Intradural Anesthesia on:
[Wikipedia]
[Google]
[Amazon]
Spinal anaesthesia (or spinal anesthesia), also called spinal block, subarachnoid block, intradural block and intrathecal block, is a form of neuraxial regional anaesthesia involving the injection of a local anaesthetic or opioid into the
 Epidural anaesthesia is a technique whereby a local anaesthetic drug is injected through a catheter placed into the epidural space. This technique is similar to spinal anaesthesia as both are neuraxial, and the two techniques may be easily confused with each other. Differences include:
* A spinal anaesthetic delivers drug to the subarachnoid space and into the cerebrospinal fluid, allowing it to act on the spinal cord directly. An epidural delivers drugs outside the dura (outside CSF), and has its main effect on nerve roots leaving the dura at the level of the epidural, rather than on the spinal cord itself.
* A spinal gives profound block of all motor and sensory function below the level of injection, whereas an epidural blocks a 'band' of nerve roots around the site of injection, with normal function above, and close-to-normal function below the levels blocked.
* The injected dose for an epidural is larger, being about 10–20 mL compared to 1.5–3.5 mL in a spinal.
* In an epidural, an indwelling catheter may be placed that allows for redosing injections, while a spinal is almost always a one-shot only. Therefore, spinal anaesthesia is more often used for shorter procedures relative to procedures which require epidural anaesthesia.
* The onset of analgesia is approximately 25–30 minutes in an epidural, while it is approximately 5 minutes in a spinal.
* An epidural often does not cause as significant a
Epidural anaesthesia is a technique whereby a local anaesthetic drug is injected through a catheter placed into the epidural space. This technique is similar to spinal anaesthesia as both are neuraxial, and the two techniques may be easily confused with each other. Differences include:
* A spinal anaesthetic delivers drug to the subarachnoid space and into the cerebrospinal fluid, allowing it to act on the spinal cord directly. An epidural delivers drugs outside the dura (outside CSF), and has its main effect on nerve roots leaving the dura at the level of the epidural, rather than on the spinal cord itself.
* A spinal gives profound block of all motor and sensory function below the level of injection, whereas an epidural blocks a 'band' of nerve roots around the site of injection, with normal function above, and close-to-normal function below the levels blocked.
* The injected dose for an epidural is larger, being about 10–20 mL compared to 1.5–3.5 mL in a spinal.
* In an epidural, an indwelling catheter may be placed that allows for redosing injections, while a spinal is almost always a one-shot only. Therefore, spinal anaesthesia is more often used for shorter procedures relative to procedures which require epidural anaesthesia.
* The onset of analgesia is approximately 25–30 minutes in an epidural, while it is approximately 5 minutes in a spinal.
* An epidural often does not cause as significant a
Effect of Glucose Concentration on the Intrathecal Spread of 0.5% Bupivacaine
/ref>
Transparent reality simulation of spinal anaesthesia
Various diagrams of needles for Lumbar puncture, Epidural, Spinal Anesthesia, etc
{{DEFAULTSORT:Spinal Anaesthesia Regional anesthesia
subarachnoid space
In anatomy, the meninges (, ''singular:'' meninx ( or ), ) are the three membranes that envelop the brain and spinal cord. In mammals, the meninges are the dura mater, the arachnoid mater, and the pia mater. Cerebrospinal fluid is located in th ...
, generally through a fine needle
Needle may refer to:
Crafting
* Crochet needle, a tool for making loops in thread or yarn
* Knitting needle, a tool for knitting, not as sharp as a sewing needle
* Sewing needle, a long slender tool with a pointed tip
* Trussing needle, a long sl ...
, usually long. It is a safe and effective form of anesthesia usually performed by anesthesiologists that can be used as an alternative to general anesthesia commonly in surgeries involving the lower extremities and surgeries below the umbilicus. The local anesthetic with or without an opioid injected into the cerebrospinal fluid provides locoregional anaesthesia: true analgesia, motor, sensory and autonomic (sympathic) blockade.
Administering analgesics (opioid, alpha2-adrenoreceptor agonist) in the cerebrospinal fluid without a local anaesthetic produces locoregional analgesia: markedly reduced pain sensation (incomplete analgesia), some autonomic blockade (parasympathetic plexi), but no sensory or motor block.
Locoregional analgesia, due to mainly the absence of motor and sympathic block may be preferred over locoregional anaesthesia in some postoperative care settings.
The tip of the spinal needle has a point or small bevel
A bevelled edge (UK) or beveled edge (US) is an edge of a structure that is not perpendicular to the faces of the piece. The words bevel and chamfer overlap in usage; in general usage they are often interchanged, while in technical usage they ...
. Recently, pencil point needles have been made available (Whitacre, Sprotte, Gertie Marx
Gertie Florentine Marx (1912-2004) was an obstetric anesthesiologist, "internationally known as 'the mother of obstetric anaesthesia'".Gerard M. BassellIn Memoriam: Gertie F. Marx, MD (1912–2004) ''International Journal of Obstetric Anesthesia'' ...
and others).
Indications
Spinal anaesthesia is a commonly used technique, either on its own or in combination withsedation
Sedation is the reduction of irritability or agitation by administration of sedative drugs, generally to facilitate a medical procedure or diagnostic procedure. Examples of drugs which can be used for sedation include isoflurane, diethyl ether, ...
or general anaesthesia
General anaesthesia (UK) or general anesthesia (US) is a medically induced loss of consciousness that renders the patient unarousable even with painful stimuli. This effect is achieved by administering either intravenous or inhalational general ...
. It is most commonly used for surgeries below the umbilicus, however recently its uses have extended to some surgeries above the umbilicus as well as for postoperative analgesia. Procedures which use spinal anesthesia include:
* Orthopaedic surgery on the pelvis
The pelvis (plural pelves or pelvises) is the lower part of the trunk, between the abdomen and the thighs (sometimes also called pelvic region), together with its embedded skeleton (sometimes also called bony pelvis, or pelvic skeleton).
The ...
, hip
In vertebrate anatomy, hip (or "coxa"Latin ''coxa'' was used by Celsus in the sense "hip", but by Pliny the Elder in the sense "hip bone" (Diab, p 77) in medical terminology) refers to either an anatomical region or a joint.
The hip region is ...
, femur, knee
In humans and other primates, the knee joins the thigh with the leg and consists of two joints: one between the femur and tibia (tibiofemoral joint), and one between the femur and patella (patellofemoral joint). It is the largest joint in the hu ...
, tibia, and ankle, including arthroplasty and joint replacement
* Vascular surgery
Vascular surgery is a surgical subspecialty in which diseases of the vascular system, or arteries, veins and lymphatic circulation, are managed by medical therapy, minimally-invasive catheter procedures and surgical reconstruction. The specialty ...
on the legs
* Endovascular aortic aneurysm repair
* Hernia (inguinal
In human anatomy, the inguinal region refers to either the groin or the lower lateral regions of the abdomen. It may also refer to:
* Conjoint tendon, previously known as the inguinal aponeurotic falx, a structure formed from the transversus abdo ...
or epigastric)
* Haemorrhoidectomy
* Nephrectomy and cystectomy in combination with general anaesthesia
* Transurethral resection of the prostate
Transurethral resection of the prostate (commonly known as a TURP, plural TURPs, and rarely as a transurethral prostatic resection, TUPR) is a urological operation. It is used to treat benign prostatic hyperplasia (BPH). As the name indicates, ...
and transurethral resection of bladder tumours
* Hysterectomy
Hysterectomy is the surgical removal of the uterus. It may also involve removal of the cervix, ovaries (oophorectomy), Fallopian tubes (salpingectomy), and other surrounding structures.
Usually performed by a gynecologist, a hysterectomy may b ...
in different techniques used
* Caesarean sections
* Pain management during vaginal birth and delivery
* Urology cases
* Examinations under anaesthesia
Spinal anaesthesia is the technique of choice for Caesarean section as it avoids a general anaesthetic and the risk of failed intubation (which is probably a lot lower than the widely quoted 1 in 250 in pregnant women). It also means the mother is conscious and the partner is able to be present at the birth of the child. The post operative analgesia from intrathecal opioids in addition to non-steroidal anti-inflammatory drugs is also good.
Spinal anesthesia may be favored when the surgical site is amenable to spinal blockade for patients with severe respiratory disease such as COPD as it avoids the potential respiratory consequences of intubation and ventilation. It may also be useful in patients where anatomical abnormalities may make tracheal intubation relatively difficult.
In pediatric patients, spinal anesthesia is particularly useful in children with difficult airways and those who are poor candidates for endotracheal anesthesia such as increased respiratory risks or presence of full stomach.
This can also be used to effectively treat and prevent pain following surgery, particularly thoracic, abdominal pelvic, and lower extremity orthopedic procedures.
Contraindications
Prior to receiving spinal anesthesia, it is important to provide a thorough medical evaluation to ensure there are no absolute contraindications and to minimize risks and complications. Although contraindications are rare, below are some of them: * Patient refusal * Local infection or sepsis at the site of injection *Bleeding disorders
Coagulopathy (also called a bleeding disorder) is a condition in which the blood's ability to coagulate (form clots) is impaired. This condition can cause a tendency toward prolonged or excessive bleeding (bleeding diathesis), which may occur spo ...
, thrombocytopaenia, or systemic anticoagulation (secondary to an increased risk of a spinal epidural hematoma)
* Severe aortic stenosis
* Increased intracranial pressure
* Space occupying lesions of the brain
* Anatomical disorders of the spine such as scoliosis (although where pulmonary function is also impaired, spinal anaesthesia may be favored)
* Hypovolaemia e.g. following massive haemorrhage, including in obstetric patients
* Allergy
Relative Contraindication
* Ehlers Danlos Syndrome, or other disorders causing resistance to local anesthesia
Risks and complications
Complications of spinal anesthesia can result from the physiologic effects on the nervous system and can also be related to placement technique. Most of the common side effects are minor and are self-resolving or easily treatable while major complications can result in more serious and permanent neurological damage and rarely death. These symptoms can occur immediately after administration of the anesthetic or be delayed. Common and minor complications include: * Mild hypotension *Bradycardia
Bradycardia (also sinus bradycardia) is a slow resting heart rate, commonly under 60 beats per minute (BPM) as determined by an electrocardiogram. It is considered to be a normal heart rate during sleep, in young and healthy or elderly adults, a ...
* Nausea and vomiting
* Transient neurological symptoms (lower back pain with pain in the legs)
* Post-dural-puncture headache
Post-dural-puncture headache (PDPH) is a complication of puncture of the dura mater (one of the membranes around the brain and spinal cord). The headache is severe and described as "searing and spreading like hot metal", involving the back and fro ...
or post-spinal headache - Associated with the size and type of spinal needle used. A 2020 meta analysis recommended use of the 26G atraumatic spinal needle to lower the risk of PDPH - specifically, the Braun Atraucan 26G needle.
Serious and permanent complications are rare but are usually related to physiologic effects on the cardiovascular system and neurological system or when the injection has been unintentionally at the wrong site. The following are some major complications:
* Nerve injuries: Cauda equina syndrome, radiculopathy
* Cardiac arrest
* Severe hypotension
* Spinal epidural hematoma, with or without subsequent neurological sequelae due to compression of the spinal nerves.
* Epidural abscess
* Infection (e.g. meningitis)
Technique
Regardless of the anaesthetic agent (drug) used, the desired effect is to block the transmission of afferent nerve signals from peripheral nociceptors. Sensory signals from the site are blocked, thereby eliminating pain. The degree of neuronal blockade depends on the amount and concentration of local anaesthetic used and the properties of the axon. Thin unmyelinatedC-fibres
Group C nerve fibers are one of three classes of nerve fiber in the central nervous system (CNS) and peripheral nervous system (PNS). The C group fibers are unmyelinated and have a small diameter and low conduction velocity, whereas Groups A a ...
associated with pain are blocked first, while thick, heavily myelinated A-alpha motor neuron
A motor neuron (or motoneuron or efferent neuron) is a neuron whose cell body is located in the motor cortex, brainstem or the spinal cord, and whose axon (fiber) projects to the spinal cord or outside of the spinal cord to directly or indirectl ...
s are blocked moderately. Heavily myelinated, small preganglionic sympathetic fibers are blocked last. The desired result is total numbness of the area. A pressure sensation is permissible and often occurs due to incomplete blockade of the thicker A-beta mechanoreceptors. This allows surgical procedures to be performed with no painful sensation to the person undergoing the procedure.
Some sedation
Sedation is the reduction of irritability or agitation by administration of sedative drugs, generally to facilitate a medical procedure or diagnostic procedure. Examples of drugs which can be used for sedation include isoflurane, diethyl ether, ...
is sometimes provided to help the patient relax and pass the time during the procedure, but with a successful spinal anaesthetic the surgery
Surgery ''cheirourgikē'' (composed of χείρ, "hand", and ἔργον, "work"), via la, chirurgiae, meaning "hand work". is a medical specialty that uses operative manual and instrumental techniques on a person to investigate or treat a pat ...
can be performed with the patient wide awake.
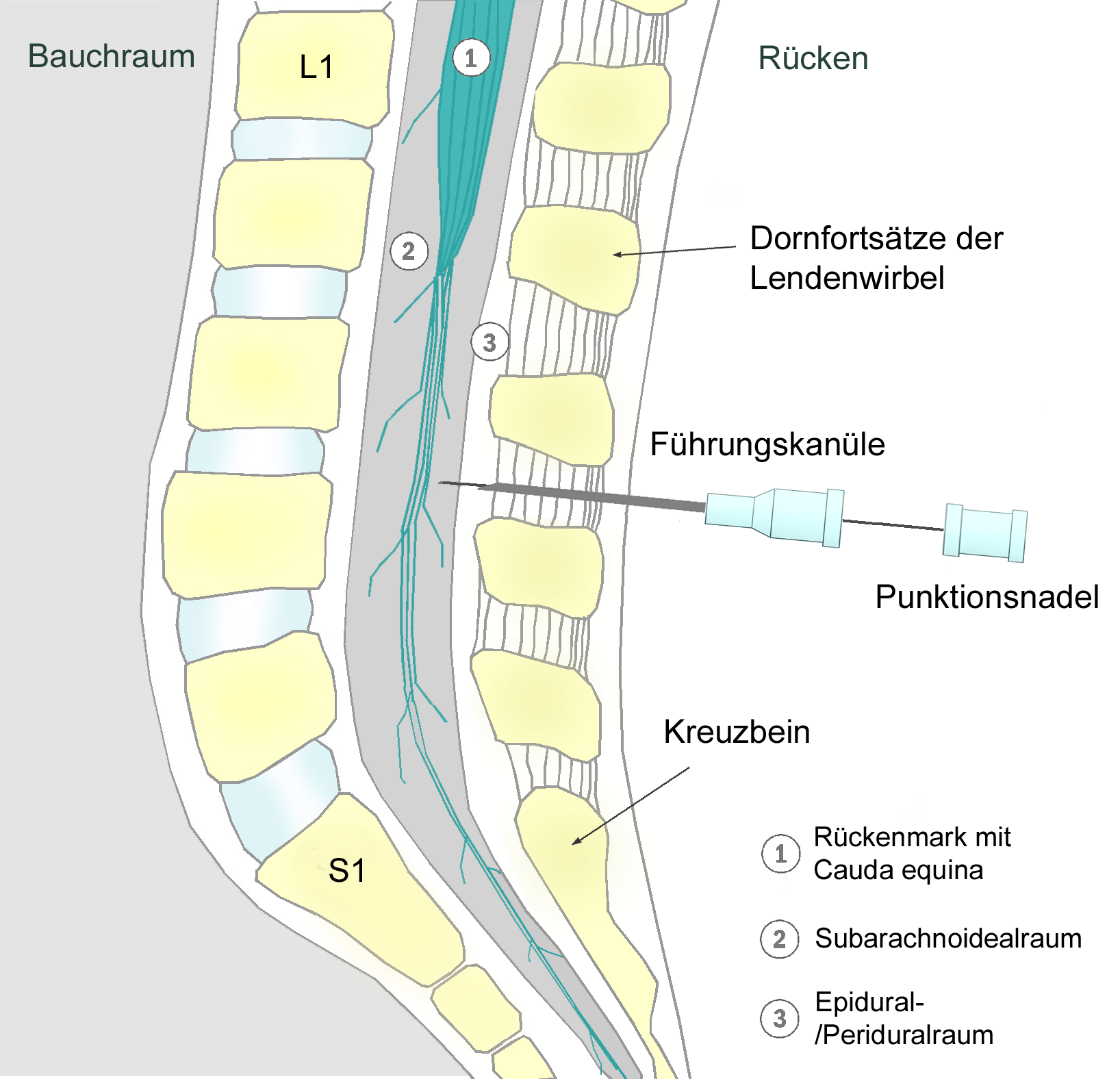
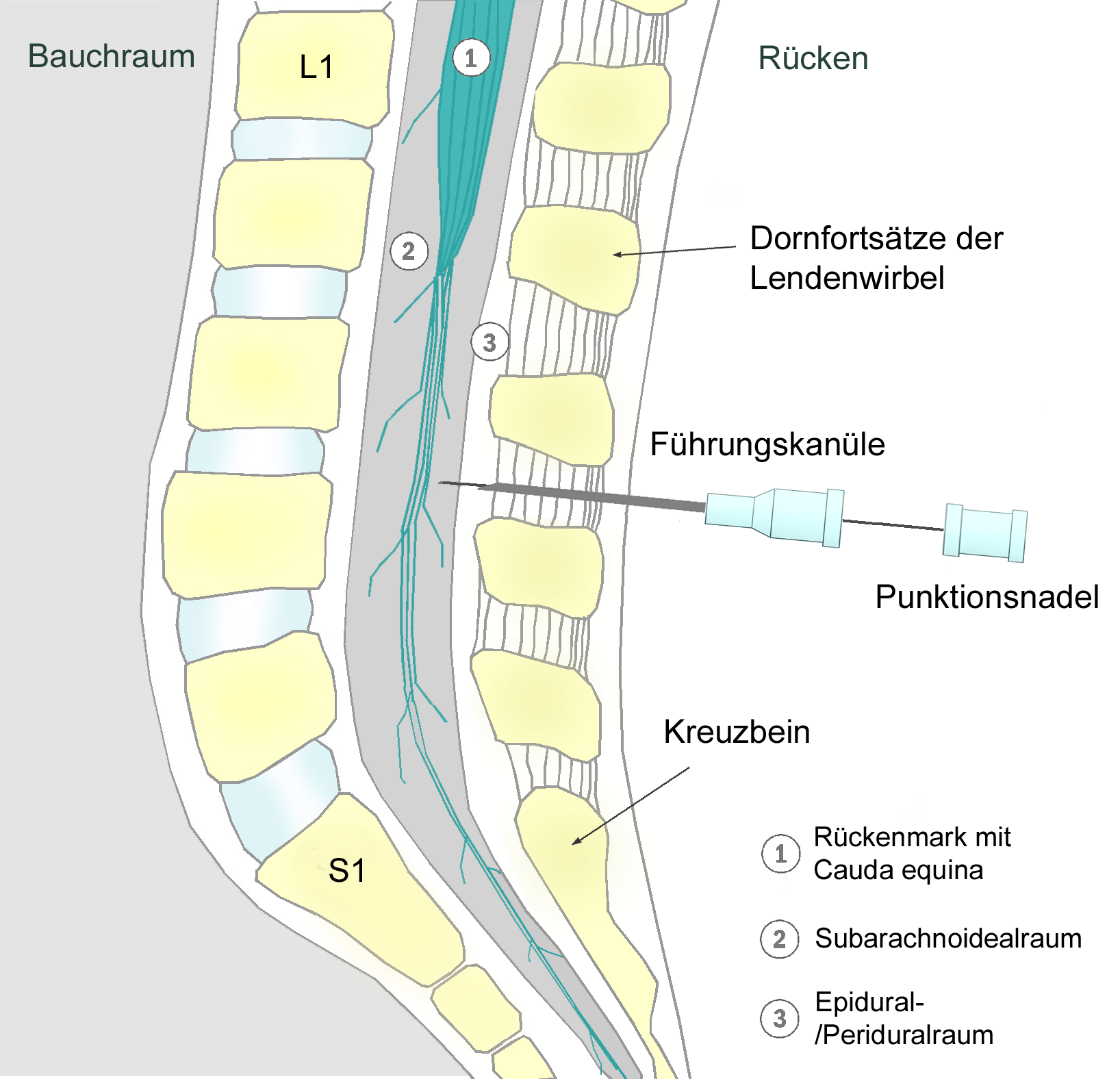
Anatomy
In spinal anesthesia, the needle is placed past the dura mater insubarachnoid space
In anatomy, the meninges (, ''singular:'' meninx ( or ), ) are the three membranes that envelop the brain and spinal cord. In mammals, the meninges are the dura mater, the arachnoid mater, and the pia mater. Cerebrospinal fluid is located in th ...
and between lumbar vertebrae. In order to reach this space, the needle must pierce through several layers of tissue and ligaments which include the supraspinous ligament, interspinous ligament, and ligamentum flavum. Because the spinal cord ( conus medullaris) is typically at the L1 or L2 level of the spine, the needle should be inserted below this between L3 and L4 space or L4 and L5 space in order to avoid injury to the spinal cord.
