T-helper cells on:
[Wikipedia]
[Google]
[Amazon]
 The T helper cells (Th cells), also known as CD4+ cells or CD4-positive cells, are a type of
The T helper cells (Th cells), also known as CD4+ cells or CD4-positive cells, are a type of
 Following
Following
 During an immune response, professional antigen-presenting cells (APCs) endocytose antigens (typically bacteria or viruses), which undergo processing, then travel from the infection site to the
During an immune response, professional antigen-presenting cells (APCs) endocytose antigens (typically bacteria or viruses), which undergo processing, then travel from the infection site to the
 The T helper cells (Th cells), also known as CD4+ cells or CD4-positive cells, are a type of
The T helper cells (Th cells), also known as CD4+ cells or CD4-positive cells, are a type of T cell
T cells (also known as T lymphocytes) are an important part of the immune system and play a central role in the adaptive immune response. T cells can be distinguished from other lymphocytes by the presence of a T-cell receptor (TCR) on their cell ...
that play an important role in the adaptive immune system
The adaptive immune system (AIS), also known as the acquired immune system, or specific immune system is a subsystem of the immune system that is composed of specialized cells, organs, and processes that eliminate pathogens specifically. The ac ...
. They aid the activity of other immune cells by releasing cytokines
Cytokines () are a broad and loose category of small proteins (~5–25 kDa) important in cell signaling.
Cytokines are produced by a broad range of cells, including immune cells like macrophages, B cell, B lymphocytes, T cell, T lymphocytes ...
. They are considered essential in B cell
B cells, also known as B lymphocytes, are a type of the lymphocyte subtype. They function in the humoral immunity component of the adaptive immune system. B cells produce antibody molecules which may be either secreted or inserted into the plasm ...
antibody class switching, breaking cross-tolerance in dendritic cells, in the activation and growth of cytotoxic T cell
A cytotoxic T cell (also known as TC, cytotoxic T lymphocyte, CTL, T-killer cell, cytolytic T cell, CD8+ T-cell or killer T cell) is a T lymphocyte (a type of white blood cell) that kills cancer cells, cells that are infected by intracellular ...
s, and in maximizing bactericidal
A bactericide or bacteriocide, sometimes abbreviated Bcidal, is a substance which kills bacteria. Bactericides are disinfectants, antiseptics, or antibiotics.
However, material surfaces can also have bactericidal properties based solely on their p ...
activity of phagocytes
Phagocytes are cell (biology), cells that protect the body by ingesting harmful foreign particles, bacteria, and dead or Apoptosis, dying cells. Their name comes from the Greek language, Greek ', "to eat" or "devour", and "-cyte", the suffix in ...
such as macrophages
Macrophages (; abbreviated MPhi, φ, MΦ or MP) are a type of white blood cell of the innate immune system that engulf and digest pathogens, such as cancer cells, microbes, cellular debris and foreign substances, which do not have proteins that ...
and neutrophil
Neutrophils are a type of phagocytic white blood cell and part of innate immunity. More specifically, they form the most abundant type of granulocytes and make up 40% to 70% of all white blood cells in humans. Their functions vary in differe ...
s. CD4+ cells are mature Th cells that express the surface protein CD4. Genetic variation in regulatory elements expressed by CD4+ cells determines susceptibility to a broad class of autoimmune disease
An autoimmune disease is a condition that results from an anomalous response of the adaptive immune system, wherein it mistakenly targets and attacks healthy, functioning parts of the body as if they were foreign organisms. It is estimated tha ...
s.
Structure and function
Th cells contain and release cytokines to aid other immune cells. Cytokines are small protein mediators that alter the behavior of target cells that express receptors for those cytokines. These cells help polarize the immune response depending on the nature of the immunological insult (for example; virus vs. extracellularbacterium
Bacteria (; : bacterium) are ubiquitous, mostly free-living organisms often consisting of one biological cell. They constitute a large domain of prokaryotic microorganisms. Typically a few micrometres in length, bacteria were among the ...
vs. intracellular bacterium vs. helminth vs. fungus vs. protist).
Mature Th cells express the surface protein CD4
In molecular biology, CD4 (cluster of differentiation 4) is a glycoprotein that serves as a co-receptor for the T-cell receptor (TCR). CD4 is found on the surface of immune cells such as helper T cells, monocytes, macrophages, and dendritic c ...
and are referred to as CD4+ T cells. CD4+ T cells are generally treated as having a pre-defined role as helper T cells within the immune system
The immune system is a network of biological systems that protects an organism from diseases. It detects and responds to a wide variety of pathogens, from viruses to bacteria, as well as Tumor immunology, cancer cells, Parasitic worm, parasitic ...
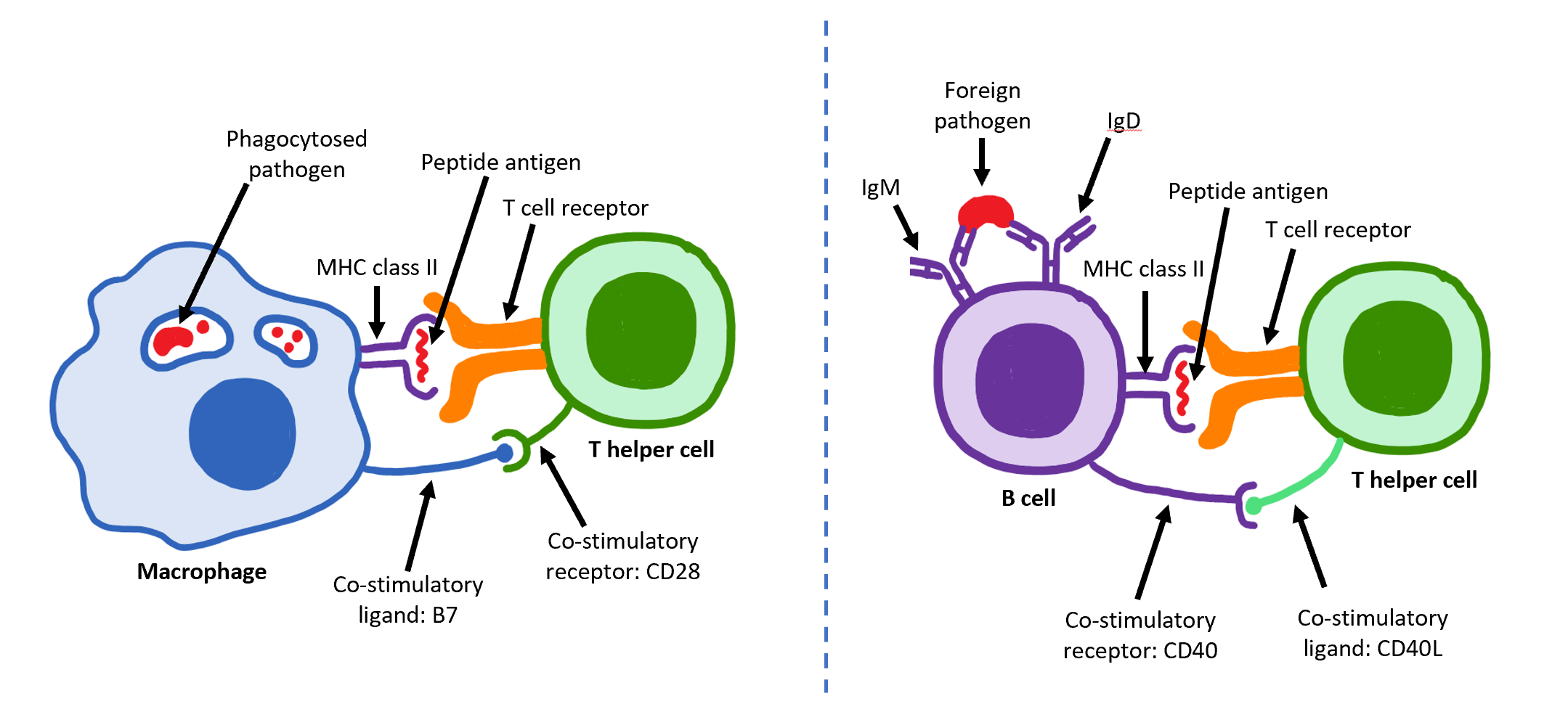
. For example, when an antigen-presenting cell
An antigen-presenting cell (APC) or accessory cell is a Cell (biology), cell that displays an antigen bound by major histocompatibility complex (MHC) proteins on its surface; this process is known as antigen presentation. T cells may recognize the ...
displays a peptide
Peptides are short chains of amino acids linked by peptide bonds. A polypeptide is a longer, continuous, unbranched peptide chain. Polypeptides that have a molecular mass of 10,000 Da or more are called proteins. Chains of fewer than twenty am ...
antigen on MHC class II
MHC Class II molecules are a class of major histocompatibility complex (MHC) molecules normally found only on professional antigen-presenting cells such as dendritic cells, macrophages, some endothelial cells, thymic epithelial cells, and B cell ...
proteins, a CD4+ cell will aid those cells through a combination of cell to cell interactions (e.g. CD40 (protein)
Cluster of differentiation 40, CD40 is a type I transmembrane protein found on antigen-presenting cells and is required for their activation. The binding of CD154 ( CD40L) on TH cells to CD40 activates antigen presenting cells and induces a var ...
and CD40L
CD154, also called CD40 ligand or CD40L, is a protein that is primarily expressed on activated T cells and is a member of the TNF superfamily of molecules. It binds to CD40 (protein), CD40 on antigen-presenting cells (APC), which leads to many e ...
) and through cytokines
Cytokines () are a broad and loose category of small proteins (~5–25 kDa) important in cell signaling.
Cytokines are produced by a broad range of cells, including immune cells like macrophages, B cell, B lymphocytes, T cell, T lymphocytes ...
.
Th cells are not a monolithic immunological entity because they are diverse in terms of function and their interaction with partner cells. In general, mature naive T cells are stimulated by professional antigen presenting cells to acquire an effector function. These are defined by the presence of a lineage-determining (or lineage-specifying) transcription factor (also called master regulator, though the term has been criticized for being too reductive). The loss of function in a lineage specifying transcription factor results in the absence of the corresponding class of helper T cell which can be devastating for the health of the host.
Activation of naive helper T cells
 Following
Following development
Development or developing may refer to:
Arts
*Development (music), the process by which thematic material is reshaped
* Photographic development
*Filmmaking, development phase, including finance and budgeting
* Development hell, when a proje ...
in the thymus
The thymus (: thymuses or thymi) is a specialized primary lymphoid organ of the immune system. Within the thymus, T cells mature. T cells are critical to the adaptive immune system, where the body adapts to specific foreign invaders. The thymus ...
, these cells (termed recent thymic emigrants (RTE)) egress from the thymus and home to secondary lymphoid organs
The lymphatic system, or lymphoid system, is an organ system in vertebrates that is part of the immune system and complementary to the circulatory system. It consists of a large network of lymphatic vessels, lymph nodes, lymphoid organs, lympha ...
(SLO; spleen
The spleen (, from Ancient Greek '' σπλήν'', splḗn) is an organ (biology), organ found in almost all vertebrates. Similar in structure to a large lymph node, it acts primarily as a blood filter.
The spleen plays important roles in reg ...
and lymph nodes
A lymph node, or lymph gland, is a kidney-shaped Organ (anatomy), organ of the lymphatic system and the adaptive immune system. A large number of lymph nodes are linked throughout the body by the lymphatic vessels. They are major sites of lymphoc ...
). Of note, only a very small minority of T cells egresses from the thymus (estimates commonly range from 1–5% but some experts feel even this is generous). Maturation of RTE in SLO results in the generation of mature naive T cells (naïve meaning they have never been exposed to the antigen
In immunology, an antigen (Ag) is a molecule, moiety, foreign particulate matter, or an allergen, such as pollen, that can bind to a specific antibody or T-cell receptor. The presence of antigens in the body may trigger an immune response.
...
that they are programmed to respond to), but naive T cells now lack or have downregulated (reduced) expression of the RTE-related surface markers, such as CD31
Platelet endothelial cell adhesion molecule (PECAM-1) also known as cluster of differentiation 31 (CD31) is a protein that in humans is encoded by the ''PECAM1'' gene found on chromosome 17, chromosome17q23.3. PECAM-1 plays a key role in removi ...
, PTK7, Complement Receptor 1 and 2 ( CR1, CR2) and the production of interleukin 8 (IL-8). Like all T cells, they express the T cell receptor
The T-cell receptor (TCR) is a protein complex, located on the surface of T cells (also called T lymphocytes). They are responsible for recognizing fragments of antigen as peptides bound to major histocompatibility complex (MHC) molecules. ...
- CD3 complex. The T cell receptor (TCR) consists of both constant and variable regions. The variable region determines what antigen the T cell can respond to. CD4+ T cells have TCRs with an affinity for Class II MHC, and CD4 is involved in determining MHC affinity during maturation in the thymus
The thymus (: thymuses or thymi) is a specialized primary lymphoid organ of the immune system. Within the thymus, T cells mature. T cells are critical to the adaptive immune system, where the body adapts to specific foreign invaders. The thymus ...
. Class II MHC proteins are generally only found on the surface of professional antigen-presenting cell
An antigen-presenting cell (APC) or accessory cell is a Cell (biology), cell that displays an antigen bound by major histocompatibility complex (MHC) proteins on its surface; this process is known as antigen presentation. T cells may recognize the ...
s (APCs). Professional antigen-presenting cells are primarily dendritic cells
A dendritic cell (DC) is an antigen-presenting cell (also known as an ''accessory cell'') of the mammalian immune system. A DC's main function is to process antigen material and present it on the cell surface to the T cells of the immune system ...
, macrophages
Macrophages (; abbreviated MPhi, φ, MΦ or MP) are a type of white blood cell of the innate immune system that engulf and digest pathogens, such as cancer cells, microbes, cellular debris and foreign substances, which do not have proteins that ...
and B cells
B cells, also known as B lymphocytes, are a type of the lymphocyte subtype. They function in the humoral immunity component of the adaptive immune system. B cells produce antibody molecules which may be either secreted or inserted into the plasm ...
, although dendritic cells are the only cell group that expresses MHC Class II constitutively (at all times). Some APCs also bind native (or unprocessed) antigens to their surface, such as follicular dendritic cells (these are ''not'' the same type of cells as the dendritic cell
A dendritic cell (DC) is an antigen-presenting cell (also known as an ''accessory cell'') of the mammalian immune system. A DC's main function is to process antigen material and present it on the cell surface to the T cells of the immune system ...
s of the immune system but rather have a non-hematopoietic origin, and in general lack MHC Class II, meaning they are not true professional antigen-presenting cells; however, follicular dendritic cells may acquire MHC Class II proteins via exosomes that become attached to them). T cells require antigens to be processed into short fragments which form linear epitopes on MHC Class II (in the case of helper T cells because they express CD4) or MHC class I (in the case of cytotoxic T cell
A cytotoxic T cell (also known as TC, cytotoxic T lymphocyte, CTL, T-killer cell, cytolytic T cell, CD8+ T-cell or killer T cell) is a T lymphocyte (a type of white blood cell) that kills cancer cells, cells that are infected by intracellular ...
s which express CD8
CD8 (cluster of differentiation 8) is a transmembrane protein, transmembrane glycoprotein that serves as a co-receptor for the T-cell receptor (TCR). Along with the TCR, the CD8 co-receptor plays a role in T cell Cell signaling, signaling and aid ...
). MHC Class II binding pockets are flexible with respect to the length of the peptides they hold. Generally, there are 9 core amino acid residues with several flanking amino acids which form a length of about 12–16 amino acids total but have been known to hold as many as 25 amino acids. By comparison, MHC Class I proteins are usually 9-10 peptides long. The activation of naive T cells is commonly explained in terms of the 3-signal model, elaborated upon below.
Activation (signal 1)
lymph node
A lymph node, or lymph gland, is a kidney-shaped organ of the lymphatic system and the adaptive immune system. A large number of lymph nodes are linked throughout the body by the lymphatic vessels. They are major sites of lymphocytes that includ ...
s. Typically, the APC responsible is a dendritic cell. If the antigen expresses appropriate molecular patterns (sometimes known as signal 0), it can induce maturation of the dendritic cell which results in enhanced expression of costimulatory molecules needed to activate T cells (see signal 2) and MHC Class II. Once at the lymph nodes, the APCs begin to present antigen peptides that are bound to Class II MHC, allowing CD4+ T cells that express the specific TCRs against the peptide/MHC complex to activate.
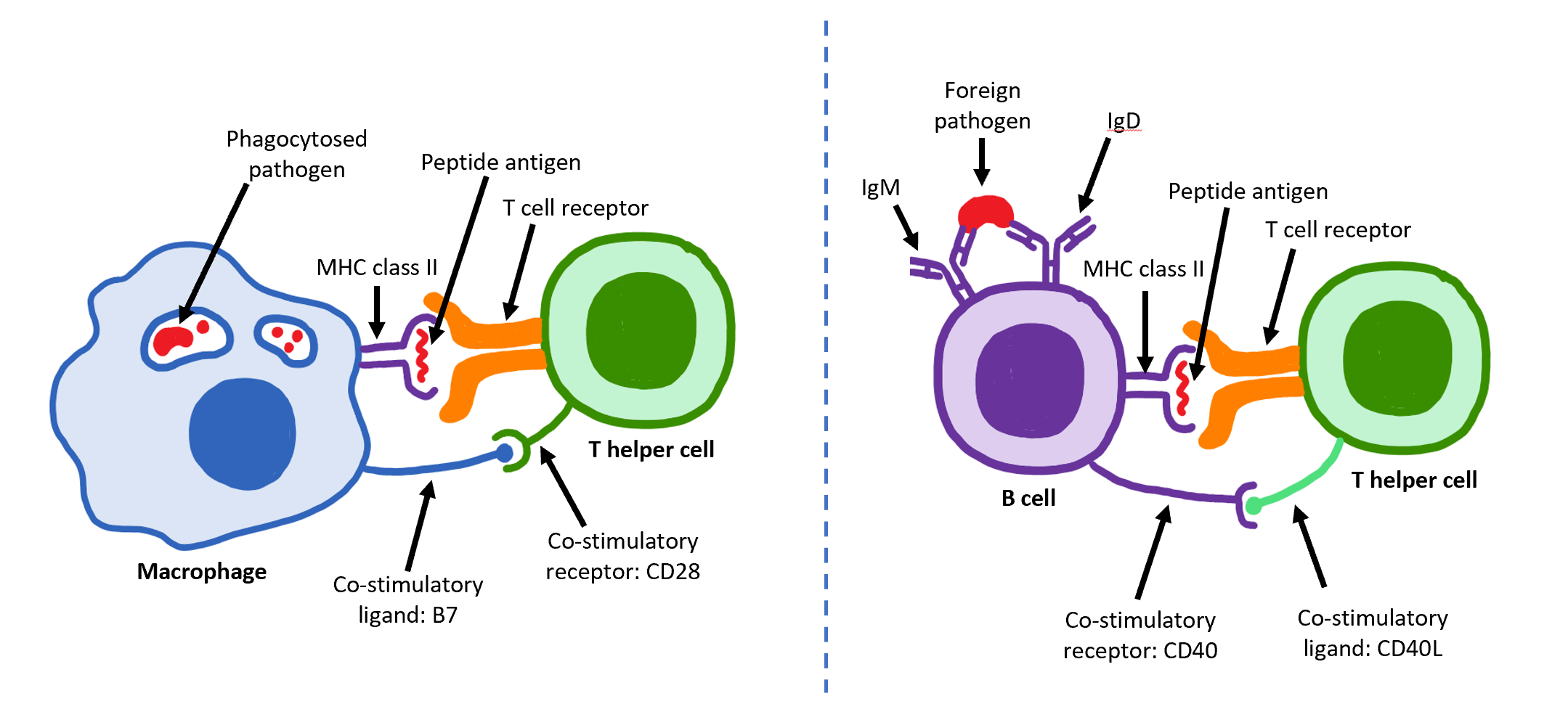
When a Th cell encounters and recognizes the antigen on an APC, the TCR- CD3 complex binds strongly to the peptide-MHC complex present on the surface of professional APCs. CD4
In molecular biology, CD4 (cluster of differentiation 4) is a glycoprotein that serves as a co-receptor for the T-cell receptor (TCR). CD4 is found on the surface of immune cells such as helper T cells, monocytes, macrophages, and dendritic c ...
, a co-receptor of the TCR complex, also binds to a different section of the MHC molecule. It is estimated that approximately 50 of these interactions are required for the activation of a helper T cell and assemblies known as microclusters have been observed forming between the TCR-CD3-CD4 complexes of the T cell and the MHC Class II proteins of the dendritic cell at the zone of contact. When these all come together, the CD4 is able to recruit a kinase called Lck which phosphorylates immunoreceptor tyrosine-based activation motif An immunoreceptor tyrosine-based activation motif (ITAM) is a conserved sequence of four amino acids that is repeated twice in the cytoplasmic tails of non-catalytic tyrosine-phosphorylated receptors, cell-surface proteins found mainly on immune ce ...
s (ITAMs) present on the CD3 gamma, delta, epsilon, and zeta chains. The protein ZAP-70
ZAP-70 (Zeta-chain-associated protein kinase 70) is a protein normally expressed near the surface membrane of Lymphocyte, lymphocytes (T cells, natural killer cells, and a subset of B cell, B cells). It is most prominently known to be recruited u ...
can bind these phosphorylated ITAMs via its SH2 domain and then itself becomes phosphorylated, wherein it orchestrates the downstream signaling required for T cell activation. Lck activation is controlled by the opposing actions of CD45 and Csk. CD45 activates Lck by dephosphorylating a tyrosine in its C-terminal tail, while Csk phosphorylates Lck at that site. The loss of CD45 produces a form of SCID because failure to activate Lck prevents appropriate T cell signaling. Memory T cells also make use of this pathway and have higher levels of Lck expressed and the function of Csk is inhibited in these cells.
The binding of the antigen-MHC to the TCR complex and CD4 may also help the APC and the Th cell adhere during Th cell activation, but the integrin protein LFA-1 on the T cell and ICAM on the APC are the primary molecules of adhesion in this cell interaction.
It is unknown what role the relatively bulky extracellular region of CD45 plays during cell interactions, but CD45 has various isoforms that change in size depending on the Th cell's activation and maturation status. For example, CD45 shortens in length following Th activation (CD45RA+ to CD45RO+), but whether this change in length influences activation is unknown. It has been proposed that the larger CD45RA may decrease the accessibility of the T cell receptor for the antigen-MHC molecule, thereby necessitating an increase in the affinity (and specificity) of the T cell for activation. However, once the activation has occurred, CD45 shortens, allowing easier interactions and activation as an effector T helper cell.
Survival (signal 2)
Having received the first TCR/CD3 signal, the naïve T cell must activate a second independent biochemical pathway, known as Signal 2. This verification step is a protective measure to ensure that a T cell is responding to a foreign antigen. If this second signal is not present during initial antigen exposure, the T cell presumes that it is auto-reactive. This results in the cell becoming anergic (anergy is generated from the unprotected biochemical changes of Signal 1). Anergic cells will not respond to any antigen in the future, even if both signals are present later on. These cells are generally believed to circulate throughout the body with no value until they undergoapoptosis
Apoptosis (from ) is a form of programmed cell death that occurs in multicellular organisms and in some eukaryotic, single-celled microorganisms such as yeast. Biochemistry, Biochemical events lead to characteristic cell changes (Morphology (biol ...
.
The second signal involves an interaction between CD28
CD28 (Cluster of Differentiation 28) is a protein expressed on T cells that provides essential co-stimulation, co-stimulatory signals required for T cell activation and survival. When T cells are stimulated through CD28 in conjunction with the T- ...
on the CD4+ T cell and the proteins CD80
The Cluster of differentiation 80 (also CD80 and B7-1) is a B7, type I membrane protein in the immunoglobulin superfamily, with an extracellular immunoglobulin constant-like domain and a variable-like domain required for receptor binding. It is c ...
(B7.1) or CD86
Cluster of Differentiation 86 (also known as CD86 and B7-2) is a protein constitutively expressed on dendritic cells, Langerhans cells, macrophages, B-cells (including memory B-cells), and on other antigen-presenting cells. Along with CD80, CD ...
(B7.2) on the professional APCs. Both CD80 and CD86 activate the CD28 receptor. These proteins are also known as co-stimulatory molecules.
Although the verification stage is necessary for the activation of naïve helper T cells, the importance of this stage is best demonstrated during the similar activation mechanism of CD8+ cytotoxic T cell
A cytotoxic T cell (also known as TC, cytotoxic T lymphocyte, CTL, T-killer cell, cytolytic T cell, CD8+ T-cell or killer T cell) is a T lymphocyte (a type of white blood cell) that kills cancer cells, cells that are infected by intracellular ...
s. As naïve CD8+ T cells have no true bias towards foreign sources, these T cells must rely on the activation of CD28 for confirmation that they recognize a foreign antigen (as CD80/CD86 is only expressed by active APC's). CD28 plays an important role in decreasing the risk of T cell auto-immunity against host antigens.
Once the naïve T cell has both pathways activated, the biochemical changes induced by Signal 1 are altered, allowing the cell to activate instead of undergoing anergy. The second signal is then obsolete; only the first signal is necessary for future activation. This is also true for memory T cells, which is one example of learned immunity. Faster responses occur upon reinfection because memory T cells have already undergone confirmation and can produce effector cells much sooner.
Differentiation (signal 3)
Once the two-signal activation is complete the T helper cell (Th) then allows itself to proliferate. It achieves this by releasing a potent T cell growth factor calledinterleukin 2
Interleukin-2 (IL-2) is an interleukin, which is a type of cytokine signaling molecule forming part of the immune system. It is a 15.5–16 Dalton (unit), kDa protein that regulates the activities of white blood cells (leukocytes, often ...
(IL-2) which acts upon itself in an autocrine
Autocrine signaling is a form of cell signaling in which a cell secretes a hormone or chemical messenger (called the autocrine agent) that binds to autocrine receptors on that same cell, leading to changes in the cell. This can be contrasted with ...
fashion. Activated T cells also produce the alpha sub-unit of the IL-2 receptor ( CD25 or IL-2R), enabling a fully functional receptor that can bind with IL-2, which in turn activates the T cell's proliferation pathways.
The autocrine
Autocrine signaling is a form of cell signaling in which a cell secretes a hormone or chemical messenger (called the autocrine agent) that binds to autocrine receptors on that same cell, leading to changes in the cell. This can be contrasted with ...
or paracrine
In cellular biology, paracrine signaling is a form of cell signaling, a type of cellular communication (biology), cellular communication in which a Cell (biology), cell produces a signal to induce changes in nearby cells, altering the behaviour of ...
secretion of IL-2 can bind to that same Th cell or neighboring Th's via the IL-2R thus driving proliferation and clonal expansion. The Th cells receiving both signals of activation and proliferation will then become Th0 (T helper 0) cells that secrete IL-2, IL-4 and interferon gamma
Interferon gamma (IFNG or IFN-γ) is a dimerized soluble cytokine that is the only member of the type II class of interferons. The existence of this interferon, which early in its history was known as immune interferon, was described by E. F. ...
(IFN-γ). The Th0 cells will then differentiate into Th1 or Th2 cells depending on cytokine
Cytokines () are a broad and loose category of small proteins (~5–25 kDa) important in cell signaling.
Cytokines are produced by a broad range of cells, including immune cells like macrophages, B cell, B lymphocytes, T cell, T lymphocytes ...
environment. IFN-γ drives Th1 cell production while IL-10 and IL-4 inhibit Th1 cell production. Conversely, IL-4 drives Th2 cell production and IFN-γ inhibits Th2 cells. These cytokines are pleiotropic and carry out many other functions of the immune response.
