ö Cells on:
[Wikipedia]
[Google]
[Amazon]
Beta cells (öý-cells) are specialized
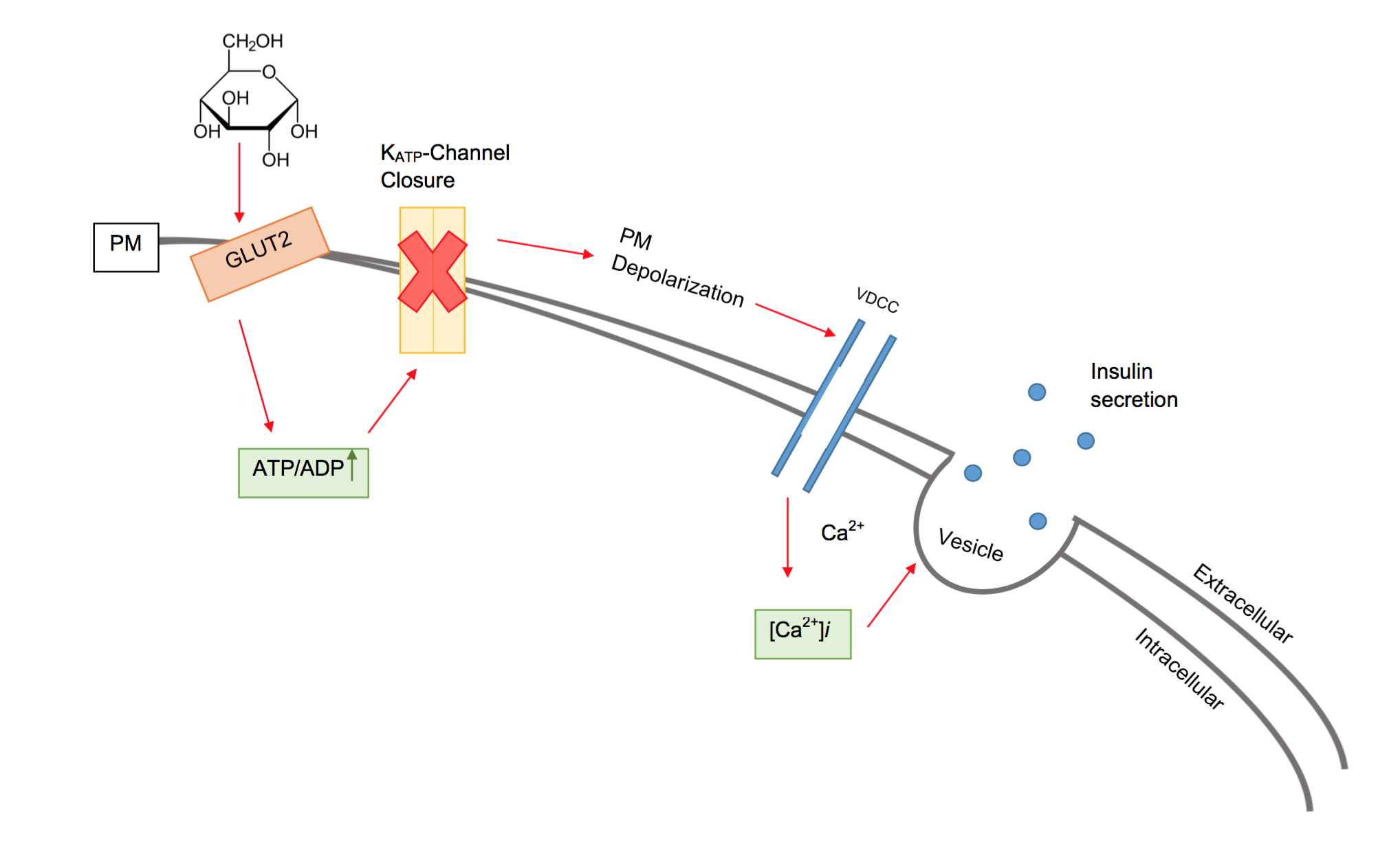 In beta cells, insulin release is stimulated primarily by glucose present in the blood. As circulating glucose levels rise, such as after ingesting a meal, insulin is secreted in a dose-dependent fashion. This system of release is commonly referred to as glucose-stimulated insulin secretion (GSIS). There are four key events to the triggering pathway of GSIS: GLUT dependent glucose uptake, glucose metabolism, KATP channel closure, and the opening of voltage gated calcium channels causing insulin granule fusion and exocytosis.
In beta cells, insulin release is stimulated primarily by glucose present in the blood. As circulating glucose levels rise, such as after ingesting a meal, insulin is secreted in a dose-dependent fashion. This system of release is commonly referred to as glucose-stimulated insulin secretion (GSIS). There are four key events to the triggering pathway of GSIS: GLUT dependent glucose uptake, glucose metabolism, KATP channel closure, and the opening of voltage gated calcium channels causing insulin granule fusion and exocytosis.
endocrine
The endocrine system is a messenger system in an organism comprising feedback loops of hormones that are released by internal glands directly into the circulatory system and that target and regulate distant organs. In vertebrates, the hypotha ...
cells
Cell most often refers to:
* Cell (biology), the functional basic unit of life
* Cellphone, a phone connected to a cellular network
* Clandestine cell, a penetration-resistant form of a secret or outlawed organization
* Electrochemical cell, a d ...
located within the pancreatic islets
The pancreatic islets or islets of Langerhans are the regions of the pancreas that contain its endocrine (hormone-producing) cells, discovered in 1869 by German pathological anatomist Paul Langerhans. The pancreatic islets constitute 1ã2% o ...
of Langerhans responsible for the production and release of insulin
Insulin (, from Latin ''insula'', 'island') is a peptide hormone produced by beta cells of the pancreatic islets encoded in humans by the insulin (''INS)'' gene. It is the main Anabolism, anabolic hormone of the body. It regulates the metabol ...
and amylin
Amylin, or islet amyloid polypeptide (IAPP), is a 37-residue peptide hormone. It is co-secreted with insulin from the pancreatic öý-cells in the ratio of approximately 100:1 (insulin:amylin). Amylin plays a role in glycemic regulation by slo ...
. Constituting ~50ã70% of cells in human islets, beta cells play a vital role in maintaining blood glucose
Glucose is a sugar with the Chemical formula#Molecular formula, molecular formula , which is often abbreviated as Glc. It is overall the most abundant monosaccharide, a subcategory of carbohydrates. It is mainly made by plants and most algae d ...
levels. Problems with beta cells can lead to disorders such as diabetes
Diabetes mellitus, commonly known as diabetes, is a group of common endocrine diseases characterized by sustained high blood sugar levels. Diabetes is due to either the pancreas not producing enough of the hormone insulin, or the cells of th ...
.
Function
The function of beta cells is primarily centered around the synthesis and secretion ofhormone
A hormone (from the Ancient Greek, Greek participle , "setting in motion") is a class of cell signaling, signaling molecules in multicellular organisms that are sent to distant organs or tissues by complex biological processes to regulate physio ...
s, particularly insulin and amylin. Both hormones work to keep blood glucose levels within a narrow, healthy range by different mechanisms. Insulin facilitates the uptake of glucose by cells, allowing them to use it for energy or store it for future use. Amylin helps regulate the rate at which glucose enters the bloodstream after a meal, slowing down the absorption of nutrients by inhibit gastric emptying.
Insulin synthesis
Beta cells are the only site of insulin synthesis in mammals. As glucose stimulates insulin secretion, it simultaneously increases proinsulin biosynthesis through translational control and enhanced gene transcription. The insulin gene is first transcribed into mRNA and translated into preproinsulin. After translation, the preproinsulin precursor contains an N-terminal signal peptide that allows translocation into therough endoplasmic reticulum
The endoplasmic reticulum (ER) is a part of a transportation system of the eukaryotic cell, and has many other important functions such as protein folding. The word endoplasmic means "within the cytoplasm", and reticulum is Latin for "little n ...
(RER). Inside the RER, the signal peptide is cleaved to form proinsulin. Then, folding of proinsulin occurs forming three disulfide bonds. Subsequent to protein folding, proinsulin is transported to the Golgi apparatus and enters immature insulin granules where proinsulin is cleaved to form insulin and C-peptide
The connecting peptide, or C-peptide, is a short 31-amino-acid polypeptide that connects insulin's A-chain to its B-chain in the proinsulin molecule. In the context of diabetes or hypoglycemia, a measurement of C-peptide blood serum levels ...
. After maturation, these secretory vesicles hold insulin, C-peptide, and amylin until calcium triggers exocytosis
Exocytosis is a term for the active transport process that transports large molecules from cell to the extracellular area. Hormones, proteins and neurotransmitters are examples of large molecules that can be transported out of the cell. Exocytosis ...
of the granule contents.
Through translational processing, insulin is encoded as a 110 amino acid precursor but is secreted as a 51 amino acid protein.
Insulin secretion
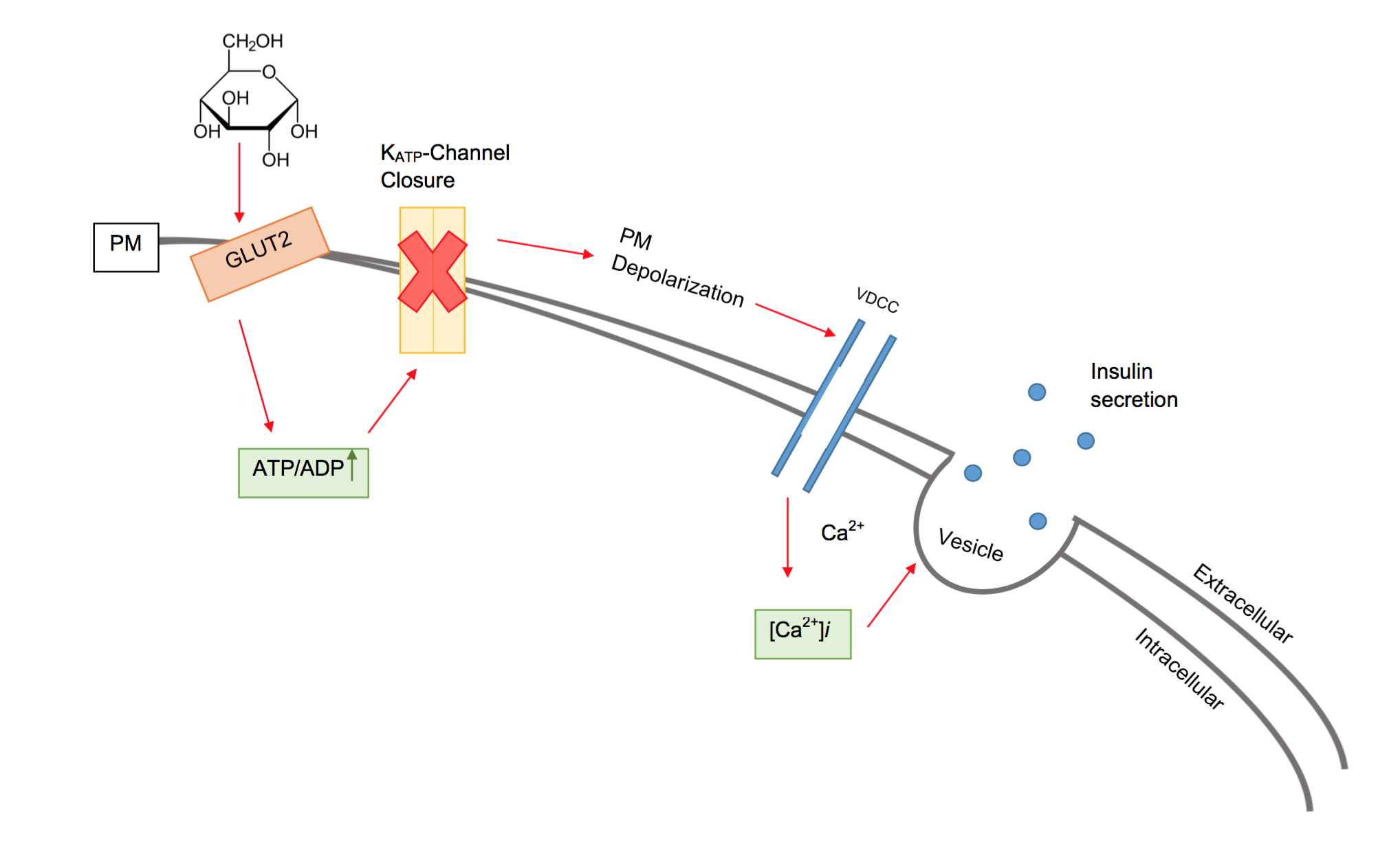 In beta cells, insulin release is stimulated primarily by glucose present in the blood. As circulating glucose levels rise, such as after ingesting a meal, insulin is secreted in a dose-dependent fashion. This system of release is commonly referred to as glucose-stimulated insulin secretion (GSIS). There are four key events to the triggering pathway of GSIS: GLUT dependent glucose uptake, glucose metabolism, KATP channel closure, and the opening of voltage gated calcium channels causing insulin granule fusion and exocytosis.
In beta cells, insulin release is stimulated primarily by glucose present in the blood. As circulating glucose levels rise, such as after ingesting a meal, insulin is secreted in a dose-dependent fashion. This system of release is commonly referred to as glucose-stimulated insulin secretion (GSIS). There are four key events to the triggering pathway of GSIS: GLUT dependent glucose uptake, glucose metabolism, KATP channel closure, and the opening of voltage gated calcium channels causing insulin granule fusion and exocytosis.
Voltage-gated calcium channels
Voltage-gated calcium channels (VGCCs), also known as voltage-dependent calcium channels (VDCCs), are a group of voltage-gated ion channels found in the membrane of excitable cells (''e.g.'' muscle, glial cells, neurons) with a permeability to ...
and ATP-sensitive potassium ion channels (KATP channels) are embedded in the plasma membrane of beta cells. Under non-glucose stimulated conditions, the KATP channels are open and the voltage gated calcium channels are closed. Via the KATP channels, potassium ions move out of the cell, down their concentration gradient, making the inside of the cell more negative with respect to the outside (as potassium ions carry a positive charge). At rest, this creates a potential difference
Voltage, also known as (electrical) potential difference, electric pressure, or electric tension, is the difference in electric potential between two points. In a static electric field, it corresponds to the work needed per unit of charge ...
across the cell surface membrane of -70mV.
When the glucose concentration outside the cell is high, glucose molecules move into the cell by facilitated diffusion
Facilitated diffusion (also known as facilitated transport or passive-mediated transport) is the process of spontaneous passive transport (as opposed to active transport) of molecules or ions across a biological membrane via specific transmembr ...
, down its concentration gradient through glucose transporter
Glucose transporters are a wide group of membrane proteins that facilitate the transport of glucose across the plasma membrane, a process known as facilitated diffusion. Because glucose is a vital source of energy for all life, these transporte ...
s (GLUT). Rodent beta cells primarily express the GLUT2
Glucose transporter 2 (GLUT2) also known as solute carrier family 2 (facilitated glucose transporter), member 2 (SLC2A2) is a transmembrane carrier protein that enables protein facilitated glucose movement across cell membranes. It is the princi ...
isoform, whereas human beta cells, although also expressing GLUT2, mainly make use of GLUT1
Glucose transporter 1 (or GLUT1), also known as solute carrier family 2, facilitated glucose transporter member 1 (SLC2A1), is a uniporter protein that in humans is encoded by the ''SLC2A1'' gene. GLUT1 facilitates the transport of glucose acro ...
