2002. Chapter 3: Keratinocyte Interactions with Fibronectin During Wound Healing. In, Heino, J. and Kahari, V.M. ''Cell Invasion''. Medical Intelligence Unit; 33. Georgetown, Tex., Austin, Tex Landes Bioscience, Inc. Electronic book.] Cells on the wound margins proliferate on the second and third day post-wounding in order to provide more cells for migration.basement membrane
The basement membrane is a thin, pliable sheet-like type of extracellular matrix that provides cell and tissue support and acts as a platform for complex signalling. The basement membrane sits between Epithelium, epithelial tissues including mesot ...
is not breached, epithelial cells are replaced within three days by division and upward migration of cells in the stratum basale in the same fashion that occurs in uninjured skin.dermis
The dermis or corium is a layer of skin between the epidermis (with which it makes up the cutis) and subcutaneous tissues, that primarily consists of dense irregular connective tissue and cushions the body from stress and strain. It is divided i ...
that are lined with viable keratinocytes.nitric oxide
Nitric oxide (nitrogen oxide or nitrogen monoxide) is a colorless gas with the formula . It is one of the principal oxides of nitrogen. Nitric oxide is a free radical: it has an unpaired electron, which is sometimes denoted by a dot in its che ...
.glycoprotein
Glycoproteins are proteins which contain oligosaccharide chains covalently attached to amino acid side-chains. The carbohydrate is attached to the protein in a cotranslational or posttranslational modification. This process is known as glycos ...
s and normally anchor the cell to the basement membrane by its cytoskeleton, are released from the cell's intermediate filaments and relocate to actin filaments to serve as attachments to the ECM for pseudopodia during migration.basement membrane
The basement membrane is a thin, pliable sheet-like type of extracellular matrix that provides cell and tissue support and acts as a platform for complex signalling. The basement membrane sits between Epithelium, epithelial tissues including mesot ...
form the stratum basale. These basal cells continue to migrate across the wound bed, and epithelial cells above them slide along as well.Fibrin
Fibrin (also called Factor Ia) is a fibrous, non-globular protein involved in the clotting of blood. It is formed by the action of the protease thrombin on fibrinogen, which causes it to polymerize. The polymerized fibrin, together with platele ...
, collagen, and fibronectin in the ECM may further signal cells to divide and migrate. Like fibroblasts, migrating keratinocytes use the fibronectin cross-linked with fibrin that was deposited in inflammation as an attachment site to crawl across. As keratinocytes migrate, they move over granulation tissue but stay underneath the scab, thereby separating the scab from the underlying tissue.
As keratinocytes migrate, they move over granulation tissue but stay underneath the scab, thereby separating the scab from the underlying tissue.
Contraction
Contraction is a key phase of wound healing with repair. If contraction continues for too long, it can lead to disfigurement and loss of function.collagen gel contraction assay
The collagen gel contraction assay is a type of wound contraction. It is performed using the dermal equivalent model, which consists of dermal fibroblasts seeded into a collagen gel.
References
Skin physiology
{{med-stub ...
or the dermal equivalent The dermal equivalent, also known as dermal replacement or neodermis, is an ''in vitro'' model of the dermal layer of skin. There is no specific way of forming a dermal equivalent, however the first dermal equivalent was constructed by seeding derma ...
model.full thickness
Full may refer to:
* People with the surname Full, including:
** Mr. Full (given name unknown), acting Governor of German Cameroon, 1913 to 1914
* A property in the mathematical field of topology; see Full set
* A property of functors in the mathe ...
wounds, contraction peaks at 5 to 15 days post wounding.smooth muscle
Smooth muscle is an involuntary non-striated muscle, so-called because it has no sarcomeres and therefore no striations (''bands'' or ''stripes''). It is divided into two subgroups, single-unit and multiunit smooth muscle. Within single-unit mus ...
cells.
Maturation and remodeling
When the levels of collagen production and degradation equalize, the maturation phase of tissue repair is said to have begun.tension lines
Langer's lines, Langer lines of skin tension, or sometimes called cleavage lines, are topological lines drawn on a map of the human body. They are parallel to the natural orientation of collagen fibers in the dermis, and generally perpendicular to ...
.[ to three weeks. The maturation phase can last for a year or longer, similarly depending on wound type.]apoptosis
Apoptosis (from grc, ἀπόπτωσις, apóptōsis, 'falling off') is a form of programmed cell death that occurs in multicellular organisms. Biochemical events lead to characteristic cell changes (morphology) and death. These changes incl ...
.venous ulcer
Venous ulcer is defined by the American Venous Forum as "a full-thickness defect of skin, most frequently in the ankle region, that fails to heal spontaneously and is sustained by chronic venous disease, based on venous duplex ultrasound testing." ...
or pathological scarring such as a keloid scar
Keloid, also known as keloid disorder and keloidal scar,
is the formation of a type of scar which, depending on its maturity, is composed mainly of either type III (early) or type I (late) collagen. It is a result of an overgrowth of granulation t ...
.
Factors affecting wound healing
Many factors controlling the efficacy, speed, and manner of wound healing fall under two types: local and systemic factors.
Local factors
* Moisture; keeping a wound moist rather than dry makes wound healing more rapid and with less pain and less scarring
* Mechanical factors
* Oedema
* Ionizing radiation
Ionizing radiation (or ionising radiation), including nuclear radiation, consists of subatomic particles or electromagnetic waves that have sufficient energy to ionize atoms or molecules by detaching electrons from them. Some particles can travel ...
* Faulty technique of wound closure
* Ischemia
Ischemia or ischaemia is a restriction in blood supply to any tissue, muscle group, or organ of the body, causing a shortage of oxygen that is needed for cellular metabolism (to keep tissue alive). Ischemia is generally caused by problems wi ...
and necrosis
Necrosis () is a form of cell injury which results in the premature death of cells in living tissue by autolysis. Necrosis is caused by factors external to the cell or tissue, such as infection, or trauma which result in the unregulated dige ...
* Foreign bodies. Sharp, small foreign bodies can penetrate the skin leaving little surface wound but causing internal injury and internal bleeding. For a glass foreign body, "frequently, an innocent skin wound disguises the extensive nature of the injuries beneath". First-degree nerve injury requires a few hours to a few weeks to recover. If a foreign body passes by a nerve and causes first-degree nerve injury during entry, then the sensation of the foreign body or pain due to internal wounding may be delayed by a few hours to a few weeks after entry. A sudden increase in pain during the first few weeks of wound healing could be a sign of a recovered nerve reporting internal injuries rather than a newly developed infection.
* Low oxygen tension
* Perfusion
Systemic factors
* Inflammation
* Diabetes – Individuals with diabetes demonstrate reduced capability in the healing of acute wounds. Additionally, diabetic individuals are susceptible to developing chronic diabetic foot ulcers, a serious complication of diabetes which affects 15% of people with diabetes and accounts for 84% of all diabetes-related lower leg amputations. The impaired healing abilities of diabetics with diabetic foot ulcers and/or acute wounds involves multiple pathophysiological mechanisms.Nutrient
A nutrient is a substance used by an organism to survive, grow, and reproduce. The requirement for dietary nutrient intake applies to animals, plants, fungi, and protists. Nutrients can be incorporated into cells for metabolic purposes or excret ...
s – Malnutrition or nutritional deficiencies have a recognizable impact on wound healing post trauma or surgical intervention. Nutrients including proteins, carbohydrates, arginine, glutamine, polyunsaturated fatty acids, vitamin A, vitamin C, vitamin E, magnesium, copper, zinc and iron all play significant roles in wound healing.Connective tissue
Connective tissue is one of the four primary types of animal tissue, along with epithelial tissue, muscle tissue, and nervous tissue. It develops from the mesenchyme derived from the mesoderm the middle embryonic germ layer. Connective tiss ...
disorders
* Smoking – Smoking causes a delay in the speed of wound repair notably in the proliferative and inflammatory phases. It also increases the likelihood of certain complications such as wound rupture, wound and flap necrosis, decrease in wound tensile strength and infection.
Research and development
Up until about 2000, the classic paradigm of wound healing, involving stem cells restricted to organ-specific lineages, had never been seriously challenged. Since then, the notion of adult stem cells having cellular ''plasticity'' or the ability to differentiate into non-lineage cells has emerged as an alternative explanation.hematopoietic
Haematopoiesis (, from Greek , 'blood' and 'to make'; also hematopoiesis in American English; sometimes also h(a)emopoiesis) is the formation of blood cellular components. All cellular blood components are derived from haematopoietic stem cells. ...
progenitor cells (that give rise to mature cells in the blood) may have the ability ''de-differentiate'' back into hematopoietic stem cells and/or ''transdifferentiate'' into non-lineage cells, such as fibroblasts.
Stem cells and cellular plasticity
Multipotent adult stem cells have the capacity to be self-renewing and give rise to different cell types. Stem cells give rise to progenitor cells, which are cells that are not self-renewing, but can generate several types of cells. The extent of stem cell involvement in cutaneous (skin) wound healing is complex and not fully understood. Stem cell injection leads to wound healing primarily through stimulation of angiogenesis.
It is thought that the epidermis and dermis are reconstituted by mitotically active stem cells that reside at the apex of rete ridges
Rete pegs (also known as rete processes or rete ridges) are the epithelial extensions that project into the underlying connective tissue in both skin and mucous membranes.
In the epithelium of the mouth, the attached gingiva exhibit rete pegs, wh ...
(basal stem cells or BSC), the bulge of hair follicle
The hair follicle is an organ found in mammalian skin. It resides in the dermal layer of the skin and is made up of 20 different cell types, each with distinct functions. The hair follicle regulates hair growth via a complex interaction between h ...
s (hair follicular stem cell or HFSC), and the papillary dermis (dermal stem cells).mesenchymal stem cells
Mesenchymal stem cells (MSCs) also known as mesenchymal stromal cells or medicinal signaling cells are multipotent stromal cells that can differentiate into a variety of cell types, including osteoblasts (bone cells), chondrocytes (cartilage ce ...
(MSC) and (2) hematopoietic stem cells (HSC). Bone marrow also harbors a progenitor subpopulation ( endothelial progenitor cells or EPC) that, in the same type of setting, are mobilized to aid in the reconstruction of blood vessels.
Wound repair versus regeneration
An injury is an interruption of morphology and/or functionality of a given tissue. After injury, structural tissue heals with incomplete or complete regeneration.[ Tissue without an interruption to the morphology almost always completely regenerates. An example of complete regeneration without an interruption of the morphology is non-injured tissue, such as skin.][ Non-injured skin has a continued replacement and regeneration of cells which always results in complete regeneration.][
There is a subtle distinction between 'repair' and 'regeneration'.][ ''Repair'' means ''incomplete regeneration''.][
''True tissue regeneration'' or ''complete regeneration'',][ Though after injury mammals can completely regenerate spontaneously, they usually do not completely regenerate. An example of a tissue regenerating completely after an interruption of morphology is the ]endometrium
The endometrium is the inner epithelial layer, along with its mucous membrane, of the mammalian uterus. It has a basal layer and a functional layer: the basal layer contains stem cells which regenerate the functional layer. The functional laye ...
; the endometrium after the process of breakdown via the menstruation cycle heals with complete regeneration.collagen
Collagen () is the main structural protein in the extracellular matrix found in the body's various connective tissues. As the main component of connective tissue, it is the most abundant protein in mammals, making up from 25% to 35% of the whole ...
- glycoaminoglycan) scaffolds. These scaffolds are structurally analogous to extracellular matrix (ECM) found in normal/un-injured dermis.Heparan sulfate analogue Heparan sulfate analogues are polymers engineered to mimic several properties of heparan sulfates. They can be constituted with a backbone of polysaccharides, such as poly glucose or glucuronatesPetit et al, Controlled sulfatation of natural anioni ...
s cannot be degraded by all known heparanases and glycanases and bind to the free heparin sulfate binding spots on the ECM, therefore preserving the normal tissue homeostasis and preventing scarring.[Van Neck et al, Heparan sulfate proteoglycan mimetics thrive tissue regeneration: an overview. In Intech book under the working title "Tissue Regeneration", is scheduled for on line publication on Nov 26, 2011"]
Repair or regeneration with regards to hypoxia-inducible factor 1-alpha (HIF-1a). In normal circumstances after injury HIF-1a is degraded by prolyl hydroxylases (PHDs). Scientists found that the simple up-regulation of HIF-1a via PHD inhibitors regenerates lost or damaged tissue in mammals that have a repair response; and the continued down-regulation of Hif-1a results in healing with a scarring response in mammals with a previous regenerative response to the loss of tissue. The act of regulating HIF-1a can either turn off, or turn on the key process of mammalian regeneration.[Zhang Y, Strehin I, Bedelbaeva K, Gourevitch D, Clark L, Leferovich J, Messersmith PB, Heber-Katz E. Drug-induced regeneration in adult mice. Sci Transl Med. 2015;290.]
Scarless wound healing
''Scarless wound healing'' is a concept based on the healing or repair of the skin (or other tissue/organs) after injury with the aim of healing with subjectively and relatively ''less'' scar tissue than normally expected. Scarless healing is sometimes mixed up with the concept of ''scar free healing
Scar free healing is the process by which significant injuries can heal without permanent damage to the tissue the injury has affected. In most healing, scars form due to the fibrosis and wound contraction, however in scar free healing, tissue is ...
,'' which is wound healing which results in absolutely no scar (''free'' of scarring). However they are different concepts.
A reverse to scarless wound healing is scarification (wound healing to scar more). Historically, certain cultures consider scarification attractive;[Rush, J. (2005). Spiritual tattoo: a cultural history of tattooing, piercing, scarification, branding, and implants, Frog Ltd.] however, this is generally not the case in the modern western society, in which many patients are turning to plastic surgery clinics with unrealistic expectations. Depending on scar type, treatment may be invasive
Invasive may refer to:
*Invasive (medical) procedure
*Invasive species
*Invasive observation, especially in reference to surveillance
*Invasively progressive spread of disease from one organ in the body to another, especially in reference to cancer ...
(intralesional steroid injections, surgery) and/or conservative ( compression therapy, topical silicone gel, brachytherapy, photodynamic therapy).[Clark, R. (1996). The molecular and cellular biology of wound repair, Springer Us.] Currently, the principal goals in wound management are to achieve rapid wound closure with a functional tissue that has minimal aesthetic scarring.regeneration
Regeneration may refer to:
Science and technology
* Regeneration (biology), the ability to recreate lost or damaged cells, tissues, organs and limbs
* Regeneration (ecology), the ability of ecosystems to regenerate biomass, using photosynthesis
...
is limited to lower vertebrates, such as salamanders, and invertebrates.collagen
Collagen () is the main structural protein in the extracellular matrix found in the body's various connective tissues. As the main component of connective tissue, it is the most abundant protein in mammals, making up from 25% to 35% of the whole ...
deposition, collagen remodelling and eventual scar formation, where fetal wound healing is believed to be more of a regenerative process with minimal or no scar formation.[ In print the antiquated concept of scarless healing was brought up the early 20th century and appeared in a paper published in the London Lancet. This process involved cutting in a surgical slant, instead of a right angle...; it was described in various Newspapers.]
Cancer
After inflammation, restoration of normal tissue integrity and function is preserved by feedback interactions between diverse cell types mediated by adhesion molecules and secreted cytokines. Disruption of normal feedback mechanisms in cancer threatens tissue integrity and enables a malignant tumor to escape the immune system. An example of the importance of the wound healing response within tumors is illustrated in work by Howard Chang and colleagues at Stanford University
Stanford University, officially Leland Stanford Junior University, is a private research university in Stanford, California. The campus occupies , among the largest in the United States, and enrolls over 17,000 students. Stanford is consider ...
studying Breast cancers.
Oral collagen supplements
Preliminary results are promising for th
short and long-term use of oral collagen supplements for wound healing
and skin aging. Oral collagen supplements also increase skin elasticity, hydration, and dermal collagen density. Collagen supplementation is generally safe with no reported adverse events. Further studies are needed to elucidate medical use in skin barrier diseases such as atopic dermatitis and to determine optimal dosing regimens.
Wound Dressings
Modern wound dressing to aid in wound repair have undergone considerable research and development in recent years. Scientists aim to develop wound dressings which have the following characteristics:exudate
An exudate is a fluid emitted by an organism through pores or a wound, a process known as exuding or exudation.
''Exudate'' is derived from ''exude'' 'to ooze' from Latin ''exsūdāre'' 'to (ooze out) sweat' (''ex-'' 'out' and ''sūdāre'' 'to ...
* Antimicrobial properties
* Maintain a humid environment
* Have high permeability to oxygen
* Easily removed from a wound site
* Non- anaphylactic characteristics
Cotton gauze dressings have been the standard of care, despite their dry properties that can adhere to wound surfaces and cause discomfort upon removal. Recent research has set out to improve cotton gauze dressings to bring them closer in line to achieve modern wound dressing properties, by coating cotton gauze wound dressing with a chitosan/ Ag/ ZnO nanocomposite. These updated dressing provide increase water absorbency and improved antibacterial efficacy
Efficacy is the ability to perform a task to a satisfactory or expected degree. The word comes from the same roots as ''effectiveness'', and it has often been used synonymously, although in pharmacology a pragmatic clinical trial#Efficacy versu ...
.
Wound cleansing
Dirt or dust on the surface of the wound, bacteria, tissue that has died, and fluid from the wound may be cleaned. The evidence supporting the most effective technique is not clear and there is insufficient evidence to conclude whether cleaning wounds is beneficial for promoting healing or whether wound cleaning solutions (polyhexamethylene biguanide, aqueous oxygen peroxide, etc.) are better than sterile water or saline solutions to help venous leg ulcers heal.
Simulating wound healing from a growth perspective
Considerable effort has been devoted to understanding the physical relationships governing wound healing and subsequent scarring, with mathematical models and simulations developed to elucidate these relationships. The growth of tissue around the wound site is a result of the migration of cells and collagen deposition by these cells. The alignment of collagen describes the degree of scarring; basket-weave orientation of collagen is characteristic of normal skin, whereas aligned collagen fibers lead to significant scarring. It has been shown that the growth of tissue and extent of scar formation can be controlled by modulating the stress at a wound site.
The growth of tissue can be simulated using the aforementioned relationships from a biochemical and biomechanical point of view. The biologically active chemicals that play an important role in wound healing are modeled with Fickian diffusion to generate concentration profiles. The balance equation for open systems when modeling wound healing incorporates mass growth due to cell migration and proliferation. Here the following equation is used:
Dtρ0 = Div (R) + R0,
where ''ρ'' represents mass density, ''R'' represents a mass flux (from cell migration), and ''R0'' represents a mass source (from cell proliferation, division, or enlargement). Relationships like these can be incorporated into an agent-based model
An agent-based model (ABM) is a computational model for simulating the actions and interactions of autonomous agents (both individual or collective entities such as organizations or groups) in order to understand the behavior of a system and wha ...
s, where the sensitivity to single parameters such as initial collagen alignment, cytokine properties, and cell proliferation rates can be tested.
Wound closure intentions
Successful wound healing is dependent on various cell types, molecular mediators and structural elements.
Primary intention
Primary intention is the healing of a clean wound without tissue loss.bone fracture
A bone fracture (abbreviated FRX or Fx, Fx, or #) is a medical condition in which there is a partial or complete break in the continuity of any bone in the body. In more severe cases, the bone may be broken into several fragments, known as a '' ...
s, healing after flap surgery
Flap surgery is a technique in plastic and reconstructive surgery where any type of tissue is lifted from a donor site and moved to a recipient site with an intact blood supply. This is distinct from a graft, which does not have an intact blood ...
.
* Early removal of dressings from clean or clean-contaminated wounds does affect primary healing of wounds.
Secondary intention
* Secondary intention is implemented when primary intention is not possible because of significant tissue damage or loss, usually due to the wound having been created by major trauma.gingivoplasty
Gingivoplasty is the process by which the gingiva are reshaped to correct deformities. Gingivoplasty is similar to gingivectomy but with a different objective. This is a procedure performed to eliminate periodontal pockets along with the reshaping ...
, tooth extraction sockets, poorly reduced fractures, burns, severe lacerations, pressure ulcers.
* There is insufficient evidence that the choice of dressings or topical agents affects the secondary healing of wounds.
* There is lack of evidence for the effectiveness of negative pressure wound therapy in wound healing by secondary intention.
Tertiary intention
(Delayed primary closure):
* The wound is initially cleaned, debrided and observed, typically 4 or 5 days before closure.
* The wound is purposely left open.
* Examples: healing of wounds by use of tissue graft
Grafting refers to a surgical procedure to move tissue from one site to another on the body, or from another creature, without bringing its own blood supply with it. Instead, a new blood supply grows in after it is placed. A similar technique ...
s.