Positioning
Patient positioning is essential to the success of the procedure and can affect how the anesthetic spreads following administration. There are 3 different positions which are used: sitting, lateral decubitus, and prone. The sitting and lateral decubitus positions are the most common. Sitting- The patient sits upright at the edge of the exam table with their back facing the provider and their legs hanging off the end of the table and feet resting on a stool. Patients should roll their shoulders and upper back forward. Lateral decubitus- In this position, the patient lays on their side with their back at the edge of the bed and facing the provider. The patient should curl their shoulder and legs and arch out their lower back. Prone- The patient is positioned face down and their back facing upwards in a jackknife position.Limitations
Spinal anaesthetics are typically limited to procedures involving most structures below the upper abdomen. To administer a spinal anaesthetic to higher levels may affect the ability to breathe by paralysing the intercostal respiratory muscles, or even thediaphragm
Diaphragm may refer to:
Anatomy
* Thoracic diaphragm, a thin sheet of muscle between the thorax and the abdomen
* Pelvic diaphragm or pelvic floor, a pelvic structure
* Urogenital diaphragm or triangular ligament, a pelvic structure
Other
* Diap ...
in extreme cases (called a "high spinal", or a "total spinal", with which consciousness is lost), as well as the body's ability to control the heart rate via the cardiac accelerator fibres. Also, injection of spinal anaesthesia higher than the level of L1 can cause damage to the spinal cord, and is therefore usually not done.
Differences with epidural anaesthesia
 Epidural anaesthesia is a technique whereby a local anaesthetic drug is injected through a catheter placed into the epidural space. This technique is similar to spinal anaesthesia as both are neuraxial, and the two techniques may be easily confused with each other. Differences include:
* A spinal anaesthetic delivers drug to the subarachnoid space and into the cerebrospinal fluid, allowing it to act on the spinal cord directly. An epidural delivers drugs outside the dura (outside CSF), and has its main effect on nerve roots leaving the dura at the level of the epidural, rather than on the spinal cord itself.
* A spinal gives profound block of all motor and sensory function below the level of injection, whereas an epidural blocks a 'band' of nerve roots around the site of injection, with normal function above, and close-to-normal function below the levels blocked.
* The injected dose for an epidural is larger, being about 10–20 mL compared to 1.5–3.5 mL in a spinal.
