|
Histocompatibility
Histocompatibility, or tissue compatibility, is the property of having the same, or sufficiently similar, alleles of a set of genes called human leukocyte antigens (HLA), or major histocompatibility complex (MHC). Each individual expresses many unique HLA proteins on the surface of their cells, which signal to the immune system whether a cell is part of the self or an invading organism. T cells recognize foreign HLA molecules and trigger an immune response to destroy the foreign cells. Histocompatibility testing is most relevant for topics related to whole organ, tissue, or stem cell transplants, where the similarity or difference between the donor's HLA alleles and the recipient's triggers the immune system to reject the transplant. The wide variety of potential HLA alleles lead to unique combinations in individuals and make matching difficult. Discovery The discovery of the MHC and role of histocompatibility in transplantation was a combined effort of many scientists in the 20t ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |
Major Histocompatibility Complex
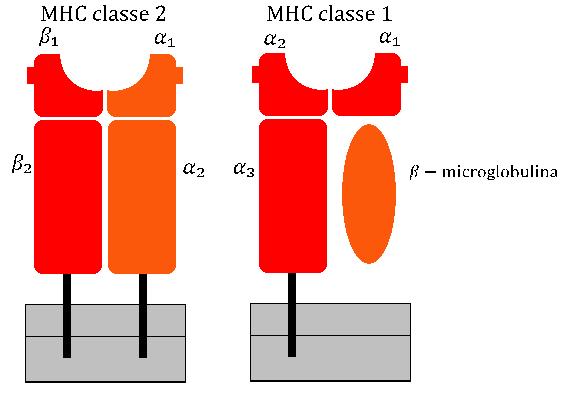
The major histocompatibility complex (MHC) is a large Locus (genetics), locus on vertebrate DNA containing a set of closely linked polymorphic genes that code for Cell (biology), cell surface proteins essential for the adaptive immune system. These cell surface proteins are called MHC molecules. Its name comes from its discovery during the study of transplanted tissue compatibility. Later studies revealed that tissue rejection due to incompatibility is only a facet of the full function of MHC molecules, which is to bind an antigen derived from self-proteins, or from pathogens, and bring the antigen presentation to the cell surface for recognition by the appropriate T cell, T-cells. MHC molecules mediate the interactions of leukocytes, also called white blood cells (WBCs), with other leukocytes or with body cells. The MHC determines donor compatibility for organ transplant, as well as one's susceptibility to autoimmune diseases. In a cell, protein molecules of the host's own pheno ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |
Jean Dausset
Jean-Baptiste-Gabriel-Joachim Dausset (19 October 1916 – 6 June 2009) was a French immunologist born in Toulouse, France. Dausset received the Nobel Prize in Physiology or Medicine in 1980 along with Baruj Benacerraf and George Davis Snell for their discovery and characterisation of the genes making the major histocompatibility complex. Using the money from his Nobel Prize and a grant from the French Television, Dausset founded the Human Polymorphism Study Center ( CEPH) in 1984, which was later renamed the Foundation Jean Dausset-CEPH in his honour. He married Rose Mayoral in 1963, with whom he had two children, Henri and Irène. Jean Dausset died on June 6, 2009, in Majorca, Spain, at the age of 92. Early life Jean-Baptiste-Gabriel-Joachim Dausset was born on 19 October 1916, in Toulouse, France. He was the youngest of four children of Henri Dausset and Elisabeth Dausset (born Renard). His father was from the Pyrénées, and was a doctor by profession, and his mother was a ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |
HLA-A
HLA-A is a group of human leukocyte antigens (HLA) that are encoded by the ''HLA-A'' locus (genetics), locus, which is located at human chromosome 6p21.3. HLA is a major histocompatibility complex (MHC) antigen specific to humans. HLA-A is one of three major types of human MHC class I transmembrane proteins. The others are HLA-B and HLA-C. The protein is a heterodimer, and is composed of a heavy α chain and smaller β chain. The α chain is encoded by a variant #HLA-A gene, ''HLA-A'' gene, and the β chain (β2-microglobulin) is an invariant Beta-2 microglobulin, β2 microglobulin molecule. The β2 microglobulin protein is encoded by the ''B2M'' gene, which is located at chromosome 15q21.1 in humans. MHC Class I molecules such as HLA-A participate in a process that presents short polypeptides to the immune system. These polypeptides are typically 7–11 amino acids in length and originate from proteins being expressed by the cell. There are two classes of polypeptide that can be ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |
Antigen