If the wound edges are not reapproximated immediately, delayed primary wound healing transpires. This type of healing may be desired in the case of contaminated wounds. By the fourth day, phagocytosis of contaminated tissues is well underway, and the processes of epithelization, collagen deposition, and maturation are occurring. Foreign materials are walled off by macrophages that may metamorphose into epithelioid cells, which are encircled by mononuclear leukocytes, forming granulomas. Usually the wound is closed surgically at this juncture, and if the "cleansing" of the wound is incomplete, chronic inflammation can ensue, resulting in prominent scarring.
Overview of involved growth factors
Following are the main growth factors involved in wound healing:
Complications of wound healing
The major complications are many:
# Deficient scar formation: Results in wound dehiscence or rupture of the wound due to inadequate formation of granulation tissue.
# Excessive scar formation: Hypertrophic scar
A hypertrophic scar is a cutaneous condition characterized by deposits of excessive amounts of collagen which gives rise to a raised scar, but not to the degree observed with keloids. Like keloids, they form most often at the sites of pimples, body ...
, keloid
Keloid, also known as keloid disorder and keloidal scar,
is the formation of a type of scar which, depending on its maturity, is composed mainly of either type III (early) or type I (late) collagen. It is a result of an overgrowth of granulation t ...
, desmoid
Aggressive fibromatosis or desmoid tumor is a rare condition. Desmoid tumors arise from cells called fibroblasts, which are found throughout the body and provide structural support, protection to the vital organs, and play a critical role in wou ...
.
# Exuberant granulation (proud flesh
Granulation tissue is new connective tissue and microscopic blood vessels that form on the surfaces of a wound during the healing process. Granulation tissue typically grows from the base of a wound and is able to fill wounds of almost any size ...
).
# Deficient contraction (in skin grafts) or excessive contraction (in burns).
# Others: Dystrophic calcification, pigmentary changes, painful scars, incisional hernia
Other complications can include infection and Marjolin's ulcer
Marjolin's ulcer refers to an aggressive ulcerating squamous cell carcinoma presenting in an area of previously traumatized, chronically inflamed, or scarred skin.Freedberg, et al. (2003). ''Fitzpatrick's Dermatology in General Medicine''. (6th ed ...
.
Biologics, skin substitutes, biomembranes and scaffolds
Advancements in the clinical understanding of wounds and their pathophysiology have commanded significant biomedical innovations in the treatment of acute, chronic, and other types of wounds. Many biologics, skin substitutes, biomembranes and scaffolds have been developed to facilitate wound healing through various mechanisms. This includes a number of products under the trade names such as ''Epicel'', ''Laserskin'', ''Transcyte, Dermagraft, AlloDerm/Strattice, Biobrane, Integra, Apligraf, OrCel, GraftJacket and PermaDerm.''[Vyas KS, Vasconez HC]
Wound Healing: Biologics, Skin Substitutes, Biomembranes and Scaffolds
. Healthcare. 2014; 2(3):356-400.
See also
* Collective cell migration
* Dressing (medical)
A dressing is a sterile pad or compress applied to a wound to promote healing and protect the wound from further harm. A dressing is designed to be in direct contact with the wound, as distinguished from a bandage, which is most often used to hold ...
* History of wound care
The history of wound care spans from prehistory to modern medicine. Wounds naturally heal by themselves, but hunter-gatherers would have noticed several factors and certain herbal remedies would speed up or assist the process, especially if it was ...
* Regeneration in humans
* Wound bed preparation
Wound bed preparation (WBP) is a systematic approach to wound management by identifying and removing barriers to healing. The concept was originally developed in plastic surgery. During the year 2000, the concept was applied to systematizing the t ...
* Wound licking
* Scar free healing
Scar free healing is the process by which significant injuries can heal without permanent damage to the tissue the injury has affected. In most healing, scars form due to the fibrosis and wound contraction, however in scar free healing, tissue is ...
Notes and references
External links
{{Authority control
Healing
Skin physiology
Physiology
Trauma surgery
 The wound healing process is not only complex but fragile, and it is susceptible to interruption or failure leading to the formation of non-healing chronic wounds. Factors that contribute to non-healing chronic wounds are diabetes, venous or arterial disease, infection, and metabolic deficiencies of old age.Enoch, S. Price, P. (2004)
The wound healing process is not only complex but fragile, and it is susceptible to interruption or failure leading to the formation of non-healing chronic wounds. Factors that contribute to non-healing chronic wounds are diabetes, venous or arterial disease, infection, and metabolic deficiencies of old age.Enoch, S. Price, P. (2004)
 As keratinocytes migrate, they move over granulation tissue but stay underneath the scab, thereby separating the scab from the underlying tissue. Epithelial cells have the ability to phagocytize debris such as dead tissue and bacterial matter that would otherwise obstruct their path. Because they must dissolve any scab that forms, keratinocyte migration is best enhanced by a moist environment, since a dry one leads to formation of a bigger, tougher scab. To make their way along the tissue, keratinocytes must dissolve the clot, debris, and parts of the ECM in order to get through. They secrete plasminogen activator, which activates plasminogen, turning it into plasmin to dissolve the scab. Cells can only migrate over living tissue, so they must excrete collagenases and proteases like matrix metalloproteinases (MMPs) to dissolve damaged parts of the ECM in their way, particularly at the front of the migrating sheet. Keratinocytes also dissolve the basement membrane, using instead the new ECM laid down by fibroblasts to crawl across.
As keratinocytes continue migrating, new epithelial cells must be formed at the wound edges to replace them and to provide more cells for the advancing sheet. Proliferation behind migrating keratinocytes normally begins a few days after wounding and occurs at a rate that is 17 times higher in this stage of epithelialization than in normal tissues. Until the entire wound area is resurfaced, the only epithelial cells to proliferate are at the wound edges.
Growth factors, stimulated by integrins and MMPs, cause cells to proliferate at the wound edges. Keratinocytes themselves also produce and secrete factors, including growth factors and basement membrane proteins, which aid both in epithelialization and in other phases of healing. Growth factors are also important for the innate immune defense of skin wounds by stimulation of the production of antimicrobial peptides and neutrophil chemotactic cytokines in keratinocytes.
Keratinocytes continue migrating across the wound bed until cells from either side meet in the middle, at which point contact inhibition causes them to stop migrating. When they have finished migrating, the keratinocytes secrete the proteins that form the new basement membrane. Cells reverse the morphological changes they underwent in order to begin migrating; they reestablish desmosomes and hemidesmosomes and become anchored once again to the basement membrane. Basal cells begin to divide and differentiate in the same manner as they do in normal skin to reestablish the strata found in reepithelialized skin.
As keratinocytes migrate, they move over granulation tissue but stay underneath the scab, thereby separating the scab from the underlying tissue. Epithelial cells have the ability to phagocytize debris such as dead tissue and bacterial matter that would otherwise obstruct their path. Because they must dissolve any scab that forms, keratinocyte migration is best enhanced by a moist environment, since a dry one leads to formation of a bigger, tougher scab. To make their way along the tissue, keratinocytes must dissolve the clot, debris, and parts of the ECM in order to get through. They secrete plasminogen activator, which activates plasminogen, turning it into plasmin to dissolve the scab. Cells can only migrate over living tissue, so they must excrete collagenases and proteases like matrix metalloproteinases (MMPs) to dissolve damaged parts of the ECM in their way, particularly at the front of the migrating sheet. Keratinocytes also dissolve the basement membrane, using instead the new ECM laid down by fibroblasts to crawl across.
As keratinocytes continue migrating, new epithelial cells must be formed at the wound edges to replace them and to provide more cells for the advancing sheet. Proliferation behind migrating keratinocytes normally begins a few days after wounding and occurs at a rate that is 17 times higher in this stage of epithelialization than in normal tissues. Until the entire wound area is resurfaced, the only epithelial cells to proliferate are at the wound edges.
Growth factors, stimulated by integrins and MMPs, cause cells to proliferate at the wound edges. Keratinocytes themselves also produce and secrete factors, including growth factors and basement membrane proteins, which aid both in epithelialization and in other phases of healing. Growth factors are also important for the innate immune defense of skin wounds by stimulation of the production of antimicrobial peptides and neutrophil chemotactic cytokines in keratinocytes.
Keratinocytes continue migrating across the wound bed until cells from either side meet in the middle, at which point contact inhibition causes them to stop migrating. When they have finished migrating, the keratinocytes secrete the proteins that form the new basement membrane. Cells reverse the morphological changes they underwent in order to begin migrating; they reestablish desmosomes and hemidesmosomes and become anchored once again to the basement membrane. Basal cells begin to divide and differentiate in the same manner as they do in normal skin to reestablish the strata found in reepithelialized skin.