* In an epidural, an indwelling catheter may be placed that allows for redosing injections, while a spinal is almost always a one-shot only. Therefore, spinal anaesthesia is more often used for shorter procedures relative to procedures which require epidural anaesthesia.
* The onset of analgesia is approximately 25–30 minutes in an epidural, while it is approximately 5 minutes in a spinal.
* An epidural often does not cause as significant a
Epidural anaesthesia is a technique whereby a local anaesthetic drug is injected through a catheter placed into the epidural space. This technique is similar to spinal anaesthesia as both are neuraxial, and the two techniques may be easily confused with each other. Differences include:
* A spinal anaesthetic delivers drug to the subarachnoid space and into the cerebrospinal fluid, allowing it to act on the spinal cord directly. An epidural delivers drugs outside the dura (outside CSF), and has its main effect on nerve roots leaving the dura at the level of the epidural, rather than on the spinal cord itself.
* A spinal gives profound block of all motor and sensory function below the level of injection, whereas an epidural blocks a 'band' of nerve roots around the site of injection, with normal function above, and close-to-normal function below the levels blocked.
* The injected dose for an epidural is larger, being about 10–20 mL compared to 1.5–3.5 mL in a spinal.
* In an epidural, an indwelling catheter may be placed that allows for redosing injections, while a spinal is almost always a one-shot only. Therefore, spinal anaesthesia is more often used for shorter procedures relative to procedures which require epidural anaesthesia.
* The onset of analgesia is approximately 25–30 minutes in an epidural, while it is approximately 5 minutes in a spinal.
* An epidural often does not cause as significant a neuromuscular block
A neuromuscular junction (or myoneural junction) is a chemical synapse between a motor neuron and a muscle fiber.
It allows the motor neuron to transmit a signal to the muscle fiber, causing muscle contraction.
Muscles require innervation to ...
as a spinal, unless specific local anaesthetics are also used which block motor fibres as readily as sensory nerve fibres.
* An epidural may be given at a cervical, thoracic, or lumbar
In tetrapod anatomy, lumbar is an adjective that means ''of or pertaining to the abdominal segment of the torso, between the diaphragm and the sacrum.''
The lumbar region is sometimes referred to as the lower spine, or as an area of the back i ...
site, while a spinal must be injected below L2 to avoid piercing the spinal cord.
Injected substances
Bupivacaine (Marcaine) is the local anaesthetic most commonly used, althoughlidocaine
Lidocaine, also known as lignocaine and sold under the brand name Xylocaine among others, is a local anesthetic of the amino amide type. It is also used to treat ventricular tachycardia. When used for local anaesthesia or in nerve blocks, lidoca ...
( lignocaine), tetracaine, procaine, ropivacaine, levobupivicaine
Levobupivacaine (rINN) is a local anaesthetic drug belonging to the amino amide group. It is the ''S''- enantiomer of bupivacaine.
Levobupivacaine hydrochloride is commonly marketed by AbbVie under the trade name Chirocaine.Rossi S, editor. Aust ...
, prilocaine, or cinchocaine may also be used. Commonly opioids
Opioids are substances that act on opioid receptors to produce morphine-like effects. Medically they are primarily used for pain relief, including anesthesia. Other medical uses include suppression of diarrhea, replacement therapy for opioid use ...
are added to improve the block and provide post-operative pain relief, examples include morphine, fentanyl, diamorphine, and buprenorphine. Non-opioids like clonidine
Clonidine, sold under the brand name Catapres among others, is an α2-adrenergic agonist medication used to treat high blood pressure, ADHD, drug withdrawal ( alcohol, opioids, or nicotine), menopausal flushing, diarrhea, spasticity, and c ...
or epinephrine
Adrenaline, also known as epinephrine, is a hormone and medication which is involved in regulating visceral functions (e.g., respiration). It appears as a white microcrystalline granule. Adrenaline is normally produced by the adrenal glands and ...
may also be added to prolong the duration of analgesia (although Clonidine may cause hypotension). In the United Kingdom, since 2004 the National Institute for Health and Care Excellence recommends that spinal anaesthesia for Caesarean section is supplemented with intrathecal diamorphine and this combination is now the modal form of anaesthesia for this indication in that country. In the United States Morphine is used for cesareans for the same purpose since diamorphine (heroin) is not used in clinical practice in the US.