In immunology, an antigen (Ag) is a molecule, moiety, foreign particulate matter, or an allergen, such as pollen, that can bind to a specific antibody or T-cell receptor. The presence of antigens in the body may trigger an immune response. Antigens can be proteins, peptides (amino acid chains), polysaccharides (chains of simple sugars), lipids, or nucleic acids. Antigens exist on normal cells, cancer cells, parasites, viruses, fungus, fungi, and bacteria. Antigens are recognized by antigen receptors, including antibodies and T-cell receptors. Diverse antigen receptors are made by cells of the immune system so that each cell has a specificity for a single antigen. Upon exposure to an antigen, only the lymphocytes that recognize that antigen are activated and expanded, a process known as clonal selection. In most cases, antibodies are ''antigen-specific'', meaning that an antibody can only react to and bind one specific antigen; in some instances, however, antibodies may cr ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |
Baruj Benacerraf
Baruj Benacerraf (; October 29, 1920 – August 2, 2011) was a Venezuelan-American immunologist, who shared the 1980 Nobel Prize in Physiology or Medicine for the "discovery of the major histocompatibility complex genes which encode cell surface protein molecules important for the immune system's distinction between self and non-self."Baruj Benacerraf – Biographical nobelprize.org His colleagues and shared recipients were Jean Dausset and . Early life and education Benacerraf was born in |
Peter Alfred Gorer
Peter Alfred Gorer FRS (14 April 1907 in London – 1961) was a British immunologist, pathologist and geneticist who pioneered the field of transplant immunology. Peter Gorer was born in London to Edgar (drowned in the 1915 sinking of RMS Lusitania) and Rachel née Cohen Gorer. He died of lung cancer in 1961. Education and work institutions He was educated at Charterhouse. He graduated from Guy's Hospital, London in 1929 and then studied genetics under J.B.S. Haldane at University College, London. From 1933 to 1940 Gorer worked at the Lister Institute before returning to Guy's Hospital to work as a pathologist. Research Gorer is credited with the co-discovery of histocompatibility antigens and the elucidation of their genetic regulation. Together with George Snell, he helped discover the murine histocompatibility 2 locus, or H-2, which is analogous to the human leukocyte antigen. Gorer also identified antigen II and determined its role in transplant tissue reje ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |
T Cell
T cells (also known as T lymphocytes) are an important part of the immune system and play a central role in the adaptive immune response. T cells can be distinguished from other lymphocytes by the presence of a T-cell receptor (TCR) on their cell surface receptor, cell surface. T cells are born from hematopoietic stem cells, found in the bone marrow. Developing T cells then migrate to the thymus gland to develop (or mature). T cells derive their name from the thymus. After migration to the thymus, the precursor cells mature into several distinct types of T cells. T cell differentiation also continues after they have left the thymus. Groups of specific, differentiated T cell subtypes have a variety of important functions in controlling and shaping the immune response. One of these functions is immune-mediated cell death, and it is carried out by two major subtypes: Cytotoxic T cell, CD8+ "killer" (cytotoxic) and T helper cell, CD4+ "helper" T cells. (These are named for the presen ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |
MHC Class I
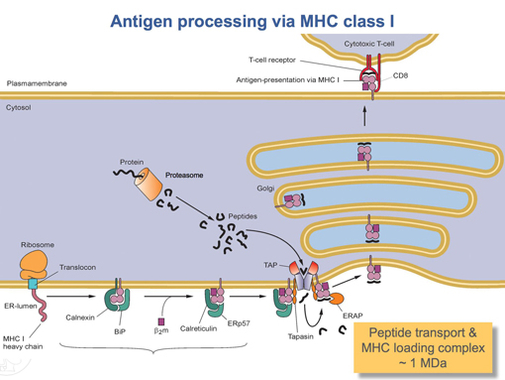
MHC class I molecules are one of two primary classes of major histocompatibility complex (MHC) molecules (the other being MHC class II) and are found on the cell surface of all nucleated cells in the bodies of vertebrates. They also occur on platelets, but not on red blood cells. Their function is to display peptide fragments of proteins from within the cell to cytotoxic T cells; this will trigger an immediate response from the immune system against a particular non-self antigen displayed with the help of an MHC class I protein. Because MHC class I molecules present peptides derived from cytosolic proteins, the pathway of MHC class I presentation is often called ''cytosolic'' or ''endogenous pathway''. In humans, the HLAs corresponding to MHC class I are HLA-A, HLA-B, and HLA-C. Function Class I MHC molecules bind peptides generated mainly from the degradation of cytosolic proteins by the proteasome. The MHC I: peptide complex is then inserted via the endoplasmic re ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |
HLA-DR
HLA-DR is an MHC class II cell surface receptor encoded by the human leukocyte antigen complex on chromosome 6 region 6p21.31. The complex of HLA-DR (Human Leukocyte Antigen – DR isotype) and peptide, generally between 9 and 30 amino acids in length, constitutes a ligand for the T-cell receptor (TCR). HLA (human leukocyte antigens) were originally defined as cell surface antigens that mediate graft-versus-host disease. Identification of these antigens has led to greater success and longevity in organ transplant. Antigens most responsible for graft loss are HLA-DR (first six months), HLA-B (first two years), and HLA-A (long-term survival). Good matching of these antigens between host and donor is most critical for achieving graft survival. HLA-DR is also involved in several autoimmune conditions, disease susceptibility and disease resistance. It is also closely linked to HLA-DQ and this linkage often makes it difficult to resolve the more causative factor in disease. HLA-DR mo ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |
HLA-B
HLA-B (major histocompatibility complex, class I, B) is a human gene that provides instructions for making a protein that plays a critical role in the immune system. HLA-B is part of a family of genes called the human leukocyte antigen (HLA) complex. The HLA complex helps the immune system distinguish the body's own proteins from proteins made by foreign invaders such as viruses and bacteria. HLA is the human version of the major histocompatibility complex (MHC), a gene family that occurs in many species. Genes in this complex are separated into three basic groups: class I, class II, and class III. In humans, the HLA-B gene and two related genes, HLA-A and HLA-C, are the major genes in MHC class I. MHC class I genes provide instructions for making proteins that are present on the surface of almost all cells. On the cell surface, these proteins are bound to protein fragments (peptides) that have been exported from within the cell. MHC class I proteins display these peptides to ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |
Transplant Rejection
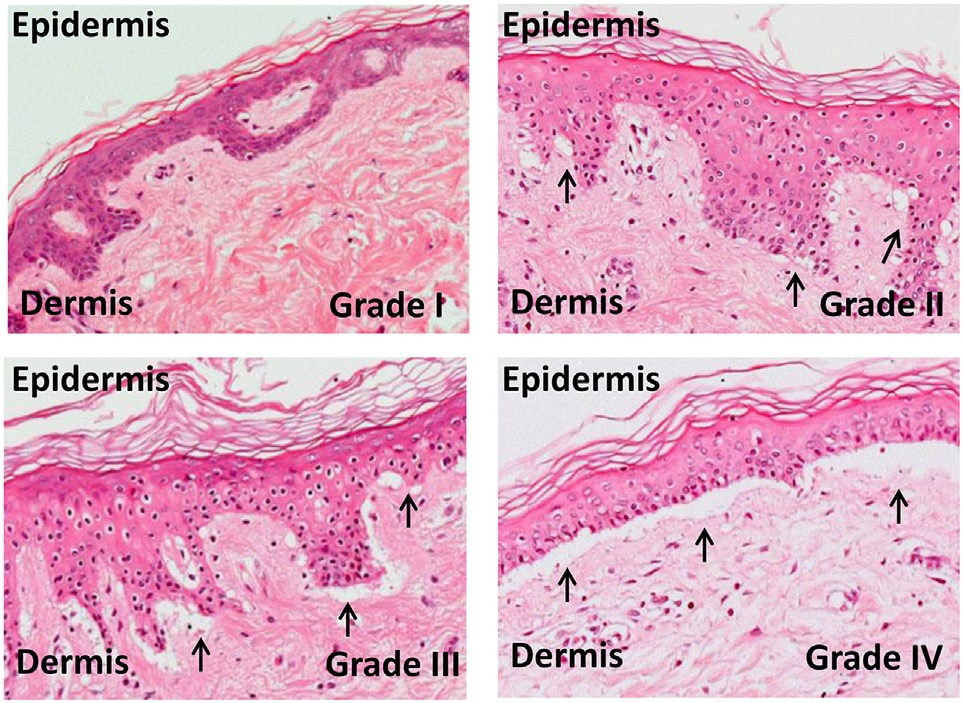
Transplant rejection occurs when transplanted tissue is rejected by the recipient's immune system, which destroys the transplanted tissue. Transplant rejection can be lessened by determining the molecular similitude between donor and recipient and by use of immunosuppressant drugs after transplant. Types Transplant rejection can be classified into three types: hyperacute, acute, and chronic. These types are differentiated by how quickly the recipient's immune system is activated and the specific aspect or aspects of immunity involved. Hyperacute rejection Hyperacute rejection is a form of rejection that manifests itself in the minutes to hours following transplantation. It is caused by the presence of pre-existing antibodies in the recipient that recognize antigens in the donor organ. These antigens are located on the endothelial lining of blood vessels within the transplanted organ and, once antibodies bind, will lead to the rapid activation of the complement system. ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |
Graft-versus-host Disease
Graft-versus-host disease (GvHD) is a syndrome, characterized by inflammation in different organs. GvHD is commonly associated with bone marrow transplants and stem cell transplants. White blood cells of the donor's immune system which remain within the donated tissue (the graft) recognize the recipient (the host) as foreign (non-self). The white blood cells present within the transplanted tissue then attack the recipient's body's cells, which leads to GvHD. This should not be confused with a transplant rejection, which occurs when the immune system of the transplant recipient rejects the transplanted tissue; GvHD occurs when the donor's immune system's white blood cells reject the recipient. The underlying principle ( alloimmunity) is the same, but the details and course may differ. GvHD can also occur after a blood transfusion, known as ''Transfusion-associated graft-versus-host disease'' or TA-GvHD if the blood products used have not been gamma irradiated or treated ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |