Pediatric Advanced Life Support on:
[Wikipedia]
[Google]
[Amazon]
Pediatric advanced life support (PALS) is a course offered by the
 PALS builds upon AHA's Pediatric
PALS builds upon AHA's Pediatric
AHA's Pediatric BLS Algorithms
for single and ≥ 2 person rescuer. The most essential component of BLS and PALS cardiac arrest care is high quality If help hasn't arrived after 2 minutes, the provider should call for help again and get an
If help hasn't arrived after 2 minutes, the provider should call for help again and get an
 Breathing
* monitor oxygen saturation with a pulse ox
* give supplemental oxygen
* give inhaled medications (e.g.,
Breathing
* monitor oxygen saturation with a pulse ox
* give supplemental oxygen
* give inhaled medications (e.g.,
 Advanced airways may be necessary if the child can't maintain their airway on their own and isn't responding to other methods of ventilation and oxygenation. Advanced airways use medical equipment to allow for open airways and ease of ventilation and medication delivery. Types of advanced airways include supraglottic devices (devices that lie above the
Advanced airways may be necessary if the child can't maintain their airway on their own and isn't responding to other methods of ventilation and oxygenation. Advanced airways use medical equipment to allow for open airways and ease of ventilation and medication delivery. Types of advanced airways include supraglottic devices (devices that lie above the

 *
*  *
*
 Treatment of pediatric cardiac arrest follows the American Heart Association's (AHA) Pediatric Cardiac Arrest Algorithm. The goals of treatment are to obtain
Treatment of pediatric cardiac arrest follows the American Heart Association's (AHA) Pediatric Cardiac Arrest Algorithm. The goals of treatment are to obtain  Once cardiac arrest is recognized, high quality
Once cardiac arrest is recognized, high quality
 Types of bradyarrhythmias
*
Types of bradyarrhythmias
*
 sinus tachycardia: normal rhythm (normal p waves), fast rate, heart rate usually < 220 bpm (beats per minute) in infants and < 180 bpm in kids
* supraventricular tachycardia (SVT): abnormal rhythm (abnormal p waves), fast rate, originates above the ventricles, heart rate usually > 220 bpm in infants and > 180 bpm in kids, narrow QRS (< 0.09 seconds)
* ventricular tachycardia (VT): fast rate, originates in the ventricles, wide QRS (> 0.09 seconds)
sinus tachycardia: normal rhythm (normal p waves), fast rate, heart rate usually < 220 bpm (beats per minute) in infants and < 180 bpm in kids
* supraventricular tachycardia (SVT): abnormal rhythm (abnormal p waves), fast rate, originates above the ventricles, heart rate usually > 220 bpm in infants and > 180 bpm in kids, narrow QRS (< 0.09 seconds)
* ventricular tachycardia (VT): fast rate, originates in the ventricles, wide QRS (> 0.09 seconds)
American Heart Association
Pediatric Advanced Life Support Course -- PALS
{{Emergency medicine Medical credentials Emergency medicine courses Emergency life support Pediatrics
American Heart Association
The American Heart Association (AHA) is a nonprofit organization in the United States that funds cardiovascular medical research, educates consumers on healthy living and fosters appropriate Heart, cardiac care in an effort to reduce disability ...
(AHA) for health care providers who take care of children and infants in the emergency room
An emergency department (ED), also known as an accident and emergency department (A&E), emergency room (ER), emergency ward (EW) or casualty department, is a medical treatment facility specializing in emergency medicine, the acute care of pat ...
, critical care and intensive care unit
An intensive care unit (ICU), also known as an intensive therapy unit or intensive treatment unit (ITU) or critical care unit (CCU), is a special department of a hospital or health care facility that provides intensive care medicine.
An inten ...
s in the hospital, and out of hospital (emergency medical services
Emergency medical services (EMS), also known as ambulance services, pre-hospital care or paramedic services, are emergency services that provide urgent pre-hospital treatment and stabilisation for serious illness and injuries and transport to d ...
(EMS)). The course teaches healthcare providers how to assess injured and sick children and recognize and treat respiratory distress/failure, shock, cardiac arrest, and arrhythmias.
Basic Life Support (BLS)
 PALS builds upon AHA's Pediatric
PALS builds upon AHA's Pediatric Basic Life Support
Basic life support (BLS) is a level of medical care which is used for patients with life-threatening condition of cardiac arrest until they can be given full medical care by advanced life support providers (paramedics, nurses, physicians or any ...
(BLS). Providers should follow thAHA's Pediatric BLS Algorithms
for single and ≥ 2 person rescuer. The most essential component of BLS and PALS cardiac arrest care is high quality
cardiopulmonary resuscitation
Cardiopulmonary resuscitation (CPR) is an emergency procedure used during Cardiac arrest, cardiac or Respiratory arrest, respiratory arrest that involves chest compressions, often combined with artificial ventilation, to preserve brain function ...
(CPR). CPR should begin with a check for responsiveness, getting help, and activating the emergency response system. After this, the provider should assess for breathing and a pulse ( brachial pulse in infant and carotid pulse in child) - all within 10 seconds. If no pulse and no breathing or only gasping, start CPR. CPR consists of chest compressions followed by rescue breaths - for single rescuer do 30 compressions and 2 breaths (30:2), for > 2 rescuers do 15 compressions and 2 breaths (15:2). The rate of chest compressions should be 100-120 compressions/min and depth should be 1.5 inches for infants and 2 inches for children.
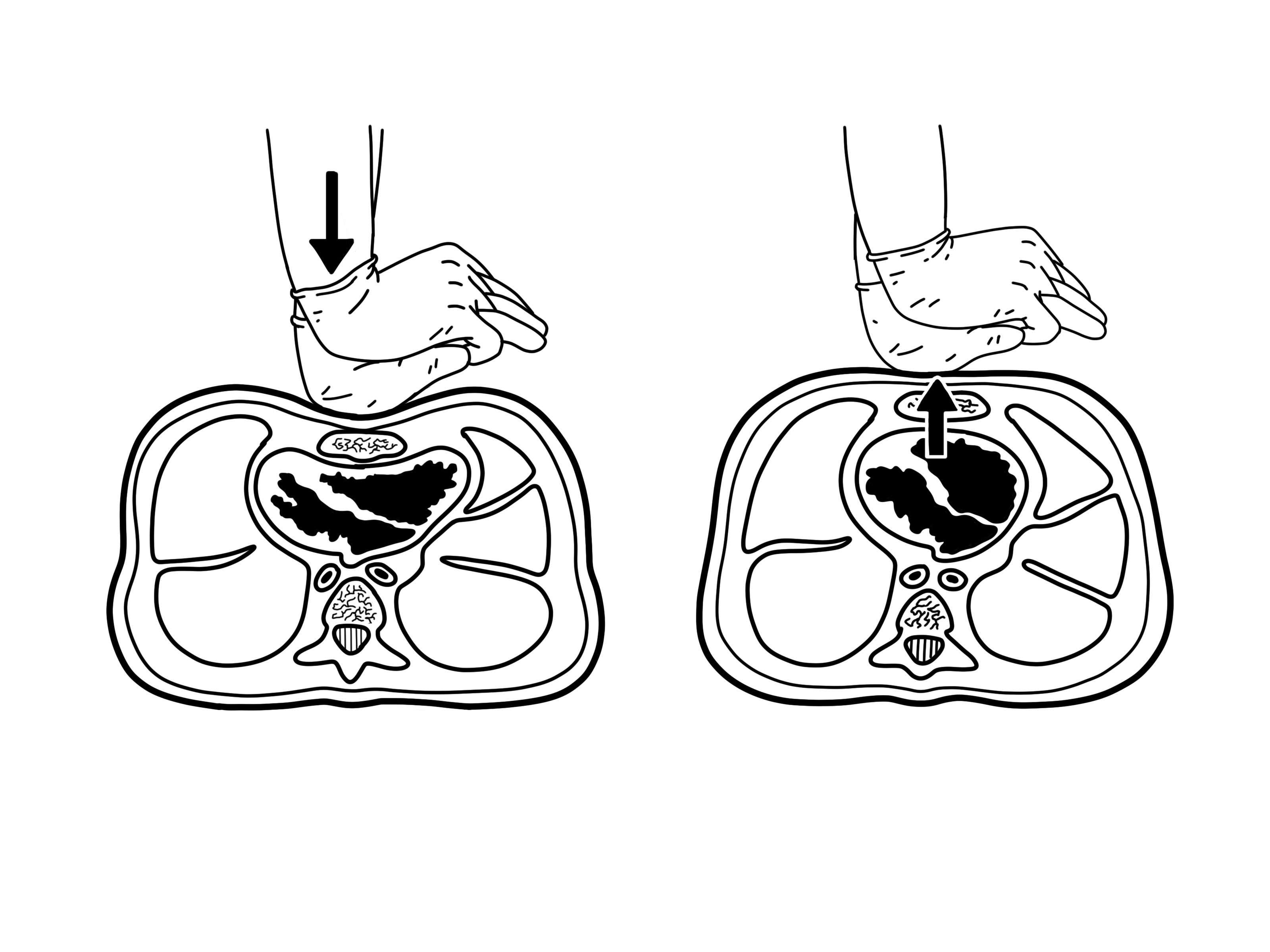
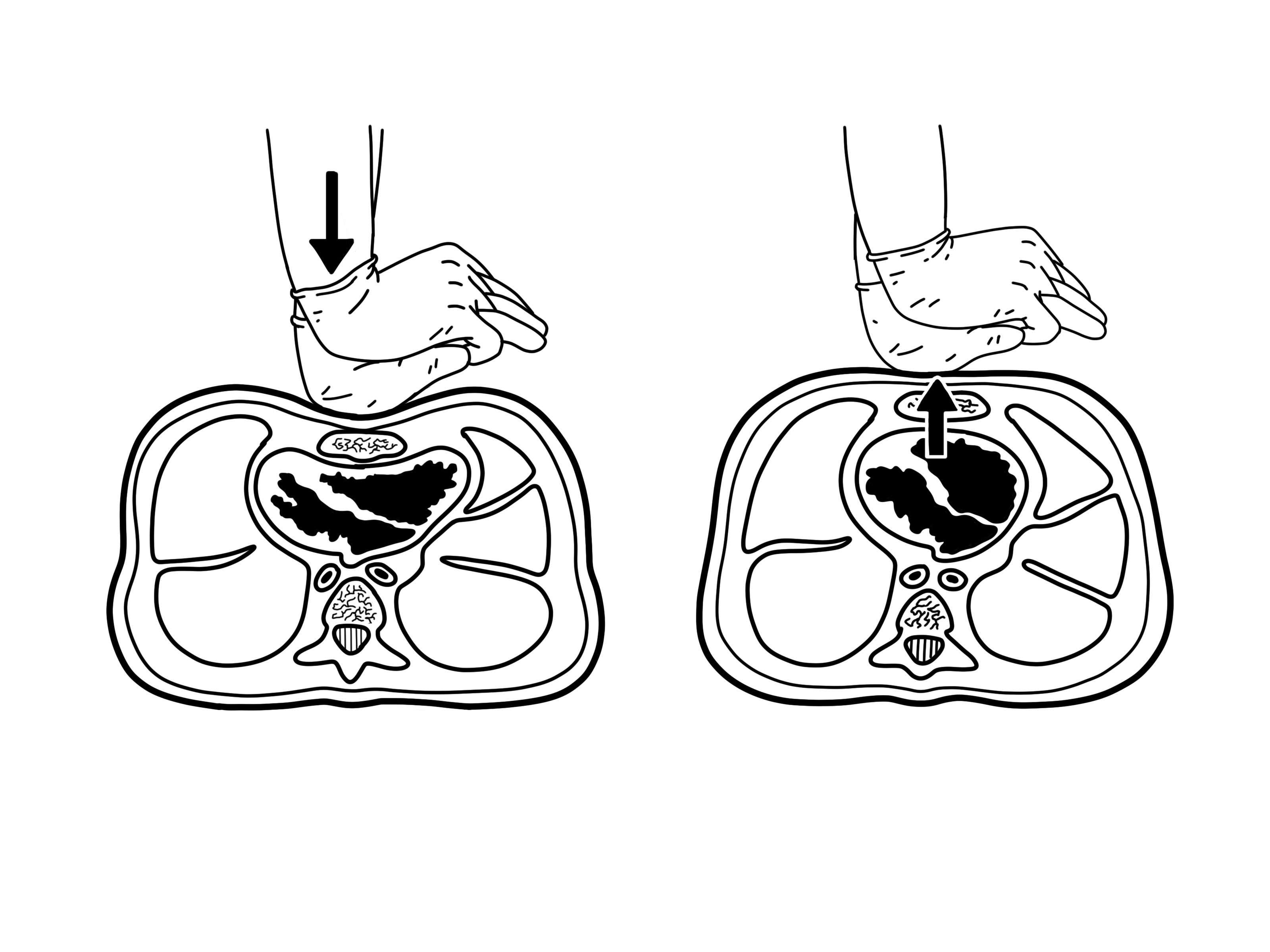
Chest compressions differ between infants and children. For infants, chest compressions can be done with the two-fingers technique (single rescuer) or two-thumbs encircling hands technique (2 rescuer). In the two-fingers technique, the provider uses their index and middle finger to press down on the infant's sternum