Effector function
In 1991, three groups reported discovering CD154, which is the molecular basis of T cell helper function. Seth Lederman atColumbia University
Columbia University in the City of New York, commonly referred to as Columbia University, is a Private university, private Ivy League research university in New York City. Established in 1754 as King's College on the grounds of Trinity Churc ...
generated a murine monoclonal antibody, 5c8 that inhibited contact-dependent T cell helper function in human cells which characterized the 32 kDa surface protein transiently expressed on CD4+ T cells. Richard Armitage at Immunex cloned a cDNA encoding CD154 by screening an expression library with CD40-Ig. Randolph Noelle at Dartmouth Medical School generated an antibody that bound a 39 kDa protein on murine T cells and inhibited helper function.
Determination of the effector T cell response
Helper T cells are capable of influencing a variety of immune cells, and the T cell response generated (including theextracellular
This glossary of biology terms is a list of definitions of fundamental terms and concepts used in biology, the study of life and of living organisms. It is intended as introductory material for novices; for more specific and technical definitions ...
signals such as cytokine
Cytokines () are a broad and loose category of small proteins (~5–25 kDa) important in cell signaling.
Cytokines are produced by a broad range of cells, including immune cells like macrophages, B cell, B lymphocytes, T cell, T lymphocytes ...
s) can be essential for a successful outcome from infection. In order to be effective, helper T cells must determine which cytokines will allow the immune system to be most useful or beneficial for the host. Understanding exactly how helper T cells respond to immune challenges is currently of major interest in immunology
Immunology is a branch of biology and medicine that covers the study of Immune system, immune systems in all Organism, organisms.
Immunology charts, measures, and contextualizes the Physiology, physiological functioning of the immune system in ...
, because such knowledge may be very useful in the treatment of disease and in increasing the effectiveness of vaccination
Vaccination is the administration of a vaccine to help the immune system develop immunity from a disease. Vaccines contain a microorganism or virus in a weakened, live or killed state, or proteins or toxins from the organism. In stimulating ...
.
Th1/Th2 model
Proliferating helper T cells that develop into effector T cells differentiate into two major subtypes of cells known as Th1 and Th2 cells (also known as Type 1 and Type 2 helper T cells, respectively). Th1 helper cells lead to an increased cell-mediated response (primarily bymacrophage
Macrophages (; abbreviated MPhi, φ, MΦ or MP) are a type of white blood cell of the innate immune system that engulf and digest pathogens, such as cancer cells, microbes, cellular debris and foreign substances, which do not have proteins that ...
s and cytotoxic T cell
A cytotoxic T cell (also known as TC, cytotoxic T lymphocyte, CTL, T-killer cell, cytolytic T cell, CD8+ T-cell or killer T cell) is a T lymphocyte (a type of white blood cell) that kills cancer cells, cells that are infected by intracellular ...
s), typically against intracellular bacteria and protozoa. They are triggered by the polarising cytokine IL-12 and their effector cytokines are IFN-γ and IL-2. The main effector cells of Th1 immunity are macrophages as well as CD8 T cells, IgG B cells, and IFN-γ CD4 T cells. The key Th1 transcription factors are STAT4 and T-bet. IFN-γ secreted by CD4 T cells can activate macrophages to phagocytose and digest intracellular bacteria and protozoa. In addition, IFN-γ can activate iNOS
Nitric oxide synthases (NOSs) are a family of enzymes catalyzing the production of nitric oxide (NO) from L-arginine. NO is an important cellular signaling molecule. It helps modulate vascular tone, insulin secretion, airway tone, and perist ...
(inducible nitric oxide synthase) to produce nitric oxide free radicals to directly kill intracellular bacteria and protozoa. Th1 overactivation against autoantigens will cause Type IV or delayed-type hypersensitivity reaction. Tuberculin reaction and Type 1 diabetes belong to this category of autoimmunity.
Th2 helper cells lead to a humoral immune response
Humoral immunity is the aspect of immunity that is mediated by macromolecules – including secreted antibodies, complement proteins, and certain antimicrobial peptides – located in extracellular fluids. Humoral immunity is named so because ...
, typically against extracellular parasites such as helminths
Parasitic worms, also known as helminths, are a polyphyletic group of large macroparasites; adults can generally be seen with the naked eye. Many are intestinal worms that are soil-transmitted and infect the gastrointestinal tract. Other par ...
. They are triggered by the polarising cytokines IL-4 and IL-2, and their effector cytokines are IL-4, IL-5, IL-9, IL-10, IL-13 and IL-25. The main effector cells are eosinophils, basophils, and mast cells as well as B cells, and IL-4/IL-5 CD4 T cells. The key Th2 transcription factors are STAT6 and GATA3. IL-4 is the positive feedback cytokine for Th2 cells differentiation. Besides, IL-4 stimulates B-cells to produce IgE antibodies, which in turn stimulate mast cells to release histamine
Histamine is an organic nitrogenous compound involved in local immune responses communication, as well as regulating physiological functions in the gut and acting as a neurotransmitter for the brain, spinal cord, and uterus. Discovered in 19 ...
, serotonin
Serotonin (), also known as 5-hydroxytryptamine (5-HT), is a monoamine neurotransmitter with a wide range of functions in both the central nervous system (CNS) and also peripheral tissues. It is involved in mood, cognition, reward, learning, ...
, and leukotriene to cause broncho-constriction, intestinal peristalsis, gastric fluid acidification to expel helminths. IL-5 from CD4 T cells will activate eosinophils to attack helminths. IL-10 suppresses Th1 cells differentiation and function of dendritic cells. Th2 overactivation against antigen will cause Type I hypersensitivity
Type I hypersensitivity (or immediate hypersensitivity), in the Hypersensitivity, Gell and Coombs classification of allergic reactions, is an allergic reaction provoked by re-exposure to a specific type of antigen referred to as an allergen. Type ...
which is an allergic reaction mediated by IgE. Allergic rhinitis, atopic dermatitis, and asthma belong to this category of overactivation . In addition to expressing different cytokines, Th2 cells also differ from Th1 cells in their cell surface glycans (oligosaccharides), which makes them less susceptible to some inducers of cell death.
While we know about the types of cytokine patterns helper T cells tend to produce, we understand less about how the patterns themselves are decided. Various evidence suggests that the type of APC presenting the antigen to the T cell has a major influence on its profile. Other evidence suggests that the concentration of antigen presented to the T cell during primary activation influences its choice. The presence of some cytokines (such as the ones mentioned above) will also influence the response that will eventually be generated, but our understanding is nowhere near complete.
Th17 helper cells
Th17 helper cells are a subset of T helper cells developmentally distinct from Th1 and Th2 lineages. Th17 cells produce interleukin 17 (IL-17), a pro-inflammatory substance, as well as interleukins 21 and 22. This means that Th17 cells are especially good at fighting extracellular pathogens and fungi, particularly during mucocutaneous immunity against '' Candida'' spp.THαβ helper cells
THαβ helper cells provide the host immunity against viruses. Their differentiation is triggered by IFN α/β or IL-10. Their key effector cytokine is IL-10. Their main effector cells are NK cells as well as CD8 T cells, IgG B cells, and IL-10 CD4 T cells. The key THαβ transcription factors are STAT1 and STAT3 as well as IRFs. IL-10 from CD4 T cells activate NK cells' ADCC to apoptose virus-infected cells and to induce host as well as viral DNA fragmentation. IFN alpha/beta can suppress transcription to avoid virus replication and transmission. Overactivation of THαβ against autoantigen will cause type 2 antibody-dependent cytotoxic hypersensitivity.Myasthenia gravis
Myasthenia gravis (MG) is a long-term neuromuscular junction disease that leads to varying degrees of skeletal muscle weakness. The most commonly affected muscles are those of the eyes, face, and swallowing. It can result in double vision, ...
or Graves' disease
Graves' disease, also known as toxic diffuse goiter or Basedow's disease, is an autoimmune disease that affects the thyroid. It frequently results in and is the most common cause of hyperthyroidism. It also often results in an enlarged thyro ...
belong to this category.
Limitations to the Th1/Th2 model
The interactions between cytokines from the Th1/Th2 model can be more complicated in some animals. For example, the Th2 cytokine IL-10 inhibits cytokine production of both Th subsets in humans. Human IL-10 (hIL-10) suppresses the proliferation and cytokine production of all T cells and the activity of macrophages, but continues to stimulate plasma cells, ensuring that antibody production still occurs. As such, hIL-10 is not believed to truly promote the Th2 response in humans, but acts to prevent over-stimulation of helper T cells while still maximising the production ofantibodies
An antibody (Ab) or immunoglobulin (Ig) is a large, Y-shaped protein belonging to the immunoglobulin superfamily which is used by the immune system to identify and neutralize antigens such as bacteria and viruses, including those that caus ...
.There are also other types of T cells that can influence the expression and activation of helper T cells, such as natural regulatory T cells
The regulatory T cells (Tregs or Treg cells), formerly known as suppressor T cells, are a subpopulation of T cells that modulate the immune system, maintain immune tolerance, tolerance to self-antigens, and prevent autoimmune disease. Treg ...
, along with less common cytokine profiles such as the Th3 subset of helper T cells. Terms such as "regulatory" and "suppression" have become ambiguous after the discovery that helper CD4+ T cells are also capable of regulating (and suppressing) their own responses outside of dedicated regulatory T cells.
One major difference between regulatory T cells and effector T cells is that regulatory T cells typically serve to modulate and deactivate the immune response, while effector T cell groups usually begin with immune-promoting cytokines and then switch to inhibitory cytokines later in their life cycle. The latter is a feature of Th3 cells, which transform into a regulatory subset after its initial activation and cytokine production.
Both regulatory T cells
The regulatory T cells (Tregs or Treg cells), formerly known as suppressor T cells, are a subpopulation of T cells that modulate the immune system, maintain immune tolerance, tolerance to self-antigens, and prevent autoimmune disease. Treg ...
and Th3 cells produce the cytokine transforming growth factor-beta (TGF-β) and IL-10. Both cytokines are inhibitory to helper T cells; TGF-β suppresses the activity of most of the immune system. There is evidence to suggest that TGF-β may not suppress activated Th2 cells as effectively as it might suppress naive cells, but it is not typically considered a Th2 cytokine.
The novel characterisation of another T helper subtype, T helper 17 cells (Th17) has cast further doubt on the basic Th1/Th2 model. These IL-17 producing cells were initially described as a pathogenic population implicated in autoimmunity but are now thought to have their own distinct effector and regulatory functions. Of note, some evidence suggest that functional plasticity is an intrinsic capacity of T helper cells. Indeed, a study in mice demonstrated that Th17 cells transform into Th1 cells ''in vivo''. A subsequent study furthermore showed that extensive T helper cell plasticity is also prominent in humans.
Many of the cytokines in this article are also expressed by other immune cells (see individual cytokines for details), and it is becoming clear that while the original Th1/Th2 model is enlightening and gives insight into the functions of helper T cells, it is far too simple to define its entire role or actions. Some immunologists question the model completely, as some ''in vivo'' studies suggest that individual helper T cells usually do not match the specific cytokine profiles of the Th model, and many cells express cytokines from both profiles. That said, the Th model has still played an important part in developing our understanding of the roles and behaviour of helper T cells and the cytokines they produce during an immune response.
Studies by Stockinger et al. revealed that another T helper subset may exist. Th9 cells are claimed to be an IL9 ( interleukin 9)–producing T cell subset focused on defending helminth infections.
Memory T cell
Historically, memory T cells were thought to belong to either the effector or central memory subtypes, each with their own distinguishing set of cell surface markers. Central memory T cells reside in the lymph nodes while effector memory T cells lack the C-C chemokine receptor type 7 (CCR7) and L-selectin (CD62L) receptors, which prevents them from trafficking to the lymph nodes. Additional populations of memory T cells are now known to exist. These include tissue-resident memory T (Trm) cells and virtual memory T cells. The single unifying theme for all memory T cell subtypes is that they are long-lived and can expand quickly to large numbers of effector T cells upon encountering their cognate antigen. By this mechanism they provide the immune system with "memory" against previously encountered pathogens.Role in disease
Considering the diverse and important role helper T cells play in the immune system, it is not surprising that these cells often influence the immune response against disease. They also occasionally generate non-beneficial responses. Very rarely, the helper T cell response could lead to the death of the host.Antitumor immunity
Hypersensitivity
The immune system must achieve a balance of sensitivity in order to respond to foreign antigens without responding to the antigens of the host itself. When the immune system responds to very low levels of antigen that it usually shouldn't respond to, ahypersensitivity
Hypersensitivity (also called hypersensitivity reaction or intolerance) is an abnormal physiological condition in which there is an undesirable and adverse immune response to an antigen. It is an abnormality in the immune system that causes Imm ...
response occurs. Hypersensitivity is believed to be the cause of allergy
Allergies, also known as allergic diseases, are various conditions caused by hypersensitivity of the immune system to typically harmless substances in the environment. These diseases include Allergic rhinitis, hay fever, Food allergy, food al ...
and some auto-immune disease.
Hypersensitivity reactions can be divided into four types:
* Type 1 hypersensitivity includes common immune disorders such as asthma
Asthma is a common long-term inflammatory disease of the airways of the lungs. It is characterized by variable and recurring symptoms, reversible airflow obstruction, and easily triggered bronchospasms. Symptoms include episodes of wh ...
, allergic rhinitis
Allergic rhinitis, of which the seasonal type is called hay fever, is a type of inflammation in the nose that occurs when the immune system overreacts to allergens in the air. It is classified as a type I hypersensitivity reaction. Signs a ...
(hay fever), eczema
Dermatitis is a term used for different types of skin inflammation, typically characterized by itchiness, redness and a rash. In cases of short duration, there may be small blisters, while in long-term cases the skin may become thickened ...
, urticaria
Hives, also known as urticaria, is a kind of skin rash with red or flesh-colored, raised, itchy bumps. Hives may burn or sting. The patches of rash may appear on different body parts, with variable duration from minutes to days, and typically ...
(hives) and anaphylaxis
Anaphylaxis (Greek: 'up' + 'guarding') is a serious, potentially fatal allergic reaction and medical emergency that is rapid in onset and requires immediate medical attention regardless of the use of emergency medication on site. It typicall ...
. These reactions all involve IgE antibodies
An antibody (Ab) or immunoglobulin (Ig) is a large, Y-shaped protein belonging to the immunoglobulin superfamily which is used by the immune system to identify and neutralize antigens such as bacteria and viruses, including those that caus ...
, which require a Th2 response during helper T cell development. Preventive treatments, such as corticosteroids
Corticosteroids are a class of steroid hormones that are produced in the adrenal cortex of vertebrates, as well as the synthetic analogues of these hormones. Two main classes of corticosteroids, glucocorticoids and mineralocorticoids, are invol ...
and montelukast
Montelukast, sold under the brand name Singulair among others, is a medication used in the maintenance treatment of asthma. It is generally less preferred for this use than inhaled corticosteroids. It is not useful for acute asthma attacks. ...
, focus on suppressing mast cells or other allergic cells; T cells do not play a primary role during the actual inflammatory response. It's important to note that the numeral allocation of hypersensitivity "types" does not correlate (and is completely unrelated) to the "response" in the Th model.
* Type 2 and Type 3 hypersensitivity both involve complications from auto-immune or low affinity antibodies. In both of these reactions, T cells may play an accomplice role in generating these auto-specific antibodies, although some of these reactions under Type 2 hypersensitivity would be considered normal in a healthy immune system (for example, Rhesus factor reactions during child-birth is a normal immune response against child antigens). The understanding of the role of helper T cells in these responses is limited but it is generally thought that Th2 cytokines would promote such disorders. For example, studies have suggested that lupus
Lupus, formally called systemic lupus erythematosus (SLE), is an autoimmune disease in which the body's immune system mistakenly attacks healthy tissue in many parts of the body. Symptoms vary among people and may be mild to severe. Common ...
(SLE) and other auto-immune diseases of similar nature can be linked to the production of Th2 cytokines.
* Type 4 hypersensitivity, also known as delayed type hypersensitivity, are caused via the over-stimulation of immune cells, commonly lymphocytes
A lymphocyte is a type of white blood cell (leukocyte) in the immune system of most vertebrates. Lymphocytes include T cells (for cell-mediated and cytotoxic adaptive immunity), B cells (for humoral, antibody-driven adaptive immunity), and ...
and macrophages
Macrophages (; abbreviated MPhi, φ, MΦ or MP) are a type of white blood cell of the innate immune system that engulf and digest pathogens, such as cancer cells, microbes, cellular debris and foreign substances, which do not have proteins that ...
, resulting in chronic inflammation
Inflammation (from ) is part of the biological response of body tissues to harmful stimuli, such as pathogens, damaged cells, or irritants. The five cardinal signs are heat, pain, redness, swelling, and loss of function (Latin ''calor'', '' ...
and cytokine release. Antibodies do not play a direct role in this allergy type. T cells play an important role in this hypersensitivity, as they activate against the stimulus itself and promote the activation of other cells; particularly macrophages via Th1 cytokines.
Other cellular hypersensitivities include cytotoxic T cell
A cytotoxic T cell (also known as TC, cytotoxic T lymphocyte, CTL, T-killer cell, cytolytic T cell, CD8+ T-cell or killer T cell) is a T lymphocyte (a type of white blood cell) that kills cancer cells, cells that are infected by intracellular ...
mediated auto-immune disease, and a similar phenomenon; transplant rejection
Transplant rejection occurs when transplanted tissue is rejected by the recipient's immune system, which destroys the transplanted tissue. Transplant rejection can be lessened by determining the molecular similitude between donor and recipien ...
. Helper T cells are required to fuel the development of these diseases. In order to create sufficient auto-reactive killer T cells, interleukin-2
Interleukin-2 (IL-2) is an interleukin, which is a type of cytokine signaling molecule forming part of the immune system. It is a 15.5–16 kDa protein that regulates the activities of white blood cells (leukocytes, often lymphocytes) ...
must be produced, and this is supplied by CD4+ T cells. CD4+ T cells can also stimulate cells such as natural killer cell
Natural killer cells, also known as NK cells, are a type of cytotoxic lymphocyte critical to the innate immune system. They are a kind of large granular lymphocytes (LGL), and belong to the rapidly expanding family of known innate lymphoid cells ...
s and macrophages via cytokines such as interferon-gamma
Interferon gamma (IFNG or IFN-γ) is a dimerized soluble cytokine that is the only member of the type II class of interferons. The existence of this interferon, which early in its history was known as immune interferon, was described by E. F. ...
, encouraging these cytotoxic cells to kill host cells in certain circumstances.
The mechanism that killer T cells use during auto-immunity is almost identical to their response against viruses
A virus is a submicroscopic infectious agent that replicates only inside the living cells of an organism. Viruses infect all life forms, from animals and plants to microorganisms, including bacteria and archaea. Viruses are found in almo ...
, and some viruses have been accused of causing auto-immune diseases such as Type 1 diabetes mellitus. Cellular auto-immune disease occurs because the host antigen recognition systems fail, and the immune system
The immune system is a network of biological systems that protects an organism from diseases. It detects and responds to a wide variety of pathogens, from viruses to bacteria, as well as Tumor immunology, cancer cells, Parasitic worm, parasitic ...
believes, by mistake, that a host antigen is foreign. As a result, the CD8+ T cells treat the host cell presenting that antigen as infected, and go on to destroy all host cells (or in the case of transplant rejection, transplant organ) that express that antigen.
Some of this section is a simplification. Many auto-immune diseases are more complex. A well-known example is rheumatoid arthritis
Rheumatoid arthritis (RA) is a long-term autoimmune disorder that primarily affects synovial joint, joints. It typically results in warm, swollen, and painful joints. Pain and stiffness often worsen following rest. Most commonly, the wrist and h ...
, where both antibodies and immune cells are known to play a role in the pathology. Generally the immunology of most auto-immune diseases is not well understood.
HIV infection
Perhaps the best example of the importance of CD4+ T cells is demonstrated withhuman immunodeficiency virus
The human immunodeficiency viruses (HIV) are two species of ''Lentivirus'' (a subgroup of retrovirus) that infect humans. Over time, they cause AIDS, acquired immunodeficiency syndrome (AIDS), a condition in which progressive failure of th ...
(HIV) infection. HIV mainly targets lymphoid CD4+ T cells, but can infect other cells that express CD4 such as macrophages
Macrophages (; abbreviated MPhi, φ, MΦ or MP) are a type of white blood cell of the innate immune system that engulf and digest pathogens, such as cancer cells, microbes, cellular debris and foreign substances, which do not have proteins that ...
and dendritic cells
A dendritic cell (DC) is an antigen-presenting cell (also known as an ''accessory cell'') of the mammalian immune system. A DC's main function is to process antigen material and present it on the cell surface to the T cells of the immune system ...
(both groups express CD4 at low levels).
It has been proposed that during the non-symptomatic phase of HIV infection, the virus has a relatively low affinity towards T cells (and has a higher affinity for macrophages), resulting in a slow kill rate of CD4+ T cells by the immune system. This is initially compensated for via the production of new helper T cells from the thymus
The thymus (: thymuses or thymi) is a specialized primary lymphoid organ of the immune system. Within the thymus, T cells mature. T cells are critical to the adaptive immune system, where the body adapts to specific foreign invaders. The thymus ...
(originally from the bone marrow
Bone marrow is a semi-solid biological tissue, tissue found within the Spongy bone, spongy (also known as cancellous) portions of bones. In birds and mammals, bone marrow is the primary site of new blood cell production (or haematopoiesis). It i ...
). Once the virus becomes lymphotropic (or T-tropic) however, it begins to infect CD4+ T cells far more efficiently (likely due to a change in the co-receptor
A co-receptor is a cell surface receptor that binds a signalling molecule in addition to a primary receptor in order to facilitate Ligand (biochemistry), ligand recognition and initiate biological processes, such as entry of a pathogen into a host ...
s it binds to during infection), and the immune system is overwhelmed. Studies suggest that only ~5% of the lymphoid-derived CD4 T cells targeted by HIV are permissive and become productively infected with the virus. More than 95% of the CD4 T cells that die are resting and are unable to support productive infection. These cells undergo abortive infection with HIV. Cell death is triggered when the host cell detects HIV foreign DNA intermediates and initiates a suicidal death pathway in an attempt to protect the host, leading to caspase-1 activation in inflammasomes, thus causing pyroptosis (a highly inflammatory form of programmed cell death).
At this point chronic inflammation ensues, and functional CD4+ T cell levels begin to decrease, eventually to a point where the CD4+ T cell population is too small to recognize the full range of antigen
In immunology, an antigen (Ag) is a molecule, moiety, foreign particulate matter, or an allergen, such as pollen, that can bind to a specific antibody or T-cell receptor. The presence of antigens in the body may trigger an immune response.
...
s that could potentially be detected. The depletion of CD4 T cells and the development of chronic inflammation are signature processes in HIV pathogenesis that propel progression to acquired immune deficiency syndrome (AIDS). CD4 T cell depleted to the cell count of less than 200cell/μL in blood during AIDS allows various pathogens
In biology, a pathogen (, "suffering", "passion" and , "producer of"), in the oldest and broadest sense, is any organism or agent that can produce disease. A pathogen may also be referred to as an infectious agent, or simply a germ.
The term ...
to escape T cell recognition, thus allowing opportunistic infection
An opportunistic infection is an infection that occurs most commonly in individuals with an immunodeficiency disorder and acts more severe on those with a weakened immune system. These types of infections are considered serious and can be caused b ...
s that would normally elicit a helper T cell response to bypass the immune system. While these complete bypass situations only occur when the helper T cell response is absolutely necessary for infection clearance, most infections increase in severity and/or duration because the immune system's helper T cells provide less efficient immune response.
Two components of the immune system are particularly affected in AIDS, due to its CD4+ T cell dependency:
# CD8
CD8 (cluster of differentiation 8) is a transmembrane protein, transmembrane glycoprotein that serves as a co-receptor for the T-cell receptor (TCR). Along with the TCR, the CD8 co-receptor plays a role in T cell Cell signaling, signaling and aid ...
+ T cells are not stimulated as effectively during the AIDS stage of HIV infection, making AIDS patients very susceptible to most viruses, including HIV itself. This decline in killing of CD4+ T cells results in the virus being produced for a longer period (the infected CD4+ T cells are not killed as quickly), increasing the proliferation of the virus, and accelerating the development of the disease.
# Antibody class switching declines significantly once helper T cell function fails. The immune system loses its ability to improve the affinity of their antibodies, and are unable to generate B cells that can produce antibody groups such as IgG and IgA. These effects are primarily due to the loss of any helper T cell that can interact with the B lymphocyte correctly. Another symptom of AIDS is the reduction in antibody levels due to a decrease in Th2 cytokines (and less interactions by helper T cells). All of these complications result in an increased susceptibility to aggressive bacterial infections, especially in areas of the body not accessible by IgM antibodies.
If the patient does not respond to (or does not receive) HIV treatment
The human immunodeficiency viruses (HIV) are two species of '' Lentivirus'' (a subgroup of retrovirus) that infect humans. Over time, they cause acquired immunodeficiency syndrome (AIDS), a condition in which progressive failure of the im ...
they will succumb usually to either cancers or infections; the immune system finally reaches a point where it is no longer coordinated or stimulated enough to deal with the disease.
Inhibition of CD4 T-cell expansion during HIV infection may occur due to microbial translocation in an IL-10-dependent way. Triggering PD-1 expressed on activated monocytes by its ligand PD-L1, induces IL-10 production which inhibits CD4 T-cell function.
COVID-19
Incoronavirus disease 2019
Coronavirus disease 2019 (COVID-19) is a contagious disease caused by the coronavirus SARS-CoV-2. In January 2020, the disease spread worldwide, resulting in the COVID-19 pandemic.
The symptoms of COVID‑19 can vary but often include f ...
(COVID-19) B cell
B cells, also known as B lymphocytes, are a type of the lymphocyte subtype. They function in the humoral immunity component of the adaptive immune system. B cells produce antibody molecules which may be either secreted or inserted into the plasm ...
, natural killer cell
Natural killer cells, also known as NK cells, are a type of cytotoxic lymphocyte critical to the innate immune system. They are a kind of large granular lymphocytes (LGL), and belong to the rapidly expanding family of known innate lymphoid cells ...
, and total lymphocyte
A lymphocyte is a type of white blood cell (leukocyte) in the immune system of most vertebrates. Lymphocytes include T cells (for cell-mediated and cytotoxic adaptive immunity), B cells (for humoral, antibody-driven adaptive immunity), an ...
counts decline, but both CD4+ and CD8+ cells decline to a far greater extent. Indicating that SARS-Cov-2
Severe acute respiratory syndrome coronavirus 2 (SARS‑CoV‑2) is a strain of coronavirus that causes COVID-19, the respiratory illness responsible for the COVID-19 pandemic. The virus previously had the Novel coronavirus, provisional nam ...
attacks the CD4+ cells during infection. Low CD4+ predicted greater likelihood of intensive care unit
An intensive care unit (ICU), also known as an intensive therapy unit or intensive treatment unit (ITU) or critical care unit (CCU), is a special department of a hospital or health care facility that provides intensive care medicine.
An inten ...
admission, and CD4+ cell count was the only parameter that predicted length of time for viral RNA
Ribonucleic acid (RNA) is a polymeric molecule that is essential for most biological functions, either by performing the function itself (non-coding RNA) or by forming a template for the production of proteins (messenger RNA). RNA and deoxyrib ...
clearance. Despite the reduced levels of CD4+, COVID-19 patients with severe disease had higher levels of Th1 CD4+ cells than patients with moderate disease. It is noted that SARS-Cov-2 does reverse transcriptase
A reverse transcriptase (RT) is an enzyme used to convert RNA genome to DNA, a process termed reverse transcription. Reverse transcriptases are used by viruses such as HIV and hepatitis B to replicate their genomes, by retrotransposon mobi ...
like HIV against these cells.
See also
* CD4+/CD8+ ratio * CD4+ T cells and antitumor immunity * CD8+ T cells * Cancer vaccine targeting CD4+ T cells *List of distinct cell types in the adult human body
The list of human cell types provides an enumeration and description of the various specialized cells found within the human body, highlighting their distinct functions, characteristics, and contributions to overall physiological processes. Cell ...
References
Further reading
* *External links
* {{DEFAULTSORT:T Helper Cell Helper Human cells Phagocytes Cell biology Immune system Lymphatic system Infectious diseases Cell signaling