Baricity
Baricity refers to the density of a substance compared to the density of human cerebrospinal fluid. Baricity is used in anesthesia to determine the manner in which a particular drug will spread in the intrathecal
Intrathecal administration is a ...
refers to the density of a substance compared to the density of human cerebrospinal fluid. Baricity is used in anaesthesia to determine the manner in which a particular drug will spread in the intrathecal space. Usually, the hyperbaric, (for example, hyperbaric bupivacaine) is chosen, as its spread can be effectively and predictably controlled by the Anaesthesiologist, by tilting the patient. Hyperbaric solutions are made more dense by adding glucose to the mixture.
Baricity
Baricity refers to the density of a substance compared to the density of human cerebrospinal fluid. Baricity is used in anesthesia to determine the manner in which a particular drug will spread in the intrathecal
Intrathecal administration is a ...
is one factor that determines the spread of a spinal anaesthetic but the effect of adding a solute to a solvent, i.e. solvation or dissolution, also has an effect on the spread of the spinal anaesthetic. In tetracaine spinal anaesthesia, it was discovered that the rate of onset of analgesia was faster and the maximum level of analgesia was higher with a 10% glucose solution than with a 5% glucose spinal anaesthetic solution. Also, the amount of ephedrine required was less in the patients who received the 5% glucose solution. In another study this time with 0.5% bupivacaine the mean maximum extent of sensory block was significantly higher with 8% glucose (T3.6) than with 0.83% glucose (T7.2) or 0.33% glucose (T9.5). Also the rate of onset of sensory block to T12 was fastest with solutions containing 8% glucose./ref>
History
The first spinal analgesia was administered in 1885 byJames Leonard Corning
James Leonard Corning (1855 – 1923) was an American neurologist, mainly known for his early experiments on neuraxial blockade in New York City.
Education
Corning was born in Stamford, Connecticut. When the American Civil War began in 1861 ...
(1855–1923), a neurologist in New York.Corning J. L. N.Y. Med. J. 1885, 42, 483 (reprinted in 'Classical File', ''Survey of Anesthesiology'' 1960, 4, 332) He was experimenting with cocaine on the spinal nerves of a dog when he accidentally pierced the dura mater.
The first planned spinal anaesthesia for surgery on a human was administered by August Bier
August Karl Gustav Bier (24 November 1861 – 12 March 1949) was a German surgeon. He was the first to perform spinal anesthesia and intravenous regional anesthesia.
Early medical career
Bier began his medical education at the Charité – Uni ...
(1861–1949) on 16 August 1898, in Kiel, when he injected 3 ml of 0.5% cocaine solution into a 34-year-old labourer.Bier A. Versuche über Cocainisirung des Rückenmarkes. ''Deutsch Zeitschrift für Chirurgie'' 1899;51:361. (translated and reprinted in 'Classical File', ''Survey of Anesthesiology'' 1962, 6, 352) After using it on 6 patients, he and his assistant each injected cocaine into the other's spine
Spine or spinal may refer to:
Science Biology
* Vertebral column, also known as the backbone
* Dendritic spine, a small membranous protrusion from a neuron's dendrite
* Thorns, spines, and prickles, needle-like structures in plants
* Spine (zoolog ...
. They recommended it for surgeries of legs, but gave it up due to the toxicity of cocaine.
See also
* Combined spinal and epidural anaesthesia * Epidural * Intrathecal administration *Lumbar puncture
Lumbar puncture (LP), also known as a spinal tap, is a medical procedure in which a needle is inserted into the spinal canal, most commonly to collect cerebrospinal fluid (CSF) for diagnostic testing. The main reason for a lumbar puncture is to ...
References
External links
Transparent reality simulation of spinal anaesthesia
Various diagrams of needles for Lumbar puncture, Epidural, Spinal Anesthesia, etc
{{DEFAULTSORT:Spinal Anaesthesia Regional anesthesia