The sternum (: sternums or sterna) or breastbone is a long flat bone located in the central part of the chest. It connects to the ribs via cartilage and forms the front of the rib cage, thus helping to protect the heart, lungs, and major bl ...
, below the nipples. In the two-thumb encircling hands technique, the provider's hands should wrap around the chest with both thumbs pressing down on the infant's sternum. For children, chest compressions should be done with the provider placing the heel of one hand over the child's lower chest and pressing down while keeping their arms straightened at the elbow.
 If help hasn't arrived after 2 minutes, the provider should call for help again and get an
If help hasn't arrived after 2 minutes, the provider should call for help again and get an automated external defibrillator
An automated external defibrillator (AED) is a portable electronic device that automatically diagnoses the life-threatening cardiac Heart arrhythmia, arrhythmias of ventricular fibrillation (VF) and pulseless ventricular tachycardia, and is able ...
(AED). Once help and the AED arrives, the provider should place the AED pads on the child, making sure to not disrupt chest compressions. The AED will let the provider know if the child has a shockable heart rhythm
''Heart Rhythm'' is a peer-reviewed medical journal published by Elsevier that covers the study and management of cardiac arrhythmia. It is the official journal of the Heart Rhythm Society, the Cardiac Electrophysiology Society, and thPediatric & ...
. If shockable, give a shock
Shock may refer to:
Common uses
Healthcare
* Acute stress reaction, also known as psychological or mental shock
** Shell shock, soldiers' reaction to battle trauma
* Circulatory shock, a medical emergency
** Cardiogenic shock, resulting from ...
and then immediately resume CPR.
Assessment
PALS teaches a systematic assessment approach so that the health care provider can quickly identify any life-threatening conditions and treat them. The PALS systematic approach algorithm begins with a quick initial assessment followed by checking for responsiveness, pulse, and breathing. If the child has no pulse and isn't breathing, startCPR
Cardiopulmonary resuscitation (CPR) is an emergency procedure used during cardiac or respiratory arrest that involves chest compressions, often combined with artificial ventilation, to preserve brain function and maintain circulation until sp ...
. If the child has a pulse but isn't breathing, provide ventilation
Ventilation may refer to:
* Ventilation (physiology), the movement of air between the environment and the lungs via inhalation and exhalation
** Mechanical ventilation, in medicine, using artificial methods to assist breathing
*** Respirator, a ma ...
and give oxygen (when possible). Once it has been established that the child has a pulse, is breathing, and doesn't require immediate life saving treatment, the provider will begin their primary assessment followed by a secondary assessment and further diagnostic workup. Continuous reassessments should be done to reassess for life-threatening conditions.
Pediatric vitals signs range according to age
Initial assessment
The initial assessment is meant to be a very quick assessment performed within the first few seconds of interacting with a child and it utilizes the acronym ABC - appearance, breathing, and color. The provider will assess appearance (level of consciousness and responsiveness, speaking or crying), breathing (breathing or not breathing, increased work of breathing, abnormal breath sounds), and color (pale, mottled,cyanotic
Cyanosis is the change of tissue color to a bluish-purple hue, as a result of decrease in the amount of oxygen bound to the hemoglobin in the red blood cells of the capillary bed. Cyanosis is apparent usually in the body tissues covered with ...
, bleeding).
Primary assessment
The primary assessment uses the acronym ABCDE - airway, breathing, circulation, disability, exposure. Airway - assess airway patency (open/patent, unobstructed vs obstructed) and if the patient will need assistance maintaining their airway Breathing - assess respiratory rate, respiratory effort, lung sounds, airway sounds, chest movement,oxygen saturation
Oxygen saturation (symbol SO2) is a relative measure of the concentration of oxygen that is Dissolution (chemistry), dissolved or carried in a given medium as a proportion of the maximal concentration that can be dissolved in that medium at the g ...
via pulse oximetry
Pulse oximetry is a noninvasive method for monitoring blood oxygen saturation. Peripheral oxygen saturation (SpO2) readings are typically within 2% accuracy (within 4% accuracy in 95% of cases) of the more accurate (and invasive) reading of art ...
Circulation - assess heart rate, heart rhythm, pulses, skin color, skin temperature, capillary refill
Capillary refill time (CRT) is defined as the time taken for color to return to an external capillary bed after pressure is applied to cause blanching. It can be measured by holding a hand higher than heart-level and pressing the soft pad of a ...
time, blood pressure
Blood pressure (BP) is the pressure of Circulatory system, circulating blood against the walls of blood vessels. Most of this pressure results from the heart pumping blood through the circulatory system. When used without qualification, the term ...
Disability - assess neurological function with AVPU pediatric response scale (alert, voice, painful, unresponsive), pediatric Glasgow Coma Scale
The Glasgow Coma Scale (GCS) is a clinical scale used to reliably measure a person's level of consciousness after a brain injury.
The GCS assesses a person based on their ability to perform eye movements, speak, and move their body. These th ...
(eye opening, motor response, verbal response), pupil response to light (normal, pinpoint, dilated, unilateral dilated), blood glucose test (low blood sugar / hypoglycemia
Hypoglycemia (American English), also spelled hypoglycaemia or hypoglycæmia (British English), sometimes called low blood sugar, is a fall in blood sugar to levels below normal, typically below 70 mg/dL (3.9 mmol/L). Whipple's tria ...
can cause altered mental status
An altered level of consciousness is any measure of arousal other than normal. Level of consciousness (LOC) is a measurement of a person's arousability and responsiveness to stimuli from the environment.
A mildly depressed level of consciousne ...
)
Exposure - assess temperature/ fever, signs of trauma (cuts, bleeding, bruises, burns, etc.), skin (petechia
A petechia (; : petechiae) is a small red or purple spot ( 1 cm in diameter) and purpura (3 to 10 mm in diameter). The term is typically used in the plural (petechiae), since a single petechia is seldom noticed or significant.
Causes Physical t ...
e, purpura
Purpura () is a condition of red or purple discolored spots on the skin that do not blanch on applying pressure. The spots are caused by bleeding underneath the skin secondary to platelet disorders, vascular disorders, coagulation disorders, ...
, etc.)
Secondary assessment
Once the primary assessment is completed, the provider can do a secondary assessment which consists of a completephysical exam
In a physical examination, medical examination, clinical examination, or medical checkup, a medical practitioner examines a patient for any possible medical signs or symptoms of a medical condition. It generally consists of a series of questions ...
and focused medical history
The medical history, case history, or anamnesis (from Greek: ἀνά, ''aná'', "open", and μνήσις, ''mnesis'', "memory") of a patient is a set of information the physicians collect over medical interviews. It involves the patient, and ev ...
. The information asked in the medical history uses the acronym SAMPLE - signs and symptoms
Signs and symptoms are diagnostic indications of an illness, injury, or condition.
Signs are objective and externally observable; symptoms are a person's reported subjective experiences.
A sign for example may be a higher or lower temperature ...
, allergies, medications (prescribed, over the counter, vitamins, herbal), past medical history (any medical problems, prior surgeries), last meal (helpful information to know because it can affect when a child can have surgery or receive anesthesia
Anesthesia (American English) or anaesthesia (British English) is a state of controlled, temporary loss of sensation or awareness that is induced for medical or veterinary purposes. It may include some or all of analgesia (relief from or prev ...
), events (onset of illness and events leading up to illness).
Parts of the history that are especially important for children include asking about medications that the child could have gotten into (e.g., if a pill fell on the floor or an unlocked medicine cabinet), history of prematurity, birth history, and immunizations
Immunization, or immunisation, is the process by which an individual's immune system becomes fortified against an infectious agent (known as the immunogen). When this system is exposed to molecules that are foreign to the body, called ''non-sel ...
.
Respiratory distress and failure
Providers must be able to identify respiratory problems that are easily treatable (e.g., treated with oxygen, suctioning/ clearing airway,albuterol
Salbutamol, also known as albuterol and sold under the brand name Ventolin among others, is a medication that opens up the medium and large airways in the lungs. It is a short-acting β2 adrenergic receptor agonist that causes relaxation of ...
, etc.) and those that can rapidly progress to life-threatening conditions. Respiratory distress can progress to respiratory failure which can progress to cardiac arrest
Cardiac arrest (also known as sudden cardiac arrest CA is when the heart suddenly and unexpectedly stops beating. When the heart stops beating, blood cannot properly Circulatory system, circulate around the body and the blood flow to the ...
. Once respiratory complaints have progressed to cardiac arrest
Cardiac arrest (also known as sudden cardiac arrest CA is when the heart suddenly and unexpectedly stops beating. When the heart stops beating, blood cannot properly Circulatory system, circulate around the body and the blood flow to the ...
, death and neurological damage are more likely to occur. For this reason, providers should aim to identify and treat respiratory conditions before they progress and worsen.
Recognition
Signs and symptoms
Common signs of respiratory distress * increased work of breathing * nasal flaring (nostrils widening during breathing) * accessory muscle use (using muscles other than the diaphragm andintercostal muscles
The intercostal muscles comprise many different groups of muscles that run between the ribs, and help form and move the chest wall. The intercostal muscles are mainly involved in the mechanical aspect of breathing by helping expand and shrink th ...
during breathing (e.g., sternocleidomastoid
The sternocleidomastoid muscle is one of the largest and most superficial cervical muscles. The primary actions of the muscle are rotation of the head to the opposite side and flexion of the neck. The sternocleidomastoid is innervated by the acces ...
))
* retractions (collapse of parts of the chest during breathing) (e.g., suprasternal, substernal, sternal, intercostal, subcostal, supraclavicular)
* head bobbing (in infants)
* grunting
* tachypnea
Tachypnea, also spelt tachypnoea, is a respiratory rate greater than normal, resulting in abnormally rapid and shallow breathing.
In adult humans at rest, any respiratory rate of 1220 per minute is considered clinically normal, with tachypnea b ...
(too fast breathing)
* pallor (pale skin)
* tachycardia
Tachycardia, also called tachyarrhythmia, is a heart rate that exceeds the normal resting rate. In general, a resting heart rate over 100 beats per minute is accepted as tachycardia in adults. Heart rates above the resting rate may be normal ...
(fast heart rate)
* agitation and anxiety
Respiratory distress can progress and worsen to respiratory failure. Signs of respiratory failure include the following
* decreased work of breathing
* eventual pauses in or altogether stopping breathing (apnea)
* bradypnea
Bradypnea is abnormally slow breathing. The respiratory rate at which bradypnea is diagnosed depends on the age of the person, with the limit being higher during childhood.
Signs and symptoms
Symptoms of bradypnea may include:
*Dizziness
*Near ...
(too slow breathing)
* decreased or absent air movement
* abnormal breath sounds
* cyanosis
Cyanosis is the change of Tissue (biology), tissue color to a bluish-purple hue, as a result of decrease in the amount of oxygen bound to the hemoglobin in the red blood cells of the capillary bed. Cyanosis is apparent usually in the Tissue (bi ...
(blue skin)
* exhaustion and unresponsiveness
* can't speak or cough
Types of respiratory problems
* upper airway obstruction - e.g.,croup
Croup ( ), also known as croupy cough, is a type of respiratory infection that is usually caused by a virus. The infection leads to swelling inside the trachea, which interferes with normal breathing and produces the classic symptoms of "bar ...
, epiglottitis, foreign body aspiration
Foreign body aspiration occurs when a foreign body enters the Respiratory tract, airway which can cause difficulty breathing or choking. Objects may reach the respiratory tract and the digestive tract from the mouth and nose, but when an object ent ...
, anaphylaxis
Anaphylaxis (Greek: 'up' + 'guarding') is a serious, potentially fatal allergic reaction and medical emergency that is rapid in onset and requires immediate medical attention regardless of the use of emergency medication on site. It typicall ...
, retropharyngeal abscess, enlarged/swollen tonsil
The tonsils ( ) are a set of lymphoid organs facing into the aerodigestive tract, which is known as Waldeyer's tonsillar ring and consists of the adenoid tonsil (or pharyngeal tonsil), two tubal tonsils, two palatine tonsils, and the lingual t ...
s
* lower airway obstruction - e.g., asthma
Asthma is a common long-term inflammatory disease of the airways of the lungs. It is characterized by variable and recurring symptoms, reversible airflow obstruction, and easily triggered bronchospasms. Symptoms include episodes of wh ...
, bronchiolitis
Bronchiolitis is inflammation of the small airways also known as the bronchioles in the lungs. Acute bronchiolitis is caused by a viral infection, usually affecting children younger than two years of age. Symptoms may include fever, cough, run ...
* lung tissue disease - e.g., pneumonia
Pneumonia is an Inflammation, inflammatory condition of the lung primarily affecting the small air sacs known as Pulmonary alveolus, alveoli. Symptoms typically include some combination of Cough#Classification, productive or dry cough, ches ...
, pneumonitis
Pneumonitis describes general inflammation of lung tissue. Possible causative agents include radiation therapy of the chest, exposure to medications used during chemo-therapy, the inhalation of debris (e.g., animal dander), aspiration, herbicide ...
, pulmonary edema
Pulmonary edema (British English: oedema), also known as pulmonary congestion, is excessive fluid accumulation in the tissue or air spaces (usually alveoli) of the lungs. This leads to impaired gas exchange, most often leading to shortness ...
* disordered control of breathing - often described as "breathing funny"; e.g., seizure
A seizure is a sudden, brief disruption of brain activity caused by abnormal, excessive, or synchronous neuronal firing. Depending on the regions of the brain involved, seizures can lead to changes in movement, sensation, behavior, awareness, o ...
, overdose
A drug overdose (overdose or OD) is the ingestion or application of a drug or other substance in quantities much greater than are recommended. Retrieved on September 20, 2014.
, trauma, coma
A coma is a deep state of prolonged unconsciousness in which a person cannot be awakened, fails to Nociception, respond normally to Pain, painful stimuli, light, or sound, lacks a normal Circadian rhythm, sleep-wake cycle and does not initiate ...
, neuromuscular disease
A neuromuscular disease is any disease affecting the peripheral nervous system (PNS), the neuromuscular junctions, or skeletal muscles, all of which are components of the motor unit. Damage to any of these structures can cause muscle atrophy and we ...
s
Management
Initial management
The initial management for respiratory distress uses the acronym ABC - airway, breathing, circulation. Airway * support the airway by making sure that it is open/patent (child can do this on their own or provider may have to open airway with head tilt-chin lift orjaw thrust
The jaw-thrust maneuver is a first aid and medical procedure used to prevent the tongue from obstructing the upper airways. This maneuver and the head-tilt/chin-lift maneuver are two of the main tools of basic airway management, and they a ...
(if suspected cervical spine injury))
* clear the airway as needed (e.g., suctioning mucus/secretions in nose and throat, removing foreign bodies, etc.)
* consider adding airway adjuncts such as nasopharyngeal airway (NPA) or oropharyngeal airway
An oropharyngeal airway (also known as an oral airway, OPA or Guedel pattern airway) is a medical device called an ''airway adjunct'' used in airway management to maintain or open a patient's airway. It does this by preventing the tongue from cov ...
(OPA) (if no gag reflex)albuterol
Salbutamol, also known as albuterol and sold under the brand name Ventolin among others, is a medication that opens up the medium and large airways in the lungs. It is a short-acting β2 adrenergic receptor agonist that causes relaxation of ...
, epinephrine
Adrenaline, also known as epinephrine, is a hormone and medication which is involved in regulating visceral functions (e.g., respiration). It appears as a white microcrystalline granule. Adrenaline is normally produced by the adrenal glands a ...
) as needed
* manually ventilate as needed (e.g., bag mask ventilation)
* prepare for advanced airway
Circulation
* monitor vitals (e.g., heart rate
Heart rate is the frequency of the cardiac cycle, heartbeat measured by the number of contractions of the heart per minute (''beats per minute'', or bpm). The heart rate varies according to the body's Human body, physical needs, including the nee ...
, blood pressure
Blood pressure (BP) is the pressure of Circulatory system, circulating blood against the walls of blood vessels. Most of this pressure results from the heart pumping blood through the circulatory system. When used without qualification, the term ...
)
* establish vascular access (for medications and fluids) as needed
Advanced airways
 Advanced airways may be necessary if the child can't maintain their airway on their own and isn't responding to other methods of ventilation and oxygenation. Advanced airways use medical equipment to allow for open airways and ease of ventilation and medication delivery. Types of advanced airways include supraglottic devices (devices that lie above the
Advanced airways may be necessary if the child can't maintain their airway on their own and isn't responding to other methods of ventilation and oxygenation. Advanced airways use medical equipment to allow for open airways and ease of ventilation and medication delivery. Types of advanced airways include supraglottic devices (devices that lie above the glottis
The glottis (: glottises or glottides) is the opening between the vocal folds (the rima glottidis). The glottis is crucial in producing sound from the vocal folds.
Etymology
From Ancient Greek ''γλωττίς'' (glōttís), derived from ''γ ...
such as OPA, NPA, laryngeal mask airway), infraglottic devices (devices that lie below the glottis and go into the trachea
The trachea (: tracheae or tracheas), also known as the windpipe, is a cartilaginous tube that connects the larynx to the bronchi of the lungs, allowing the passage of air, and so is present in almost all animals' lungs. The trachea extends from ...
such as endotracheal tube
A tracheal tube is a catheter that is inserted into the trachea for the primary purpose of establishing and maintaining a patent airway and to ensure the adequate exchange of oxygen and carbon dioxide.
Many different types of tracheal tubes are a ...
(intubation
Intubation (sometimes entubation) is a medical procedure involving the insertion of a tube into the body. Most commonly, intubation refers to tracheal intubation, a procedure during which an endotracheal tube is inserted into the trachea to supp ...
)), and surgery (incision below the glottis such as cricothyrotomy
A cricothyrotomy (also called cricothyroidotomy or laryngotomy) is a medical procedure where an opening is created through the cricothyroid membrane to establish a patent airway during emergency airway management. Cricothyrotomy is primarily per ...
and tracheotomy
Tracheotomy (, ), or tracheostomy, is a surgical airway management procedure which consists of making an incision on the front of the neck to open a direct airway to the trachea. The resulting stoma (hole) can serve independently as an airway ...
). Surgical advanced airways are typically performed when intubation and other less invasive methods fail or are contraindicated or when the child will need long term mechanical ventilation
Mechanical ventilation or assisted ventilation is the Medicine, medical term for using a ventilator, ventilator machine to fully or partially provide artificial ventilation. Mechanical ventilation helps move air into and out of the lungs, wit ...
.
Intubation
To perform an intubation, the health care provider should be able to perform the steps of rapid sequence intubation (preparation, preoxygenation, pretreatment, paralysis and sedation, positioning, placement of tube, postintubation management).Further management
Further management should be based on the specific medical condition the child has. For example, if the child is experiencing respiratory distress secondary toasthma
Asthma is a common long-term inflammatory disease of the airways of the lungs. It is characterized by variable and recurring symptoms, reversible airflow obstruction, and easily triggered bronchospasms. Symptoms include episodes of wh ...
, management would include albuterol
Salbutamol, also known as albuterol and sold under the brand name Ventolin among others, is a medication that opens up the medium and large airways in the lungs. It is a short-acting β2 adrenergic receptor agonist that causes relaxation of ...
, inhaled corticosteroids, supplemental oxygen
Oxygen is a chemical element; it has chemical symbol, symbol O and atomic number 8. It is a member of the chalcogen group (periodic table), group in the periodic table, a highly reactivity (chemistry), reactive nonmetal (chemistry), non ...
, and more depending upon the severity of the asthma.
Shock
Shock
Shock may refer to:
Common uses
Healthcare
* Acute stress reaction, also known as psychological or mental shock
** Shell shock, soldiers' reaction to battle trauma
* Circulatory shock, a medical emergency
** Cardiogenic shock, resulting from ...
is defined as inadequate blood flow (perfusion
Perfusion is the passage of fluid through the circulatory system or lymphatic system to an organ (anatomy), organ or a tissue (biology), tissue, usually referring to the delivery of blood to a capillary bed in tissue. Perfusion may also refer t ...
) in the body, causing tissues and organs to (1) not get enough oxygen and nutrients and (2) have trouble getting rid of toxic products of metabolism (e.g., lactate). It is important to recognize and treat shock as early as possible because the body requires oxygen and nutrients to function and without them, organs can eventually shut down and people can die. Common signs of shock include weak pulses, altered mental status
An altered level of consciousness is any measure of arousal other than normal. Level of consciousness (LOC) is a measurement of a person's arousability and responsiveness to stimuli from the environment.
A mildly depressed level of consciousne ...
, bradycardia
Bradycardia, also called bradyarrhythmia, is a resting heart rate under 60 beats per minute (BPM). While bradycardia can result from various pathological processes, it is commonly a physiological response to cardiovascular conditioning or due ...
or tachycardia
Tachycardia, also called tachyarrhythmia, is a heart rate that exceeds the normal resting rate. In general, a resting heart rate over 100 beats per minute is accepted as tachycardia in adults. Heart rates above the resting rate may be normal ...
, low urine output, hypotension
Hypotension, also known as low blood pressure, is a cardiovascular condition characterized by abnormally reduced blood pressure. Blood pressure is the force of blood pushing against the walls of the arteries as the heart pumps out blood and is ...
, and pale, cold skin. Treating shock focuses on increasing blood flow and oxygen delivery to tissues and organs before organs are permanently damaged. This section will discuss the recognition and management of shock.
Recognition
Shock severity
The severity of shock is typically based onsystolic blood pressure
Blood pressure (BP) is the pressure of circulating blood against the walls of blood vessels. Most of this pressure results from the heart pumping blood through the circulatory system. When used without qualification, the term "blood pressure" r ...
. For this reason, measuring blood pressure is an important way to assess shock; however, blood pressure machines may not be very accurate if pulses are weak and the arms and legs (where the blood pressure is measured) are poorly perfused.
Compensated shock is when the body is able to compensate through various mechanisms (e.g., raising the heart rate, increasing systemic vascular resistance, and more) to keep the systolic blood pressure in a normal range.
Hypotensive/ decompensated shock is when the body cannot maintain systolic blood pressure in the normal range, and it becomes too low (hypotensive
Hypotension, also known as low blood pressure, is a cardiovascular condition characterized by abnormally reduced blood pressure. Blood pressure is the force of blood pushing against the walls of the arteries as the heart pumps out blood and is ...
).
Types of shock
There are 4 main types of shock: hypovolemic, distributive, cardiogenic, and obstructive.Hypovolemic shock
Hypovolemic shock
Hypovolemic shock is a form of Shock (circulatory), shock caused by severe hypovolemia (insufficient blood volume or extracellular fluid in the body). It can be caused by severe dehydration or blood loss. Hypovolemic shock is a medical emergency ...
is caused by low blood volume (hypovolemia) and is the most common cause of shock in pediatric patients. Common causes of volume loss include diarrhea
Diarrhea (American English), also spelled diarrhoea or diarrhœa (British English), is the condition of having at least three loose, liquid, or watery bowel movements in a day. It often lasts for a few days and can result in dehydration d ...
, vomiting, hemorrhage
Bleeding, hemorrhage, haemorrhage or blood loss, is blood escaping from the circulatory system from damaged blood vessels. Bleeding can occur internally, or externally either through a natural opening such as the mouth, nose, ear, urethra, ...
, not drinking enough, burns, osmotic diuresis (e.g., diabetic ketoacidosis
Diabetic ketoacidosis (DKA) is a potentially life-threatening acute complication of diabetes mellitus. Signs and symptoms may include vomiting, abdominal pain, deep gasping breathing, increased urination, weakness, confusion and occasionally ...
), and third space losses. Signs of hypovolemic shock are related to the low blood volume and decreased blood flow to extremities (e.g., cold extremities, slow capillary refill
Capillary refill time (CRT) is defined as the time taken for color to return to an external capillary bed after pressure is applied to cause blanching. It can be measured by holding a hand higher than heart-level and pressing the soft pad of a ...
, and weak distal pulses).
Distributive shock
Distributive shock is caused by abnormally distributed blood throughout the body which causes some parts of the body to receive inadequate blood supply. Common causes of distributive shock includesepsis
Sepsis is a potentially life-threatening condition that arises when the body's response to infection causes injury to its own tissues and organs.
This initial stage of sepsis is followed by suppression of the immune system. Common signs and s ...
, anaphylaxis
Anaphylaxis (Greek: 'up' + 'guarding') is a serious, potentially fatal allergic reaction and medical emergency that is rapid in onset and requires immediate medical attention regardless of the use of emergency medication on site. It typicall ...
, and head or spinal cord injury (neurogenic shock
Neurogenic shock is a distributive type of shock resulting in hypotension (low blood pressure), often with bradycardia (slowed heart rate), caused by disruption of autonomic nervous system pathways. It can occur after damage to the central nerv ...
).
* Septic shock is typically caused by an infection or inflammation in the body. Signs of septic shock include fever
Fever or pyrexia in humans is a symptom of an anti-infection defense mechanism that appears with Human body temperature, body temperature exceeding the normal range caused by an increase in the body's temperature Human body temperature#Fever, s ...
or hypothermia
Hypothermia is defined as a body core temperature below in humans. Symptoms depend on the temperature. In mild hypothermia, there is shivering and mental confusion. In moderate hypothermia, shivering stops and confusion increases. In severe ...
, petechia
A petechia (; : petechiae) is a small red or purple spot ( 1 cm in diameter) and purpura (3 to 10 mm in diameter). The term is typically used in the plural (petechiae), since a single petechia is seldom noticed or significant.
Causes Physical t ...
, and purpura
Purpura () is a condition of red or purple discolored spots on the skin that do not blanch on applying pressure. The spots are caused by bleeding underneath the skin secondary to platelet disorders, vascular disorders, coagulation disorders, ...
. Lab tests might show leukocytosis
Leukocytosis is a condition in which the white cell (leukocyte) count is above the normal range in the blood. It is frequently a sign of an inflammatory response, most commonly the result of infection, but may also occur following certain parasit ...
or leukopenia
Leukopenia () is a decrease in the number of white blood cells (leukocytes). It places individuals at increased risk of infection as white blood cells are the body's primary defense against infections.
Signs and symptoms
Symptoms may include:
* s ...
, metabolic acidosis
Metabolic acidosis is a serious electrolyte disorder characterized by an imbalance in the body's acid-base balance. Metabolic acidosis has three main root causes: increased acid production, loss of bicarbonate, and a reduced ability of the kidn ...
with high lactate, and more.
* Anaphylactic shock is caused by an allergen
An allergen is an otherwise harmless substance that triggers an allergic reaction in sensitive individuals by stimulating an immune response.
In technical terms, an allergen is an antigen that is capable of stimulating a type-I hypersensitivi ...
and common signs include facial swelling, throat swelling, hives
Hives, also known as urticaria, is a kind of skin rash with red or flesh-colored, raised, itchy bumps. Hives may burn or sting. The patches of rash may appear on different body parts, with variable duration from minutes to days, and typically ...
, wheezing
A wheeze is a clinical symptom of a continuous, coarse, whistling sound produced in the respiratory airways during breathing. For wheezes to occur, part of the respiratory tree must be narrowed or obstructed (for example narrowing of the lower ...
, etc.
Cardiogenic shock
Cardiogenic shock
Cardiogenic shock is a medical emergency resulting from inadequate blood flow to the body's organs due to the dysfunction of the heart. Signs of inadequate blood flow include low urine production (<30 mL/hour), cool arms and legs, and decreased ...
is caused by abnormal heart function or problems within the heart that impair pumping of blood within the heart. Common causes of cardiogenic shock include congenital heart diseases, arrhythmia
Arrhythmias, also known as cardiac arrhythmias, are irregularities in the cardiac cycle, heartbeat, including when it is too fast or too slow. Essentially, this is anything but normal sinus rhythm. A resting heart rate that is too fast – ab ...
s, myocarditis
Myocarditis is inflammation of the cardiac muscle. Myocarditis can progress to inflammatory cardiomyopathy when there is associated ventricular remodeling and cardiac dysfunction due to chronic inflammation. Symptoms can include shortness of bre ...
(inflammation of the heart muscle), cardiomyopathy
Cardiomyopathy is a group of primary diseases of the heart muscle. Early on there may be few or no symptoms. As the disease worsens, shortness of breath, feeling tired, and swelling of the legs may occur, due to the onset of heart failure. A ...
(impairment of the heart's ability to pump), trauma/injury of the heart, drug or poison toxicity. Common signs include tachycardia, distant pulses, and worsening with giving fluids.
Obstructive shock
Obstructive shock
Obstructive shock is one of the four types of shock, caused by a physical obstruction in the flow of blood. Obstruction can occur at the level of the great vessels or the heart itself. Causes include pulmonary embolism, cardiac tamponade, and ten ...
is caused by disrupted flow of blood to the heart or flow of blood out of the heart. Common causes include tension pneumothorax
A pneumothorax is collection of air in the pleural space between the lung and the chest wall. Symptoms typically include sudden onset of sharp, one-sided chest pain and shortness of breath. In a minority of cases, a one-way valve is formed b ...
, cardiac tamponade
Cardiac tamponade, also known as pericardial tamponade (), is a compression of the heart due to pericardial effusion (the build-up of pericardial fluid in the pericardium, sac around the heart). Onset may be rapid or gradual. Symptoms typically i ...
, pulmonary embolism
Pulmonary embolism (PE) is a blockage of an pulmonary artery, artery in the lungs by a substance that has moved from elsewhere in the body through the bloodstream (embolism). Symptoms of a PE may include dyspnea, shortness of breath, chest pain ...
, and ductal dependent congenital heart defects (conditions that worsen when the ductus arteriosus
The ductus arteriosus, also called the ductus Botalli, named after the Italian physiologist Leonardo Botallo, is a blood vessel in the developing fetus connecting the trunk of the pulmonary artery to the proximal descending aorta. It allows mos ...
closes after birth) (e.g., hypoplastic left heart syndrome
Hypoplastic left heart syndrome (HLHS) is a rare congenital heart defect in which the left side of the heart is severely underdeveloped and incapable of supporting the systemic circulation. It is estimated to account for 2-3% of all congenital hea ...
and coarctation of the aorta
Coarctation of the aorta (CoA) is a congenital condition whereby the aorta is narrow, usually in the area where the ductus arteriosus ( ligamentum arteriosum after regression) inserts. The word ''coarctation'' means "pressing or drawing toget ...
).
* Tension pneumothorax
A pneumothorax is collection of air in the pleural space between the lung and the chest wall. Symptoms typically include sudden onset of sharp, one-sided chest pain and shortness of breath. In a minority of cases, a one-way valve is formed b ...
: a build up of air in the pleural space
The pleural cavity, or pleural space (or sometimes intrapleural space), is the potential space between the pulmonary pleurae, pleurae of the pleural sac that surrounds each lung. A small amount of serous fluid, serous pleural fluid is maintained ...
of the lungs causing compression and collapse of the lung. Common signs include trauma to the chest, distended neck veins, tracheal deviation (away from side of injury), and decreased breath sounds on side of injury.
* Cardiac tamponade
Cardiac tamponade, also known as pericardial tamponade (), is a compression of the heart due to pericardial effusion (the build-up of pericardial fluid in the pericardium, sac around the heart). Onset may be rapid or gradual. Symptoms typically i ...
: a build up of fluid or blood in the space surrounding the heart (pericardium
The pericardium (: pericardia), also called pericardial sac, is a double-walled sac containing the heart and the roots of the great vessels. It has two layers, an outer layer made of strong inelastic connective tissue (fibrous pericardium), ...
) causing compression of the heart. Common signs include muffled heart sounds and pulsus paradoxus.
* Pulmonary embolism
Pulmonary embolism (PE) is a blockage of an pulmonary artery, artery in the lungs by a substance that has moved from elsewhere in the body through the bloodstream (embolism). Symptoms of a PE may include dyspnea, shortness of breath, chest pain ...
: obstruction of a pulmonary artery
A pulmonary artery is an artery in the pulmonary circulation that carries deoxygenated blood from the right side of the heart to the lungs. The largest pulmonary artery is the ''main pulmonary artery'' or ''pulmonary trunk'' from the heart, and ...
or a branch of the pulmonary arteries most commonly by a clot causing blocked flow of blood out of or back into the heart. Children with predispositions to forming clots such as those with sickle cell disease
Sickle cell disease (SCD), also simply called sickle cell, is a group of inherited Hemoglobinopathy, haemoglobin-related blood disorders. The most common type is known as sickle cell anemia. Sickle cell anemia results in an abnormality in the ...
, cancer, coagulation disorders, and central venous catheter
A central venous catheter (CVC), also known as a central line (c-line), central venous line, or central venous access catheter, is a catheter placed into a large vein. It is a form of venous access. Placement of larger catheters in more centr ...
s are more likely to have pulmonary emboli. Common signs include worsening heart and lung function as evidenced by chest pain, tachycardia
Tachycardia, also called tachyarrhythmia, is a heart rate that exceeds the normal resting rate. In general, a resting heart rate over 100 beats per minute is accepted as tachycardia in adults. Heart rates above the resting rate may be normal ...
, shortness of breath
Shortness of breath (SOB), known as dyspnea (in AmE) or dyspnoea (in BrE), is an uncomfortable feeling of not being able to breathe well enough. The American Thoracic Society defines it as "a subjective experience of breathing discomfort that con ...
, heart failure
Heart failure (HF), also known as congestive heart failure (CHF), is a syndrome caused by an impairment in the heart's ability to Cardiac cycle, fill with and pump blood.
Although symptoms vary based on which side of the heart is affected, HF ...
, and more.
Management
Management of shock should be based on the type of shock. When the type of shock hasn't been identified yet, the provider should start with some initial treatments and labs. All children with suspected shock should receive supplementaloxygen
Oxygen is a chemical element; it has chemical symbol, symbol O and atomic number 8. It is a member of the chalcogen group (periodic table), group in the periodic table, a highly reactivity (chemistry), reactive nonmetal (chemistry), non ...
, ventilation if in respiratory distress (via nasal canula, high flow nasal canula, noninvasive ventilation
Non-invasive ventilation (NIV) is the use of breathing support administered through a face mask, nasal mask, or a helmet. Air, usually with added oxygen, is given through the mask under positive pressure; generally the amount of pressure is alte ...
, or mechanical ventilation
Mechanical ventilation or assisted ventilation is the Medicine, medical term for using a ventilator, ventilator machine to fully or partially provide artificial ventilation. Mechanical ventilation helps move air into and out of the lungs, wit ...
), and treatment for life-threatening conditions. Providers should establish vascular access (intravenous
Intravenous therapy (abbreviated as IV therapy) is a medical technique that administers fluids, medications and nutrients directly into a person's vein. The intravenous route of administration is commonly used for rehydration or to provide nutr ...
access IVs with a large caliber needle">Intravenous_therapy.html" ;"title=" peripheral IVs with a large caliber needleand if that isn't possible, intraosseous access (IO) or central venous line). Providers should also obtain initial lab studies including a Blood sugar level">rapid blood glucose, basic metabolic panel">Central venous catheter">central venous line). Providers should also obtain initial lab studies including a Blood sugar level">rapid blood glucose, basic metabolic panel (BMP) (measures serum electrolytes, blood urea nitrogen, and creatinine), Lactic acidosis, lactic acid level, complete blood count (CBC), and Urine test strip, urine dipstick.

Fluids
The provider should start crystalloid fluids (normal saline
Saline (also known as saline solution) is a mixture of sodium chloride (salt) and water. It has a number of uses in medicine including cleaning wounds, removal and storage of contact lenses, and help with dry eyes. By intravenous therapy, inje ...
or lactated Ringers). For compensated shock give 10-20 ml/kg over 5-20 min and for hypotensive shock, give 20 ml/lg over 5-10 min. However, if there are signs that the patient has too much fluid (fluid overload) such as worsening respiratory distress, jugular venous distention, crackles
Crackles are the clicking, rattling, or crackling noises that may be made by one or both lungs of a human or animal with a respiratory disease during inhalation, and occasionally during exhalation. They are usually heard only with a stethosco ...
, hepatomegaly
Hepatomegaly is enlargement of the liver. It is a non-specific sign (medicine), medical sign, having many causes, which can broadly be broken down into infection, hepatic tumours, and metabolic disorder. Often, hepatomegaly presents as an abdomin ...
, then fluids should not be given. With continued signs of shock and no signs of fluid overload, kids can continue to receive 10-20 ml/kg of fluids with a max of 60 ml/kg in the first hour. However, if cardiogenic shock is suspected, kids should receive less fluids over a longer time (e.g., 5-10 ml/kg over 15-30 min).
Hypovolemic shock
Hypovolemic shock is mainly treated with fluid replacement, as described in the fluids section above. If the hypovolemic shock is caused by a hemorrhage, then the provider should obtainblood type
A blood type (also known as a blood group) is based on the presence and absence of antibody, antibodies and Heredity, inherited antigenic substances on the surface of red blood cells (RBCs). These antigens may be proteins, carbohydrates, glycop ...
, blood cross match, and coagulation studies ( PT, INR, PTT). In hemorrhagic shock, patients should receive blood or blood products if they aren't improving with fluids.
Distributive shock
Distributive shock is mainly treated with fluid replacement, as described in the fluids section above, andvasopressors
An antihypotensive, also known as a vasopressor, is an agent that raises blood pressure by constricting blood vessels, thereby increasing systemic vascular resistance. This is different from inotropes which increase the force of cardiac contra ...
. For those with suspected septic shock, providers should obtain blood culture
A blood culture is a medical laboratory test used to detect bacteria or fungi in a person's blood. Under normal conditions, the blood does not contain microorganisms: their presence can indicate a bloodstream infection such as bacteremia or ...
, urinalysis
Urinalysis, a portmanteau of the words ''urine'' and ''analysis'', is a Test panel, panel of medical tests that includes physical (macroscopic) examination of the urine, chemical evaluation using urine test strips, and #Microscopic examination, m ...
, urine culture
Bacteriuria is the presence of bacteria in urine. Bacteriuria accompanied by symptoms is a urinary tract infection while that without is known as asymptomatic bacteriuria. Diagnosis is by urinalysis or urine culture. ''Escherichia coli'' is the ...
, c-reactive protein
C-reactive protein (CRP) is an annular (ring-shaped) pentameric protein found in blood plasma, whose circulating concentrations rise in response to inflammation. It is an acute-phase protein of hepatic origin that increases following interleukin ...
(CRP) (marker of inflammation), procalcitonin (marker of inflammation), fibrinogen
Fibrinogen (coagulation factor I) is a glycoprotein protein complex, complex, produced in the liver, that circulates in the blood of all vertebrates. During tissue and vascular injury, it is converted Enzyme, enzymatically by thrombin to fibrin ...
, D-dimer
D-dimer (or D dimer) is a dimer that is a fibrin degradation product (FDP), a small protein fragment present in the blood after a blood clot is degraded by fibrinolysis. It is so named because it contains two D fragments of the fibrin protein ...
, bilirubin
Bilirubin (BR) (adopted from German, originally bili—bile—plus ruber—red—from Latin) is a red-orange compound that occurs in the normcomponent of the straw-yellow color in urine. Another breakdown product, stercobilin, causes the brown ...
labs, and more. Those in anaphylactic shock should be treated with intramuscular epinephrine.
Cardiogenic shock
Cardiogenic shock typically worsens with fluids. Providers should obtain anECG
Electrocardiography is the process of producing an electrocardiogram (ECG or EKG), a recording of the heart's electrical activity through repeated cardiac cycles.
It is an electrogram of the heart which is a graph of voltage versus time of ...
and echocardiogram
Echocardiography, also known as cardiac ultrasound, is the use of ultrasound to examine the heart. It is a type of medical imaging, using standard ultrasound or Doppler ultrasound. The visual image formed using this technique is called an echo ...
for patients suspected to have cardiogenic shock. Treatment can include vasopressors
An antihypotensive, also known as a vasopressor, is an agent that raises blood pressure by constricting blood vessels, thereby increasing systemic vascular resistance. This is different from inotropes which increase the force of cardiac contra ...
, inotrope
An inotrope or inotropic is a drug or any substance that alters the force or energy of muscular contractions. Negatively inotropic agents weaken the force of muscular contractions. Positively inotropic agents increase the strength of muscular ...
s, and treatment of any arrhythmia
Arrhythmias, also known as cardiac arrhythmias, are irregularities in the cardiac cycle, heartbeat, including when it is too fast or too slow. Essentially, this is anything but normal sinus rhythm. A resting heart rate that is too fast – ab ...
s.
Obstructive shock
Obstructive shock is treated by treating the underlying cause of the shock. Tension pneumothorax is treated with achest tube
A chest tube (also chest drain, thoracic catheter, tube thoracostomy or intercostal drain) is a drain (surgery), surgical drain that is inserted through the chest wall and into the pleural space or the Mediastinum. The insertion of the tube is som ...
and needle thoracostomy which allows the air to get out of the pleural space. Cardiac tamponade is treated with pericardiocentesis
Pericardiocentesis (PCC), also called pericardial tap, is a medical procedure where fluid is aspirated from the pericardium (the sac enveloping the heart).
Anatomy and physiology
The pericardium is a fibrous sac surrounding the heart composed o ...
which removes the fluid from the pericardium and decompresses the heart. Pulmonary embolism is treated with anticoagulant
An anticoagulant, commonly known as a blood thinner, is a chemical substance that prevents or reduces the coagulation of blood, prolonging the clotting time. Some occur naturally in blood-eating animals, such as leeches and mosquitoes, which ...
s (prevent body from making more clots) and if bad enough, thrombectomy
Mechanical thrombectomy, or simply thrombectomy, is the removal of a blood clot (thrombus) from a blood vessel, often and especially endovascularly as an interventional radiology procedure called endovascular thrombectomy (EVT). It thus contr ...
(surgical removal of clots). Ductal dependent congenital heart defects are treated with prostaglandin E1
Prostaglandin E1 (PGE1) is a naturally occurring prostaglandin with various medical uses. Alprostadil and misoprostol are synthetic forms of prostaglandin E1 used as medications. Lubiprostone, a derivative of prostaglandin E1, is also used as ...
/ alprostadil which keeps the ductus arteriosus
The ductus arteriosus, also called the ductus Botalli, named after the Italian physiologist Leonardo Botallo, is a blood vessel in the developing fetus connecting the trunk of the pulmonary artery to the proximal descending aorta. It allows mos ...
open.
Cardiac Arrest
Cardiac arrest
Cardiac arrest (also known as sudden cardiac arrest CA is when the heart suddenly and unexpectedly stops beating. When the heart stops beating, blood cannot properly Circulatory system, circulate around the body and the blood flow to the ...
occurs when the heart stops working and blood stops moving throughout the body.
In infants and children, cardiac arrest is typically caused by (1) hypoxic/asphyxial arrest and less commonly by (2) sudden cardiac arrest due to heart problems or arrhythmias. In adults, cardiac arrest is usually caused by heart problems such as acute coronary syndrome
Acute coronary syndrome (ACS) is a syndrome due to decreased blood flow in the coronary arteries such that part of the heart muscle is unable to function properly or dies. The most common symptom is centrally located pressure-like chest pain, ...
. Hypoxic/asphyxial cardiac arrest is a result of progressive respiratory failure and/or shock. For this reason, it is important to treat respiratory failure and shock early so that they don't progress to cardiac arrest.
Sudden cardiac arrest is typically caused by arrhythmias such ventricular fibrillation
Ventricular fibrillation (V-fib or VF) is an abnormal heart rhythm in which the Ventricle (heart), ventricles of the heart Fibrillation, quiver. It is due to disorganized electrical conduction system of the heart, electrical activity. Ventricula ...
(VF) and pulseless ventricular tachycardia (pVT). These arrhythmias are more common in kids with hypertrophic cardiomyopathy
Hypertrophic cardiomyopathy (HCM, or HOCM when obstructive) is a condition in which muscle tissues of the heart become thickened without an obvious cause. The parts of the heart most commonly affected are the interventricular septum and the ...
, cardiac channelopathies (e.g., long QT syndrome
Long QT syndrome (LQTS) is a condition affecting repolarization (relaxing) of the heart after a heartbeat, giving rise to an abnormally lengthy QT interval. It results in an increased risk of an irregular heartbeat which can result in fainti ...
), myocarditis
Myocarditis is inflammation of the cardiac muscle. Myocarditis can progress to inflammatory cardiomyopathy when there is associated ventricular remodeling and cardiac dysfunction due to chronic inflammation. Symptoms can include shortness of bre ...
, drugs (e.g., cocaine
Cocaine is a tropane alkaloid and central nervous system stimulant, derived primarily from the leaves of two South American coca plants, ''Erythroxylum coca'' and ''Erythroxylum novogranatense, E. novogranatense'', which are cultivated a ...
, digoxin
Digoxin (better known as digitalis), sold under the brand name Lanoxin among others, is a medication used to treat various heart disease, heart conditions. Most frequently it is used for atrial fibrillation, atrial flutter, and heart failure. ...
), commotio cordis, and anomalous coronary artery.
There are many causes of reversible cardiac arrest and the mnemonic "H's and T's" is used to remember these causes.
Recognition
Signs of cardiac arrest include no pulse (within 10 seconds), no breathing or only gasping, and unresponsiveness. As mentioned above, cardiac arrest in kids is mainly a result of respiratory failure and shock, so providers need to treat those conditions quickly and be on the look out for signs of cardiac arrest. Because cardiac arrest can also be caused by arrhythmias, providers should get ECGs of these patients. The 4 main cardiac arrest rhythms areventricular fibrillation
Ventricular fibrillation (V-fib or VF) is an abnormal heart rhythm in which the Ventricle (heart), ventricles of the heart Fibrillation, quiver. It is due to disorganized electrical conduction system of the heart, electrical activity. Ventricula ...
(VF), pulseless ventricular tachycardia
Ventricular tachycardia (V-tach or VT) is a cardiovascular disorder in which fast heart rate occurs in the ventricles of the heart. Although a few seconds of VT may not result in permanent problems, longer periods are dangerous; and multiple ...
(pVT), asystole
Asystole (New Latin, from Greek privative a "not, without" + ''systolē'' "contraction") is the absence of ventricular contractions in the context of a lethal heart arrhythmia (in contrast to an induced asystole on a cooled patient on a heart-lun ...
, and pulseless electrical activity
Pulseless electrical activity (PEA) is a form of cardiac arrest in which the electrocardiogram shows a heart rhythm that should produce a pulse, but does not. Pulseless electrical activity is found initially in about 20% of out-of-hospital cardia ...
(PEA).
ventricular fibrillation
Ventricular fibrillation (V-fib or VF) is an abnormal heart rhythm in which the Ventricle (heart), ventricles of the heart Fibrillation, quiver. It is due to disorganized electrical conduction system of the heart, electrical activity. Ventricula ...
(VF): disorganized and rapid quivering of the ventricles
* pulseless ventricular tachycardia
Ventricular tachycardia (V-tach or VT) is a cardiovascular disorder in which fast heart rate occurs in the ventricles of the heart. Although a few seconds of VT may not result in permanent problems, longer periods are dangerous; and multiple ...
(pVT): organized wide QRS complex
The QRS complex is the combination of three of the graphical deflections seen on a typical electrocardiogram (ECG or EKG). It is usually the central and most visually obvious part of the tracing. It corresponds to the depolarization of the ri ...
es with no pulse
* asystole
Asystole (New Latin, from Greek privative a "not, without" + ''systolē'' "contraction") is the absence of ventricular contractions in the context of a lethal heart arrhythmia (in contrast to an induced asystole on a cooled patient on a heart-lun ...
: no cardiac electrical activity, ECG shows a flat line *
* pulseless electrical activity
Pulseless electrical activity (PEA) is a form of cardiac arrest in which the electrocardiogram shows a heart rhythm that should produce a pulse, but does not. Pulseless electrical activity is found initially in about 20% of out-of-hospital cardia ...
(PEA): no pulses but ECG shows organized electrical activity (not VF or asystole); not a specific rhythm
Management
 Treatment of pediatric cardiac arrest follows the American Heart Association's (AHA) Pediatric Cardiac Arrest Algorithm. The goals of treatment are to obtain
Treatment of pediatric cardiac arrest follows the American Heart Association's (AHA) Pediatric Cardiac Arrest Algorithm. The goals of treatment are to obtain return of spontaneous circulation
Return of spontaneous circulation (ROSC) is the resumption of a sustained heart rhythm that perfuses the body after cardiac arrest. It is commonly associated with significant respiratory effort. Signs of return of spontaneous circulation include b ...
(ROSC), meaning that the heart starts working on its own.
 Once cardiac arrest is recognized, high quality
Once cardiac arrest is recognized, high quality CPR
Cardiopulmonary resuscitation (CPR) is an emergency procedure used during cardiac or respiratory arrest that involves chest compressions, often combined with artificial ventilation, to preserve brain function and maintain circulation until sp ...
needs to be started immediately. After starting chest compressions, the provider should (1) give ventilations (via bag mask) and oxygen, (2) attach monitor/defibrillator
Defibrillation is a treatment for life-threatening cardiac arrhythmias, specifically ventricular fibrillation (V-Fib) and non-perfusing ventricular tachycardia (V-Tach). Defibrillation delivers a dose of electric current (often called a ''count ...
pads or ECG electrode
An electrode is an electrical conductor used to make contact with a nonmetallic part of a circuit (e.g. a semiconductor, an electrolyte, a vacuum or a gas). In electrochemical cells, electrodes are essential parts that can consist of a varie ...
s to the child so that defibrillation
Defibrillation is a treatment for life-threatening cardiac arrhythmias, specifically ventricular fibrillation (V-Fib) and non-perfusing ventricular tachycardia (V-Tach). Defibrillation delivers a dose of electric current (often called a ''count ...
s (aka shocks) can be given if needed, and (3) establish vascular access (IV, IO). Attaching the defibrillator and establishing vascular access should NOT interrupt chest compressions.
Once the monitor/defibrillator is connected, the provider should assess the heart rhythm. Of the 4 cardiac arrest rhythms, VF and pVT are shockable rhythms and asystole
Asystole (New Latin, from Greek privative a "not, without" + ''systolē'' "contraction") is the absence of ventricular contractions in the context of a lethal heart arrhythmia (in contrast to an induced asystole on a cooled patient on a heart-lun ...
and PEA
Pea (''pisum'' in Latin) is a pulse or fodder crop, but the word often refers to the seed or sometimes the pod of this flowering plant species. Peas are eaten as a vegetable. Carl Linnaeus gave the species the scientific name ''Pisum sativum' ...
are unshockable rhythms. Shockable rhythms are rhythms that can improve with a shock and thus, should receive a shock. Unshockable rhythms are rhythms that won't improve with a shock and thus, should NOT receive a shock. The monitor/defibrillator will either tell the providers if the rhythm is shockable (automated external defibrillator
An automated external defibrillator (AED) is a portable electronic device that automatically diagnoses the life-threatening cardiac Heart arrhythmia, arrhythmias of ventricular fibrillation (VF) and pulseless ventricular tachycardia, and is able ...
s (AED)) or the providers will be able to read the ECG and determine for themselves if the rhythm is shockable (manual defibrillators). If shockable, give a shock then resume CPR. If not shockable, continue CPR, give epinephrine, and consider an advanced airway.
After every 2 minutes of giving CPR the provider should reassess the patient's heart rhythm to see if it is shockable or unshockable, and give a shock if it is shockable. This 2 minute cycle of CPR and rhythm assessment should continue until it is determined by the providers that further management is unlikely to save the patient. For patients with shockable rhythms who haven't achieved ROSC, providers can give epinephrine after 2 shocks and amiodarone or lidocaine after 3 shocks. Throughout CPR and rhythm assessments, the providers should be treating any suspected reversible causes of cardiac arrest (H's and T's listed above).
Defibrillations/shocks
* first shock should be 2 J/kg
* second shock should be 4 J/kg
* all other shocks should be ≥ 4 J/kg with max of 10 J/kg
Medicines that can be given during treatment of cardiac arrest are listed below. The doses listed below are for IV/IO medicationa. Medications via endotracheal tube (ET) are often given at higher doses.
* epinephrine
Adrenaline, also known as epinephrine, is a hormone and medication which is involved in regulating visceral functions (e.g., respiration). It appears as a white microcrystalline granule. Adrenaline is normally produced by the adrenal glands a ...
: 0.01 mg/kg every 3–5 minutes with max single dose of 1 mg
* amiodarone
Amiodarone is an antiarrhythmic medication used to treat and prevent a number of types of cardiac dysrhythmias. This includes ventricular tachycardia, ventricular fibrillation, and wide complex tachycardia, atrial fibrillation, and paroxys ...
: 5 mg/kg initially, can repeat 2 more times (total of 3 doses), max of 300 mg per dose, max 15 mg/kg, given for refractory VF and pVT
* lidocaine
Lidocaine, also known as lignocaine and sold under the brand name Xylocaine among others, is a local anesthetic of the amino amide type. It is also used to treat ventricular tachycardia and ventricular fibrillation. When used for local anae ...
: 1 mg/kg initially with continuous infusion of 20-50 mcg/kg/min after, given for refractory VF and pVT
* magnesium sulfate
Magnesium sulfate or magnesium sulphate is a chemical compound, a salt with the formula , consisting of magnesium cations (20.19% by mass) and sulfate anions . It is a white crystalline solid, soluble in water but not in ethanol.
Magnesi ...
: 25–50 mg/kg diluted in 10 ml D5W (5% dextrose) and infused over 1–2 minutes, max 2g per dose, given for pulseless torsades de pointes
''Torsades de pointes, torsade de pointes'' or ''torsades des pointes'' (TdP; also called ''torsades'') (, , translated as "twisting of peaks") is a specific type of abnormal heart rhythm that can lead to sudden cardiac death. It is a polymorph ...
(a type of ventricular tachycardia)
Arrhythmias
PALS providers should be able to identify and treat different types of abnormal pediatric heart rhythms including bradyarrhythmias,tachyarrhythmias
Tachycardia, also called tachyarrhythmia, is a heart rate that exceeds the normal resting rate. In general, a resting heart rate over 100 beats per minute is accepted as tachycardia in adults. Heart rates above the resting rate may be normal ...
, and cardiac arrest rhythms (discussed above). In defining heart rates that are too slow or too fast, it is important to understand the ranges of pediatric heart rates by age. Normal ranges of pediatric heart rates change with age, with heart rates being faster closer to birth and slower closer to adulthood.
Bradyarrythmias
Bradycardia
Bradycardia, also called bradyarrhythmia, is a resting heart rate under 60 beats per minute (BPM). While bradycardia can result from various pathological processes, it is commonly a physiological response to cardiovascular conditioning or due ...
is defined as a slow heart rate for a child's age. Bradycardia associated with signs of shock (altered mental status, hypotension, etc.) can be an early warning sign for cardiac arrest. Signs of bradycardia include fatigue, confusion, dizziness, and lightheadedness. Possible causes of bradycardia include hypoxia, hypothermia
Hypothermia is defined as a body core temperature below in humans. Symptoms depend on the temperature. In mild hypothermia, there is shivering and mental confusion. In moderate hypothermia, shivering stops and confusion increases. In severe ...
, and certain medications.
 Types of bradyarrhythmias
*
Types of bradyarrhythmias
* sinus bradycardia
Sinus bradycardia is a sinus rhythm with a reduced rate of electrical discharge from the sinoatrial node, resulting in a bradycardia, a heart rate that is lower than the normal range (60–100 beats per minute for adult humans).
Signs and sympt ...
: normal rhythm, slow rate
* atrioventricular block
Atrioventricular block (AV block) is a type of heart block that occurs when the electrical signal traveling from the atria, or the upper chambers of the heart, to ventricles, or the lower chambers of the heart, is impaired. Normally, the sinoatr ...
** first degree: prolonged PR interval (> 0.20 seconds)
** second degree
*** mobitz type I (wenckebach): progressive lengthening of PR interval then dropped beat (p wave with no QRS)
*** mobitz type II: equal PR intervals with intermittent dropped beats (p wave with no QRS)
** third degree: complete dissociation between p wave
A P wave (primary wave or pressure wave) is one of the two main types of elastic body waves, called seismic waves in seismology. P waves travel faster than other seismic waves and hence are the first signal from an earthquake to arrive at any ...
and QRS complex
The QRS complex is the combination of three of the graphical deflections seen on a typical electrocardiogram (ECG or EKG). It is usually the central and most visually obvious part of the tracing. It corresponds to the depolarization of the ri ...
, atria and ventricles are beating independent of one another
Management
Providers should follow the AHA's Pediatric Bradycardia With a Pulse Algorithm. As always, provides need to support airway, breathing, and circulation and begin CPR if needed. Bradyarrythmias with signs of shock can be treated with epinephrine and atropine in order to increase heart rate. If medications aren't helping, providers can consider cardiac pacing. * epinephrine: 0.01 mg/kg every 3–5 minutes *atropine
Atropine is a tropane alkaloid and anticholinergic medication used to treat certain types of nerve agent and pesticide poisonings as well as some types of slow heart rate, and to decrease saliva production during surgery. It is typically give ...
: 0.02 mg/kg, can repeat one time, max dose 0.5 mg, min dose of 0.1 mg
Tachyarrhythmias
Tachycardia
Tachycardia, also called tachyarrhythmia, is a heart rate that exceeds the normal resting rate. In general, a resting heart rate over 100 beats per minute is accepted as tachycardia in adults. Heart rates above the resting rate may be normal ...
is defined as a fast heart rate for a child's age. Signs of tachycardia are similar to bradycardia but also include palpitations, decreased feeding/eating, and irritability. Tachyarrhythmias are fast abnormal heart rhythms.
Types of tachyarrhythmias
* Management
Providers should follow the AHA's Pediatric Tachycardia With a Pulse Algorithm. As always, provides need to support airway, breathing, and circulation and begin CPR if needed. Management of tachyarrhythmias depends on if the child is stable or unstable (experiencing cardiopulmonary compromise: signs of shock, hypotension, altered mental status). Unstable tachyarrhythmia is treated with synchronized cardioversion - initially 0.5-1 J/kg but can increase to 2 J/kg if smaller dose is not working. Stable tachyarrhythmia treatment is subcategorized based on narrow QRS vs. wide QRS. If narrow QRS/ SVT, performvagal maneuver
A vagal maneuver is an action used to stimulate the parasympathetic nervous system by activating the vagus nerve. The vagus nerve is the longest nerve of the autonomic nervous system and helps regulate many critical aspects of human physiology, i ...
s and give adenosine
Adenosine (symbol A) is an organic compound that occurs widely in nature in the form of diverse derivatives. The molecule consists of an adenine attached to a ribose via a β-N9- glycosidic bond. Adenosine is one of the four nucleoside build ...
. If wide QRS/ VT with regular rhythm and monomorphic QRS, the provider can give adenosine and should consult pediatric cardiology
Cardiology () is the study of the heart. Cardiology is a branch of medicine that deals with disorders of the heart and the cardiovascular system. The field includes medical diagnosis and treatment of congenital heart defects, coronary artery di ...
for recommendations.
* adenosine
Adenosine (symbol A) is an organic compound that occurs widely in nature in the form of diverse derivatives. The molecule consists of an adenine attached to a ribose via a β-N9- glycosidic bond. Adenosine is one of the four nucleoside build ...
: first dose 0.1 mg/kg with max 6 mg, second dose 0.2 mg/kg with max 12 mg
Criticism
PETA
People for the Ethical Treatment of Animals (PETA; ) is an American animal rights nonprofit organization based in Norfolk, Virginia, and led by Ingrid Newkirk, its international president.
Founded in March 1980 by Newkirk and animal right ...
has criticized the use of animals in PALS training which the organization calls "cruel and unnecessary". PETA says that hundreds of PALS training centers have begun using simulators in response to concerns regarding the animals' welfare. The American Heart Association neither endorses nor requires the use of animals in intubation training.
See also
* Advanced Pediatric Life Support (APLS) * Advanced Cardiac Life Support (ACLS) * Neonatal Resuscitation Program (NRP)References
External links
American Heart Association
Pediatric Advanced Life Support Course -- PALS
{{Emergency medicine Medical credentials Emergency medicine courses Emergency life support Pediatrics