|
Length Of Stay
Length of stay (LOS) is the duration of a single episode of hospitalization. patient, Inpatient days are calculated by subtracting day of admission from day of :wikt:discharge, discharge. Analysis A common statistic associated with length of stay is the average length of stay (ALOS), a mean calculated by dividing the sum of inpatient days by the number of patients admissions with the same diagnosis-related group classification. A variation in the calculation of ALOS can be to consider only length of stay during the period under analysis. Length of stay is typically highly skewness, skewed and so statistical approaches taking that into account are recommended. While the mean length of stay is useful from the point of view of costs, it may be a poor statistic in terms of representing a typical length of stay, and the median may be preferred. It is useful to be able to predict an individual's expected length of stay or to model length of stay to determine factors that affect it. Vari ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |
Hospital
A hospital is a healthcare institution providing patient treatment with specialized Medical Science, health science and auxiliary healthcare staff and medical equipment. The best-known type of hospital is the general hospital, which typically has an emergency department to treat urgent health problems ranging from fire and accident victims to a sudden illness. A district hospital typically is the major health care facility in its region, with many beds for intensive care and additional beds for patients who need long-term care. Specialized hospitals include trauma centers, rehabilitation hospitals, children's hospitals, geriatric hospitals, and hospitals for specific medical needs, such as psychiatric hospitals for psychiatry, psychiatric treatment and other disease-specific categories. Specialized hospitals can help reduce health care costs compared to general hospitals. Hospitals are classified as general, specialty, or government depending on the sources of income received. ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |
Patient
A patient is any recipient of health care services that are performed by Health professional, healthcare professionals. The patient is most often Disease, ill or Major trauma, injured and in need of therapy, treatment by a physician, nurse, optometrist, dentist, veterinarian, or other health care provider. Etymology The word wikt:patient, patient originally meant 'one who suffers'. This English noun comes from the Latin word , the present participle of the deponent verb, , meaning , and akin to the Ancient Greek, Greek verb ( ) and its cognate noun (). This language has been construed as meaning that the role of patients is to passively accept and tolerate the suffering and treatments prescribed by the healthcare providers, without engaging in Shared decision-making in medicine, shared decision-making about their care. Outpatients and inpatients An outpatient (or out-patient) is a patient who attends an Outpatient clinic (hospital department), outpatient clinic with no ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |
Diagnosis-related Group
Diagnosis-related group (DRG) is a system to classify hospital cases into one of originally 467 groups, with the last group (coded as 470 through v24, 999 thereafter) being "Ungroupable". This system of classification was developed as a collaborative project by Robert B Fetter, PhD, of the Yale School of Management, and John D. Thompson, MPH, of the Yale School of Public Health.Fetter RB, Shin Y, Freeman JL, Averill RF, Thompson JD (1980) Case mix definition by diagnosis related groups. Medical Care 18(2):1–53 The system is also referred to as "the DRGs", and its intent was to identify the "products" that a hospital provides. One example of a "product" is an appendectomy. The system was developed in anticipation of convincing Congress to use it for reimbursement, to replace "cost based" reimbursement that had been used up to that point. DRGs are assigned by a "grouper" program based on ICD (International Classification of Diseases) diagnoses, procedures, age, sex, discharge ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |
Skewness
In probability theory and statistics, skewness is a measure of the asymmetry of the probability distribution of a real-valued random variable about its mean. The skewness value can be positive, zero, negative, or undefined. For a unimodal distribution (a distribution with a single peak), negative skew commonly indicates that the ''tail'' is on the left side of the distribution, and positive skew indicates that the tail is on the right. In cases where one tail is long but the other tail is fat, skewness does not obey a simple rule. For example, a zero value in skewness means that the tails on both sides of the mean balance out overall; this is the case for a symmetric distribution but can also be true for an asymmetric distribution where one tail is long and thin, and the other is short but fat. Thus, the judgement on the symmetry of a given distribution by using only its skewness is risky; the distribution shape must be taken into account. Introduction Consider the two d ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |
Median
The median of a set of numbers is the value separating the higher half from the lower half of a Sample (statistics), data sample, a statistical population, population, or a probability distribution. For a data set, it may be thought of as the “middle" value. The basic feature of the median in describing data compared to the Arithmetic mean, mean (often simply described as the "average") is that it is not Skewness, skewed by a small proportion of extremely large or small values, and therefore provides a better representation of the center. Median income, for example, may be a better way to describe the center of the income distribution because increases in the largest incomes alone have no effect on the median. For this reason, the median is of central importance in robust statistics. Median is a 2-quantile; it is the value that partitions a set into two equal parts. Finite set of numbers The median of a finite list of numbers is the "middle" number, when those numbers are liste ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |
Markov Chain
In probability theory and statistics, a Markov chain or Markov process is a stochastic process describing a sequence of possible events in which the probability of each event depends only on the state attained in the previous event. Informally, this may be thought of as, "What happens next depends only on the state of affairs ''now''." A countably infinite sequence, in which the chain moves state at discrete time steps, gives a discrete-time Markov chain (DTMC). A continuous-time process is called a continuous-time Markov chain (CTMC). Markov processes are named in honor of the Russian mathematician Andrey Markov. Markov chains have many applications as statistical models of real-world processes. They provide the basis for general stochastic simulation methods known as Markov chain Monte Carlo, which are used for simulating sampling from complex probability distributions, and have found application in areas including Bayesian statistics, biology, chemistry, economics, fin ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |
Negative Binomial
In probability theory and statistics, the negative binomial distribution, also called a Pascal distribution, is a discrete probability distribution that models the number of failures in a sequence of independent and identically distributed Bernoulli trials before a specified/constant/fixed number of successes r occur. For example, we can define rolling a 6 on some dice as a success, and rolling any other number as a failure, and ask how many failure rolls will occur before we see the third success (r=3). In such a case, the probability distribution of the number of failures that appear will be a negative binomial distribution. An alternative formulation is to model the number of total trials (instead of the number of failures). In fact, for a specified (non-random) number of successes , the number of failures is random because the number of total trials is random. For example, we could use the negative binomial distribution to model the number of days (random) a certain machin ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |
Prospective Payment System
A prospective payment system (PPS) is a term used to refer to several payment methodologies for which means of determining insurance reimbursement is based on a predetermined payment regardless of the intensity of the actual service provided. It includes a system for paying hospitals based on predetermined prices, from Medicare (United States), Medicare. Payments are typically based on codes provided on the insurance claim such as these: * Diagnosis-related groups for hospital inpatient claims * Ambulatory Payment Classification for hospital outpatient claims * Current Procedural Terminology for other outpatient claims The PPS was established by the Centers for Medicare and Medicaid Services (CMS), as a result of the Social Security Amendments Act of 1983, specifically to address expensive hospital care. Regardless of services provided, payment was of an established fee. The idea was to encourage hospitals to lower their prices for expensive hospital care. In 2000, CMS changed th ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |
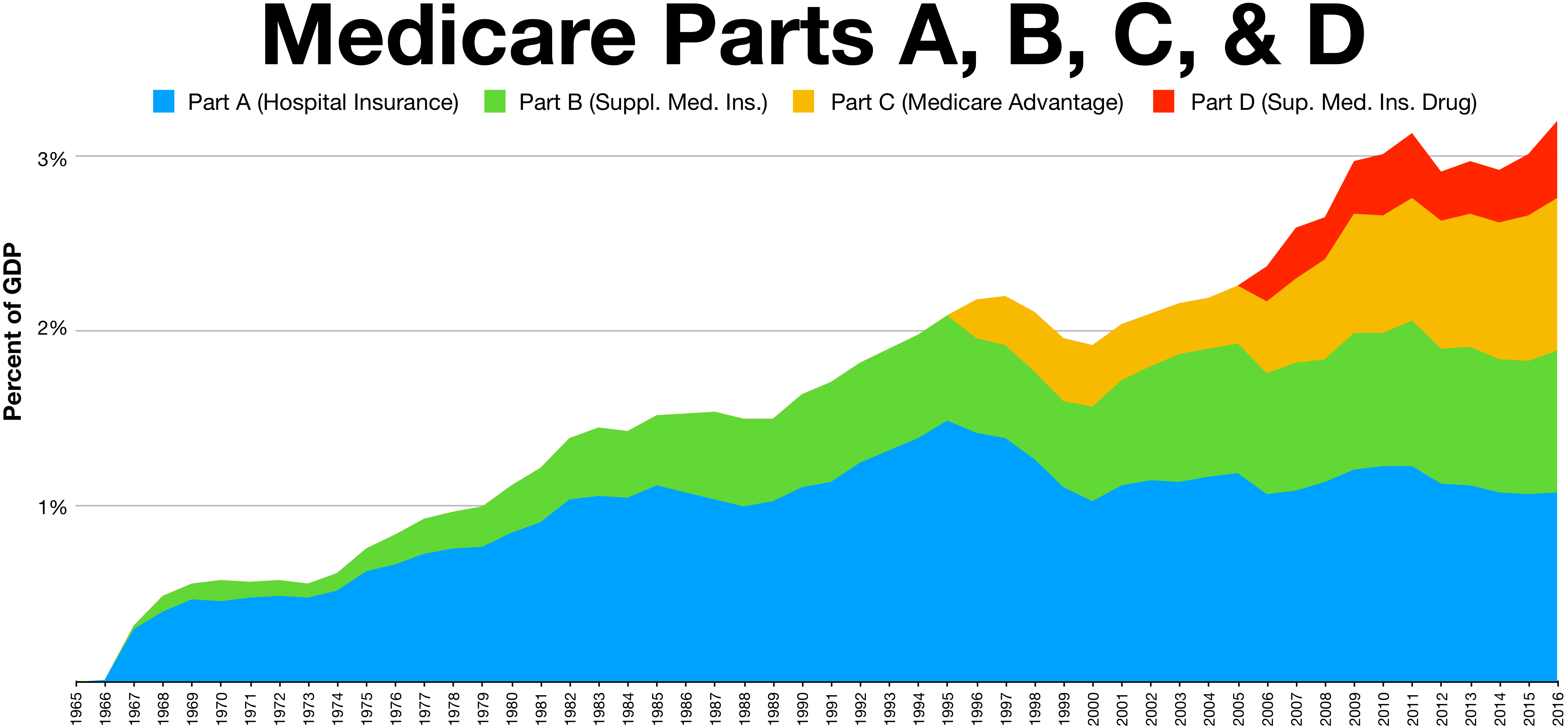
Medicare (United States)
Medicare is a federal health insurance program in the United States for people age 65 or older and younger people with disabilities, including those with End Stage Renal Disease Program, end stage renal disease and amyotrophic lateral sclerosis (ALS or Lou Gehrig's disease). It started in 1965 under the Social Security Administration and is now administered by the Centers for Medicare and Medicaid Services (CMS). Medicare is divided into four parts: A, B, C and D. Part A covers hospital, skilled nursing, and hospice services. Part B covers outpatient services. Part D covers self-administered prescription drugs. Part C is an alternative that allows patients to choose private plans with different benefit structures that provide the same services as Parts A and B, usually with additional benefits. In 2022, Medicare provided health insurance for 65.0 million individuals—more than 57 million people aged 65 and older and about 8 million younger people. According to annual Medicare ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |
Inpatient Care
Inpatient care is the care of patients whose condition requires admission to a hospital. Progress in modern medicine and the advent of comprehensive out-patient clinics ensure that patients are only admitted to a hospital when they are extremely ill or have severe physical trauma. Progress Patients enter inpatient care mainly from previous ambulatory care such as referral from a family doctor, or through emergency medicine departments. The patient formally becomes an " inpatient" at the writing of an admission note. Likewise, it is formally ended by writing a discharge note. Planning for patient discharge Health care professionals involved in rehabilitation are often involved in discharge planning for patients. When considering patient discharge, there are a number of factors to take into consideration: the patient's current state, their place of residence and the type of support available. When considering the patient's current state, although the patient may be eligible f ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |