 Polyclonal B cell response is a natural mode of immune response exhibited by the
Polyclonal B cell response is a natural mode of immune response exhibited by the Humoral response to infection
Diseases which can be transmitted from one organism to another are known asB cell response
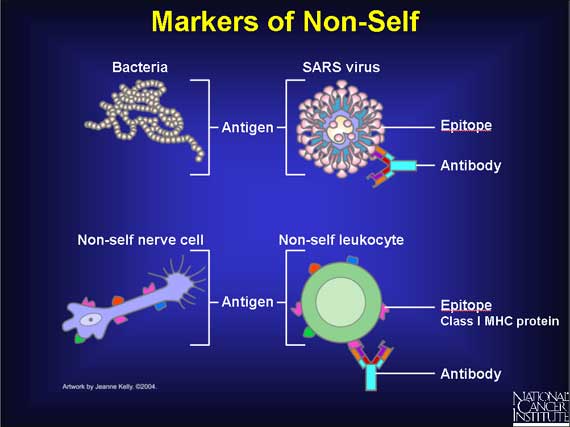
Recognition of pathogens
Pathogens synthesizeSpecific recognition of epitope by B cells
Nonspecific recognition by macrophages
Macrophages and related cells employ a different mechanism to recognize the pathogen. Their receptors recognize certain motifs present on the invading pathogen that are very ''unlikely'' to be present on a host cell. Such repeating motifs are recognized by pattern recognition receptors (PRRs) like the toll-like receptors (TLRs) expressed by the macrophages. Since the same receptor could bind to a given motif present on surfaces of widely disparate microorganisms, this mode of recognition is relatively nonspecific, and constitutes anAntigen processing
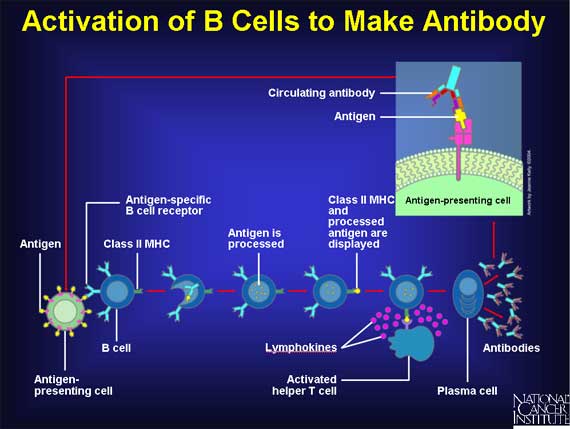
Antigen presentation
After the processed antigen (peptide) is complexed to the MHC molecule, they both migrate together to theT helper cell stimulation
The CD 4+ cells through their T cell receptor- CD3 complex recognize the epitope-bound MHC II molecules on the surface of the antigen presenting cells, and get 'activated'. Upon this activation, these T cells proliferate and differentiate into Th2 cells. This makes them produce soluble chemical signals that promote their own survival. However, another important function that they carry out is the stimulation of B cell by establishing ''direct'' physical contact with them.Co-stimulation of B cell by activated T helper cell
Complete stimulation of T helper cells requires the B7 molecule present on the antigen presenting cell to bind with CD28 molecule present on the T cell surface (in close proximity with the T cell receptor). Likewise, a second interaction between the CD40 ligand or CD154 ( CD40L) present on T cell surface and CD40 present on B cell surface, is also necessary. The same interactions that stimulate the T helper cell also stimulate the B cell, hence the term ''costimulation''. The entire mechanism ensures that an activated T cell only stimulates a B cell that recognizes the antigen containing the ''same'' epitope as recognized by the T cell receptor of the "costimulating" T helper cell. The B cell gets stimulated, apart from the direct costimulation, by certain growth factors, viz., interleukins 2, 4, 5, and 6 in a paracrine fashion. These factors are usually produced by the newly activated T helper cell. However, this activation occurs only after the B cell receptor present on a memory or aProliferation and differentiation of B cell
A naive (or ''inexperienced'') B cell is one which belongs to a clone which has never encountered the epitope to which it is specific. In contrast, a memory B cell is one which derives from an activated naive or memory B cell. The activation of a naive or a memory B cell is followed by a manifold proliferation of that particular B cell, most of the progeny of which terminally differentiate into plasma B cells;The plasma cells secrete antibodies that bind to the ''same'' structure that had stimulated the B cell in the first place by binding to its B cell receptor. the rest survive as memory B cells. So, when the naive cells belonging to a particular clone encounter their specific antigen to give rise to the plasma cells, and also leave a few memory cells, this is known as the ''primary immune response''. In the course of proliferation of this clone, the B cell receptorDefinition of ''Affinity'' from Online Etymology Dictionary
an
Definition of ''Affinity'' from TheFreeDictionary by Farlex
/ref> Other paratopes bind better to epitopes that are ''slightly'' different from the original epitope that had stimulated proliferation. Variations in the epitope structure are also usually produced by mutations in the genes of pathogen coding for their antigen. Somatic hypermutation, thus, makes the B cell receptors and the soluble antibodies in subsequent encounters with antigens, more inclusive in their antigen recognition potential of ''altered'' epitopes, apart from bestowing greater specificity for the antigen that induced proliferation in the first place. When the memory cells get stimulated by the antigen to produce plasma cells (just like in the clone's primary response), and leave even more memory cells in the process, this is known as a ''
Basis of polyclonality
Responses are polyclonal in nature as each clone somewhat specializes in producing antibodies against a given epitope, and because, each antigen contains multiple epitopes, each of which in turn can be recognized by more than one clone of B cells. To be able to react to innumerable antigens, as well as multiple constituent epitopes, the immune system requires the ability to recognize a very great number of epitopes in all, i.e., there should be a great diversity of B cell clones.Clonality of B cells
Memory and naïve B cells normally exist in relatively small numbers. As the body needs to be able to respond to a large number of potential pathogens, it maintains a pool of B cells with a wide range of specificities. Consequently, while there is almost always at least one B (naive or memory) cell capable of responding to any given epitope (of all that the immune system can react against), there are very few exact duplicates. However, when a single B cell encounters an antigen to which it can bind, it can proliferate very rapidly. Such a group of cells with identical specificity towards the epitope is known as a ''Single antigen contains multiple overlapping epitopes
 A single antigen can be thought of as a sequence of multiple overlapping epitopes. Many unique B cell clones may be able to bind to the individual epitopes. This imparts even greater multiplicity to the overall response. All of these B cells can become activated and produce large colonies of plasma cell clones, each of which can secrete up to 1000 antibody molecules against each epitope per second.
A single antigen can be thought of as a sequence of multiple overlapping epitopes. Many unique B cell clones may be able to bind to the individual epitopes. This imparts even greater multiplicity to the overall response. All of these B cells can become activated and produce large colonies of plasma cell clones, each of which can secrete up to 1000 antibody molecules against each epitope per second.
Multiple clones recognize single epitope
In addition to different B cells reacting to ''different'' epitopes on the same antigen, B cells belonging to different clones may also be able to react to the ''same'' epitope. An epitope that can be attacked by many different B cells is said to be highly ''immunogenic''. In these cases, the ''binding affinities'' for respective epitope-paratope pairs vary, with some B cell clones producing antibodies that bind strongly to the epitope, and others producing antibodies that bind weakly.Clonal selection
The clones that bind to a particular epitope with greater strength are more likely to be ''selected'' for further proliferation in the germinal centers of the follicles in various lymphoid tissues like the lymph nodes. This is not unlikeDiversity of B cell clones
Although there are many diverse pathogens, many of which are constantly mutating, it is a surprise that a majority of individuals remain free of infections. Thus, maintenance of health requires the body to recognize all pathogens (antigens they present or produce) likely to exist. This is achieved by maintaining a pool of immensely large (about 109) clones of B cells, each of which reacts against a specific epitope by recognizing and producing antibodies against it. However, at any given time very few clones actually remain receptive to their specific epitope. Thus, approximately 107 different epitopes can be recognized by all the B cell clones combined. Moreover, in a lifetime, an individual usually requires the generation of antibodies against very few antigens in comparison with the number that the body can recognize and respond against.Significance of the phenomenon
Increased probability of recognizing any antigen
If an antigen can be recognized by more than one component of its structure, it is less likely to be "missed" by the immune system.Analogically, if in a crowded place, one is supposed to recognize a person, it is better to know as many physical features as possible. If you know the person only by the hairstyle, there is a chance of overlooking the person if that changes. Whereas, if apart from the hairstyle, if you also happen to know the facial features and what the person will wear on a particular day, it becomes much more unlikely that you will miss that person. Mutation of pathogenic organisms can result in modification of antigen—and, hence, epitope—structure. If the immune system "remembers" what the other epitopes look like, the antigen, and the organism, will still be recognized and subjected to the body's immune response. Thus, the polyclonal response widens the range of pathogens that can be recognized.Limitation of immune system against rapidly mutating viruses
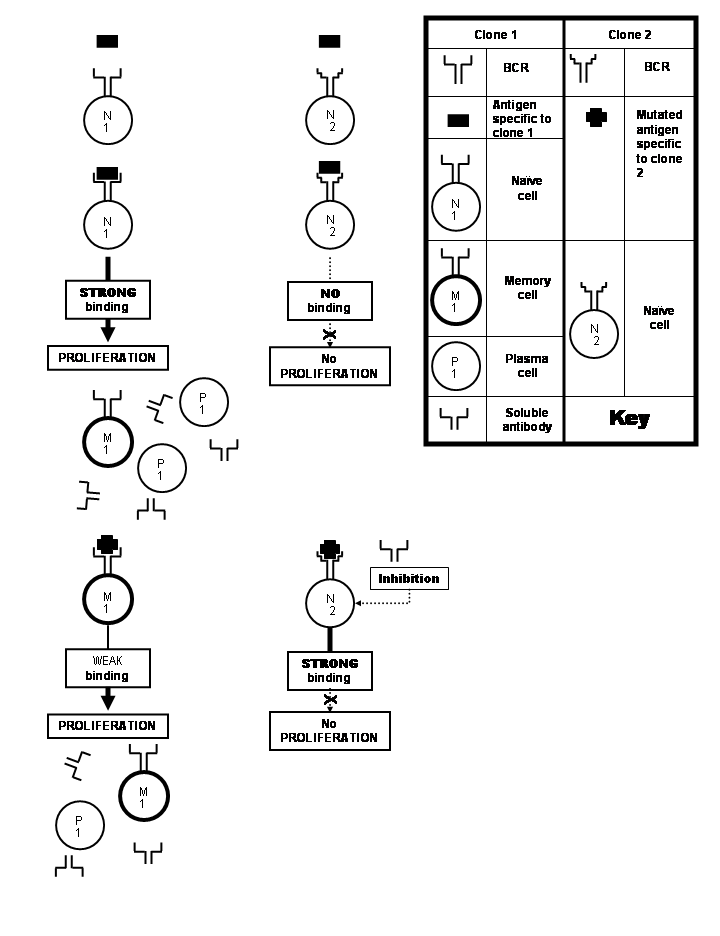 Many viruses undergo frequent mutations that result in changes in amino acid composition of their important proteins. Epitopes located on the protein may also undergo alterations in the process. Such an altered epitope binds less strongly with the antibodies specific to the unaltered epitope that would have stimulated the immune system. This is unfortunate because somatic hypermutation does give rise to clones capable of producing soluble antibodies that would have bound the altered epitope avidly enough to neutralize it. But these clones would consist of naive cells which are not allowed to proliferate by the weakly binding antibodies produced by the priorly stimulated clone. This doctrine is known as the '' original antigenic sin''. This phenomenon comes into play particularly in immune responses against
Many viruses undergo frequent mutations that result in changes in amino acid composition of their important proteins. Epitopes located on the protein may also undergo alterations in the process. Such an altered epitope binds less strongly with the antibodies specific to the unaltered epitope that would have stimulated the immune system. This is unfortunate because somatic hypermutation does give rise to clones capable of producing soluble antibodies that would have bound the altered epitope avidly enough to neutralize it. But these clones would consist of naive cells which are not allowed to proliferate by the weakly binding antibodies produced by the priorly stimulated clone. This doctrine is known as the '' original antigenic sin''. This phenomenon comes into play particularly in immune responses against Increased chances of autoimmune reactions
In autoimmunity the immune system wrongly recognizes certain native molecules in the body as foreign (''self-antigen''), and mounts an immune response against them. Since these native molecules, as normal parts of the body, will naturally always exist in the body, the attacks against them can get stronger over time (akin to secondary immune response). Moreover, many organisms exhibitDifficulty in producing monoclonal antibodies
History
The first evidence of presence of a neutralizing substance in the blood that could counter infections came when Emil von Behring along with Kitasato Shibasaburō in 1890 developed effectiveSee also
*Notes
References
Further reading
* * *External links
An Introduction to the Immune system
{{DEFAULTSORT:Polyclonal B Cell Response Immune system Immunology Cell biology