Polymorphic Ventricular Tachycardia on:
[Wikipedia]
[Google]
[Amazon]
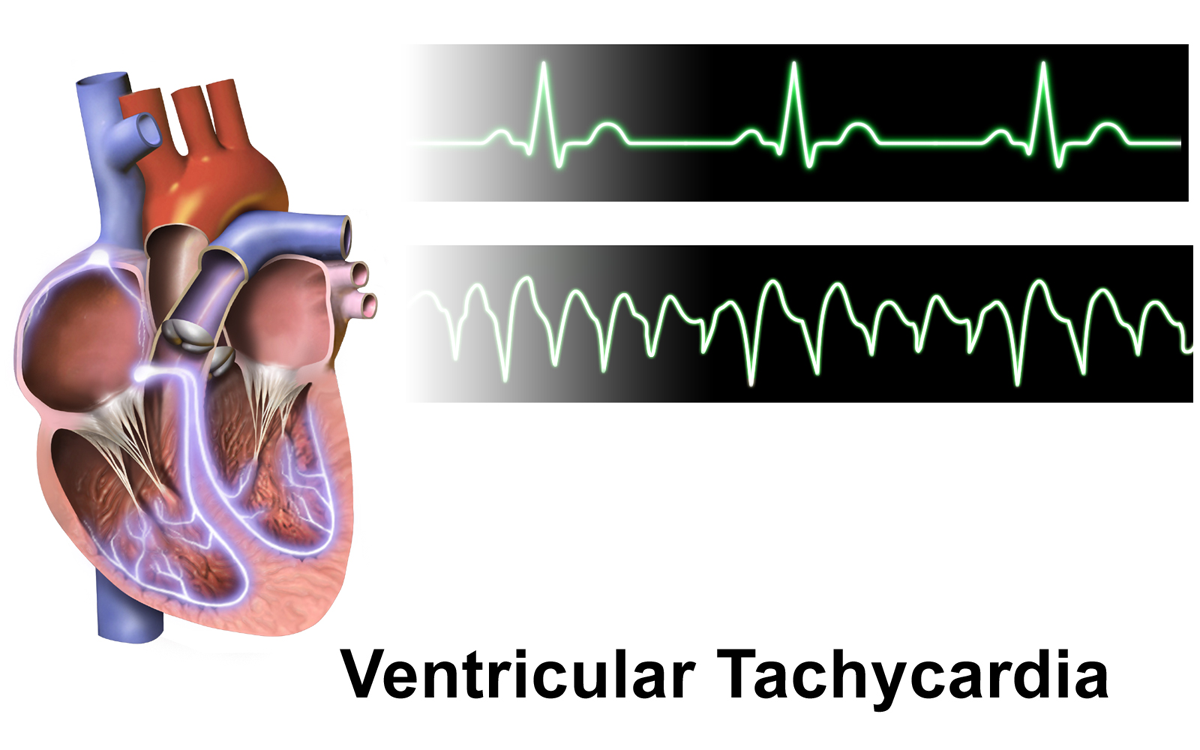
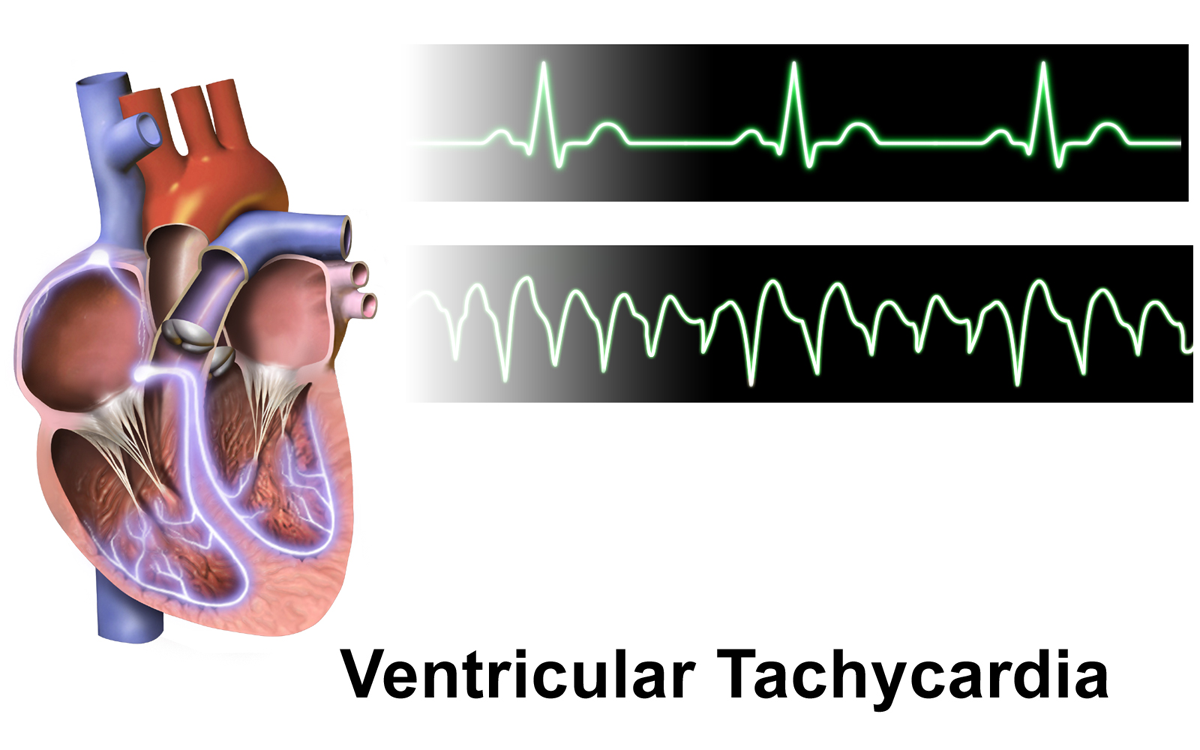
Ventricular tachycardia (V-tach or VT) is a cardiovascular disorder in which fast heart rate occurs in the ventricles of the
 Ventricular tachycardia can be classified based on its ''morphology'':
* Monomorphic ventricular tachycardia means that the appearance of all the beats match each other in each lead of a surface electrocardiogram (ECG).
** Scar-related monomorphic ventricular tachycardia is the most common type and a frequent cause of death in patients having survived a heart attack, especially if they have weak heart muscle.
** Right ventricular outflow tract (RVOT) tachycardia is a type of monomorphic ventricular tachycardia originating in the right ventricular outflow tract. RVOT morphology refers to the characteristic pattern of this type of tachycardia on an ECG.
** The source of the re-entry circuit can be identified by evaluating the morphology of the QRS complex in the V1 lead of a surface ECG. If the R wave is dominant (consistent with a
Ventricular tachycardia can be classified based on its ''morphology'':
* Monomorphic ventricular tachycardia means that the appearance of all the beats match each other in each lead of a surface electrocardiogram (ECG).
** Scar-related monomorphic ventricular tachycardia is the most common type and a frequent cause of death in patients having survived a heart attack, especially if they have weak heart muscle.
** Right ventricular outflow tract (RVOT) tachycardia is a type of monomorphic ventricular tachycardia originating in the right ventricular outflow tract. RVOT morphology refers to the characteristic pattern of this type of tachycardia on an ECG.
** The source of the re-entry circuit can be identified by evaluating the morphology of the QRS complex in the V1 lead of a surface ECG. If the R wave is dominant (consistent with a
Ventricular Tachycardia (Free ECG book)
{{Authority control Cardiac arrhythmia Wikipedia medicine articles ready to translate Wikipedia emergency medicine articles ready to translate
heart
The heart is a muscular Organ (biology), organ found in humans and other animals. This organ pumps blood through the blood vessels. The heart and blood vessels together make the circulatory system. The pumped blood carries oxygen and nutrie ...
. Although a few seconds of VT may not result in permanent problems, longer periods are dangerous; and multiple episodes over a short period of time are referred to as an electrical storm. Short periods may occur without symptoms, or present with lightheadedness, palpitations
Palpitations occur when a person becomes aware of their heartbeat. The heartbeat may feel hard, fast, or uneven in their chest.
Symptoms include a very fast or irregular heartbeat. Palpitations are a sensory symptom. They are often described as ...
, shortness of breath
Shortness of breath (SOB), known as dyspnea (in AmE) or dyspnoea (in BrE), is an uncomfortable feeling of not being able to breathe well enough. The American Thoracic Society defines it as "a subjective experience of breathing discomfort that con ...
, chest pain, and decreased level of consciousness. Ventricular tachycardia may lead to coma
A coma is a deep state of prolonged unconsciousness in which a person cannot be awakened, fails to Nociception, respond normally to Pain, painful stimuli, light, or sound, lacks a normal Circadian rhythm, sleep-wake cycle and does not initiate ...
and persistent vegetative state
A vegetative state (VS) or post-coma unresponsiveness (PCU) is a disorder of consciousness in which patients with severe brain damage are in a state of partial arousal rather than true awareness. After four weeks in a vegetative state, the patie ...
due to lack of blood and oxygen to the brain. Ventricular tachycardia may result in ventricular fibrillation
Ventricular fibrillation (V-fib or VF) is an abnormal heart rhythm in which the Ventricle (heart), ventricles of the heart Fibrillation, quiver. It is due to disorganized electrical conduction system of the heart, electrical activity. Ventricula ...
(VF) and turn into cardiac arrest
Cardiac arrest (also known as sudden cardiac arrest CA is when the heart suddenly and unexpectedly stops beating. When the heart stops beating, blood cannot properly Circulatory system, circulate around the body and the blood flow to the ...
. This conversion of the VT into VF is called the degeneration of the VT. It is found initially in about 7% of people in cardiac arrest.
Ventricular tachycardia can occur due to coronary heart disease, aortic stenosis, cardiomyopathy, electrolyte imbalance, or a heart attack
A myocardial infarction (MI), commonly known as a heart attack, occurs when Ischemia, blood flow decreases or stops in one of the coronary arteries of the heart, causing infarction (tissue death) to the heart muscle. The most common symptom ...
. Diagnosis is by an electrocardiogram (ECG) showing a rate of greater than 120 beats per minute and at least three wide QRS complexes in a row. It is classified as non-sustained versus sustained based on whether it lasts less than or more than 30 seconds. The term ventricular arrhythmia refers to the group of abnormal cardiac rhythms originating from the ventricle, which includes ventricular tachycardia, ventricular fibrillation, and torsades de pointes.
In those who have normal blood pressure
Blood pressure (BP) is the pressure of Circulatory system, circulating blood against the walls of blood vessels. Most of this pressure results from the heart pumping blood through the circulatory system. When used without qualification, the term ...
and strong pulse, the antiarrhythmic medication procainamide may be used. Otherwise, immediate cardioversion is recommended, preferably with a biphasic DC shock of 200 joules. In those in cardiac arrest due to ventricular tachycardia, cardiopulmonary resuscitation
Cardiopulmonary resuscitation (CPR) is an emergency procedure used during Cardiac arrest, cardiac or Respiratory arrest, respiratory arrest that involves chest compressions, often combined with artificial ventilation, to preserve brain function ...
(CPR) and defibrillation is recommended. Biphasic defibrillation may be better than monophasic. While waiting for a defibrillator, a precordial thump may be attempted (by those who have experience) in those on a heart monitor who are seen going into an unstable ventricular tachycardia. In those with cardiac arrest due to ventricular tachycardia, survival is about 75%. An implantable cardiac defibrillator or medications such as calcium channel blockers or amiodarone
Amiodarone is an antiarrhythmic medication used to treat and prevent a number of types of cardiac dysrhythmias. This includes ventricular tachycardia, ventricular fibrillation, and wide complex tachycardia, atrial fibrillation, and paroxys ...
may be used to prevent recurrence.
Signs and symptoms
While a few seconds may not result in problems, longer periods are dangerous. Short periods may occur without symptoms or present with lightheadedness,palpitations
Palpitations occur when a person becomes aware of their heartbeat. The heartbeat may feel hard, fast, or uneven in their chest.
Symptoms include a very fast or irregular heartbeat. Palpitations are a sensory symptom. They are often described as ...
, shortness of breath
Shortness of breath (SOB), known as dyspnea (in AmE) or dyspnoea (in BrE), is an uncomfortable feeling of not being able to breathe well enough. The American Thoracic Society defines it as "a subjective experience of breathing discomfort that con ...
, chest pain, or unconsciousness
Unconsciousness is a state in which a living individual exhibits a complete, or near-complete, inability to maintain an awareness of self and environment or to respond to any human or environmental stimulus. Unconsciousness may occur as the r ...
. Ventricular tachycardia may turn into ventricular fibrillation
Ventricular fibrillation (V-fib or VF) is an abnormal heart rhythm in which the Ventricle (heart), ventricles of the heart Fibrillation, quiver. It is due to disorganized electrical conduction system of the heart, electrical activity. Ventricula ...
and can result in cardiac arrest
Cardiac arrest (also known as sudden cardiac arrest CA is when the heart suddenly and unexpectedly stops beating. When the heart stops beating, blood cannot properly Circulatory system, circulate around the body and the blood flow to the ...
.
Cause
Ventricular tachycardia can occur due to coronary heart disease, aortic stenosis, cardiomyopathy, electrolyte problems (e.g., low blood levels of magnesium orpotassium
Potassium is a chemical element; it has Symbol (chemistry), symbol K (from Neo-Latin ) and atomic number19. It is a silvery white metal that is soft enough to easily cut with a knife. Potassium metal reacts rapidly with atmospheric oxygen to ...
), inherited channelopathies (e.g., long-QT syndrome), catecholaminergic polymorphic ventricular tachycardia, arrhythmogenic right ventricular dysplasia, alcohol withdrawal syndrome (typically following atrial fibrillation
Atrial fibrillation (AF, AFib or A-fib) is an Heart arrhythmia, abnormal heart rhythm (arrhythmia) characterized by fibrillation, rapid and irregular beating of the Atrium (heart), atrial chambers of the heart. It often begins as short periods ...
), or a myocardial infarction
A myocardial infarction (MI), commonly known as a heart attack, occurs when Ischemia, blood flow decreases or stops in one of the coronary arteries of the heart, causing infarction (tissue death) to the heart muscle. The most common symptom ...
.
Pathophysiology
The morphology of the tachycardia depends on its cause and the origin of the re-entry electrical circuit in the heart. In monomorphic ventricular tachycardia, the shape of each heart beat on the ECG looks the same because the impulse is either being generated from increased automaticity of a single point in either the left or the right ventricle, or due to a reentry circuit within the ventricle. The most common cause of monomorphic ventricular tachycardia is scarring of the heart muscle from a previousmyocardial infarction
A myocardial infarction (MI), commonly known as a heart attack, occurs when Ischemia, blood flow decreases or stops in one of the coronary arteries of the heart, causing infarction (tissue death) to the heart muscle. The most common symptom ...
(heart attack). This scar cannot conduct electrical activity, so there is a potential circuit ''around'' the scar that results in the tachycardia. This is similar to the re-entrant circuits that are the cause of atrial flutter and the re-entrant forms of supraventricular tachycardia. Other rarer congenital causes of monomorphic VT include right ventricular dysplasia, and right and left ventricular outflow tract VT.
Polymorphic ventricular tachycardia, on the other hand, is most commonly caused by abnormalities of ventricular muscle repolarization. The predisposition to this problem usually manifests on the ECG as a prolongation of the QT interval. QT prolongation may be congenital or acquired. Congenital problems include long QT syndrome and catecholaminergic polymorphic ventricular tachycardia. Acquired problems are usually related to drug toxicity or electrolyte abnormalities, but can occur as a result of myocardial ischemia. Class III anti-arrhythmic drugs such as sotalol and amiodarone
Amiodarone is an antiarrhythmic medication used to treat and prevent a number of types of cardiac dysrhythmias. This includes ventricular tachycardia, ventricular fibrillation, and wide complex tachycardia, atrial fibrillation, and paroxys ...
prolong the QT interval and may in some circumstances be pro-arrhythmic. Other relatively common drugs including some antibiotics and antihistamines may also be a danger, in particular in combination with one another. Problems with blood levels of potassium, magnesium and calcium may also contribute. High-dose magnesium is often used as an antidote in cardiac arrest protocols.
Diagnosis
Thediagnosis
Diagnosis (: diagnoses) is the identification of the nature and cause of a certain phenomenon. Diagnosis is used in a lot of different academic discipline, disciplines, with variations in the use of logic, analytics, and experience, to determine " ...
of ventricular tachycardia is made based on the rhythm seen on either a 12-lead ECG or a telemetry rhythm strip. It may be very difficult to differentiate between ventricular tachycardia and wide-complex supraventricular tachycardia in some cases. In particular, supraventricular tachycardias with aberrant conduction from a pre-existing bundle branch block are commonly misdiagnosed as ventricular tachycardia. Other rarer phenomena include Ashman beats and antidromic atrioventricular re-entry tachycardias.
Various diagnostic criteria have been developed to determine whether a wide complex tachycardia is ventricular tachycardia or a more benign rhythm. In addition to these diagnostic criteria, if the individual has a history of a myocardial infarction
A myocardial infarction (MI), commonly known as a heart attack, occurs when Ischemia, blood flow decreases or stops in one of the coronary arteries of the heart, causing infarction (tissue death) to the heart muscle. The most common symptom ...
, congestive heart failure
Heart failure (HF), also known as congestive heart failure (CHF), is a syndrome caused by an impairment in the heart's ability to fill with and pump blood.
Although symptoms vary based on which side of the heart is affected, HF typically pr ...
, or recent angina, the wide complex tachycardia is much more likely to be ventricular tachycardia.
The proper diagnosis is important, as the misdiagnosis of supraventricular tachycardia when ventricular tachycardia is present is associated with worse prognosis. This is particularly true if calcium channel blocker
Calcium channel blockers (CCB), calcium channel antagonists or calcium antagonists are a group of medications that disrupt the movement of calcium () through calcium channels. Calcium channel blockers are used as antihypertensive drugs, i.e., as ...
s, such as verapamil, are used to attempt to terminate a presumed supraventricular tachycardia. Therefore, it is wisest to assume that all wide complex tachycardia is VT until proven otherwise.
ECG features of ventricular tachycardia, in addition to the increased heart rate, are:
# A wide QRS complex (because the ectopics for the generation of the cardiac impulse originate in the ventricular myocyte and are propagated via the intermyocyte conduction, which is a delayed conduction)
# A Josephson's sign where there is the notch in the downsloping of the S wave near its nadir (considered very specific for the VT)
# Capture beats (normal QRS complex in between when the heart picks up the sinus rhythm from the impulses generated by the SA node), fusion beats (due to the fusion of the abnormal and the normal QRS complexes), which has a unique morphology
# Positive or negative concordance
# Extreme axis deviation or northwest axis (axis between -90 and +180 degrees)
Classification
 Ventricular tachycardia can be classified based on its ''morphology'':
* Monomorphic ventricular tachycardia means that the appearance of all the beats match each other in each lead of a surface electrocardiogram (ECG).
** Scar-related monomorphic ventricular tachycardia is the most common type and a frequent cause of death in patients having survived a heart attack, especially if they have weak heart muscle.
** Right ventricular outflow tract (RVOT) tachycardia is a type of monomorphic ventricular tachycardia originating in the right ventricular outflow tract. RVOT morphology refers to the characteristic pattern of this type of tachycardia on an ECG.
** The source of the re-entry circuit can be identified by evaluating the morphology of the QRS complex in the V1 lead of a surface ECG. If the R wave is dominant (consistent with a
Ventricular tachycardia can be classified based on its ''morphology'':
* Monomorphic ventricular tachycardia means that the appearance of all the beats match each other in each lead of a surface electrocardiogram (ECG).
** Scar-related monomorphic ventricular tachycardia is the most common type and a frequent cause of death in patients having survived a heart attack, especially if they have weak heart muscle.
** Right ventricular outflow tract (RVOT) tachycardia is a type of monomorphic ventricular tachycardia originating in the right ventricular outflow tract. RVOT morphology refers to the characteristic pattern of this type of tachycardia on an ECG.
** The source of the re-entry circuit can be identified by evaluating the morphology of the QRS complex in the V1 lead of a surface ECG. If the R wave is dominant (consistent with a right bundle branch block
A right bundle branch block (RBBB) is a heart block in the Bundle branches#Structure, right bundle branch of the Electrical conduction system of the heart, electrical conduction system.
During a right bundle branch block, the right ventricle (h ...
morphology), this indicates the origin of the VT is the left ventricle. Conversely, if the S wave is dominant (consistent with a left bundle branch block morphology, this is consistent with VT originating from the right ventricle or interventricular septum.
* Polymorphic ventricular tachycardia, on the other hand, has beat-to-beat variations in morphology. This may appear as a cyclical progressive change in cardiac axis, previously referred to by its French name '' torsades de pointes'' ("twisting of the spikes"). However, at the current time, the term ''torsades de pointes'' is reserved for polymorphic VT occurring in the context of a prolonged resting QT interval.
Another way to classify ventricular tachycardias is the ''duration of the episodes'': Three or more beats in a row on an ECG that originate from the ventricle at a rate of more than 120 beats per minute constitute a ventricular tachycardia.
* If the fast rhythm self-terminates within 30 seconds, it is considered a non-sustained ventricular tachycardia.
* If the rhythm lasts more than 30 seconds, it is known as a sustained ventricular tachycardia (even if it terminates on its own after 30 seconds).
A third way to classify ventricular tachycardia is on the basis of its ''symptoms'': Pulseless VT is associated with no effective cardiac output, hence, no effective pulse, and is a cause of cardiac arrest (see also: pulseless electrical activity EA. In this circumstance, it is best treated the same way as ventricular fibrillation (VF), and is recognized as one of the shockable rhythms on the cardiac arrest protocol. Some VT is associated with reasonable cardiac output and may even be asymptomatic. The heart usually tolerates this rhythm poorly in the medium to long term, and patients may certainly deteriorate to pulseless VT or to VF.
Occasionally in ventricular tachycardia, supraventricular impulses are conducted to the ventricles, generating QRS complexes with normal or aberrant supraventricular morphology (ventricular capture). Or, those impulses can be merged with complexes that are originated in the ventricle and produce a summation pattern (fusion complexes).
Less common is ventricular tachycardia that occurs in individuals with structurally normal hearts. This is known as ''idiopathic ventricular tachycardia'' and in the monomorphic form coincides with little or no increased risk of sudden cardiac death. In general, ''idiopathic ventricular tachycardia'' occurs in younger individuals diagnosed with VT. While the causes of idiopathic VT are not known, in general it is presumed to be congenital, and can be brought on by any number of diverse factors.
Treatment
Therapy may be directed either at terminating an episode of the abnormal heart rhythm or at reducing the risk of another VT episode. The treatment for stable VT is tailored to the specific person, with regard to how well the individual tolerates episodes of ventricular tachycardia, how frequently episodes occur, their comorbidities, and their wishes. Individuals with pulseless VT or unstable VT are hemodynamically compromised and require immediate electric cardioversion to shock them out of the VT rhythm.Cardioversion
If the patient has a pulse, meaning blood is circulating around their body and reaching vital organs, it is usually possible to terminate the episode using electric cardioversion. Cardioversion should be synchronized to the R wave in order to avoid degeneration of the rhythm toventricular fibrillation
Ventricular fibrillation (V-fib or VF) is an abnormal heart rhythm in which the Ventricle (heart), ventricles of the heart Fibrillation, quiver. It is due to disorganized electrical conduction system of the heart, electrical activity. Ventricula ...
, if possible. An initial energy of 100J is recommended. If the waveform is polymorphic, then higher energies and an unsynchronized shock should be provided (also known as defibrillation).
Defibrillation
A person with pulseless VT should be treated following current ACLS guidelines. This includes high-energy unsynchronized defibrillation, at either 360J for a monophasic defibrillator or 200J for a biphasic defibrillator. Additionally, epinephrine and other antiarrythmatics such as lidocane may be administered to terminate the rhythm. The shock may be delivered to the outside of the chest using the two pads of an external defibrillator, or internally to the heart by an implantable cardioverter-defibrillator (ICD) if one has previously been inserted. An ICD may also be set to attempt to overdrive pace the ventricle. Pacing the ventricle at a rate faster than the underlying tachycardia can sometimes be effective in terminating the rhythm. If this fails after a short trial, the ICD will usually stop pacing, charge up and deliver a defibrillation grade shock.Medication
For those who are stable with a monomorphic waveform the medications procainamide or sotalol may be used and are more effective thanlidocaine
Lidocaine, also known as lignocaine and sold under the brand name Xylocaine among others, is a local anesthetic of the amino amide type. It is also used to treat ventricular tachycardia and ventricular fibrillation. When used for local anae ...
. Evidence does not show that amiodarone
Amiodarone is an antiarrhythmic medication used to treat and prevent a number of types of cardiac dysrhythmias. This includes ventricular tachycardia, ventricular fibrillation, and wide complex tachycardia, atrial fibrillation, and paroxys ...
is better than procainamide.
Torsades de Pointes (polymorphic VT) can be caused by low magnesium level in the blood. Thus, magnesium sulfate can be administered to help terminate the arrhythmia.
Long-term anti-arrhythmic therapy may be indicated to prevent recurrence of VT. Beta-blockers and a number of class III anti-arrhythmics are commonly used, such as the beta-blockers carvedilol, metoprolol, and bisoprolol, and the Potassium-Channel-Blockers amiodarone, dronedarone, bretylium, sotalol, ibutilide, and dofetilide. Angiotensin-converting-enzyme (ACE) inhibitors and aldosterone antagonists are also sometimes used in this setting.
Invasive treatment
AnICD
The International Classification of Diseases (ICD) is a globally used medical classification that is used in epidemiology, health management and clinical diagnostics, diagnosis. The ICD is maintained by the World Health Organization (WHO), which ...
(implantable cardioverter defibrillator) is more effective than drug therapy for prevention of sudden cardiac death due to VT and VF, but does not prevent these rhythms from happening.
Catheter ablation is a potentially definitive treatment option for those with recurrent VT. Remote magnetic navigation is one effective method to do the procedure.
In the past, ablation was often not considered until pharmacological options had been exhausted, often after the patient had developed substantial morbidity from recurrent episodes of VT and ICD shocks. Antiarrhythmic medications can reduce the frequency of ICD therapies, but have efficacy varies and side effects can be significant. Advances in technology and understanding of VT substrates now allow ablation of multiple and unstable VTs with acceptable safety and efficacy, even in patients with advanced heart disease.
References
External links
Ventricular Tachycardia (Free ECG book)
{{Authority control Cardiac arrhythmia Wikipedia medicine articles ready to translate Wikipedia emergency medicine articles ready to translate