and GLUT3
Glucose transporter 3 (or GLUT3), also known as solute carrier family 2, facilitated glucose transporter member 3 (SLC2A3) is a protein that in humans is encoded by the ''SLC2A3'' gene. GLUT3 facilitates the transport of glucose across the plas ...
isoforms. Since beta cells use glucokinase
Glucokinase () is an enzyme that facilitates phosphorylation of glucose to glucose-6-phosphate. Glucokinase is expressed in cells of the liver and pancreas of humans and most other vertebrates. In each of these organs it plays an important ro ...
to catalyze the first step of glycolysis
Glycolysis is the metabolic pathway that converts glucose () into pyruvic acid, pyruvate and, in most organisms, occurs in the liquid part of cells (the cytosol). The Thermodynamic free energy, free energy released in this process is used to form ...
, metabolism only occurs around physiological blood glucose
The blood sugar level, blood sugar concentration, blood glucose level, or glycemia is the measure of glucose concentrated in the blood. The body tightly blood sugar regulation, regulates blood glucose levels as a part of metabolic homeostasis ...
levels and above. Metabolism of glucose produces ATP, which increases the ATP to ADP ratio.
The KATP channels close when the ATP to ADP ratio rises. The closure of the KATP channels causes the outward potassium ion current to diminish, leading to inward currents of potassium ions dominating. As a result, the potential difference across the membrane becomes more positive (as potassium ions accumulate inside the cell). This change in potential difference opens the voltage-gated calcium channels
Voltage-gated calcium channels (VGCCs), also known as voltage-dependent calcium channels (VDCCs), are a group of voltage-gated ion channels found in the membrane of excitable cells (''e.g.'' muscle, glial cells, neurons) with a permeability to ...
, which allows calcium ions from outside the cell to move into the cell down their concentration gradient. When the calcium ions enter the cell, they cause vesicles
Vesicle may refer to:
; In cellular biology or chemistry
* Vesicle (biology and chemistry), a supramolecular assembly of lipid molecules, like a cell membrane
* Synaptic vesicle
In a neuron, synaptic vesicles (or neurotransmitter vesicles) s ...
containing insulin to move to, and fuse with, the cell surface membrane, releasing insulin by exocytosis
Exocytosis is a term for the active transport process that transports large molecules from cell to the extracellular area. Hormones, proteins and neurotransmitters are examples of large molecules that can be transported out of the cell. Exocytosis ...
into the pancreatic capillaries. The venous blood then eventually empties into the hepatic portal vein.
In addition to the triggering pathway, the amplifying pathway can cause increased insulin secretion without a further increase in intracellular calcium levels. The amplifying pathway is modulated by byproducts of glucose metabolism along with various intracellular signaling pathways; incretin
Incretins are a group of metabolic hormones that decrease Blood sugar level, blood glucose levels. Incretins are released after eating and augment the secretion of insulin released from Pancreas, pancreatic beta cells of the islets of Langerhans ...
hormone signaling being one important example.
Other hormones secreted
*C-peptide
The connecting peptide, or C-peptide, is a short 31-amino-acid polypeptide that connects insulin's A-chain to its B-chain in the proinsulin molecule. In the context of diabetes or hypoglycemia, a measurement of C-peptide blood serum levels ...
, which is secreted into the bloodstream in equimolar quantities to insulin. C-peptide helps to prevent neuropathy and other vascular deterioration related symptoms of diabetes mellitus
Diabetes mellitus, commonly known as diabetes, is a group of common endocrine diseases characterized by sustained hyperglycemia, high blood sugar levels. Diabetes is due to either the pancreas not producing enough of the hormone insulin, or th ...
. A practitioner would measure the levels of C-peptide to obtain an estimate for the viable beta cell mass.
* Amylin
Amylin, or islet amyloid polypeptide (IAPP), is a 37-residue peptide hormone. It is co-secreted with insulin from the pancreatic öý-cells in the ratio of approximately 100:1 (insulin:amylin). Amylin plays a role in glycemic regulation by slo ...
, also known as islet amyloid polypeptide (IAPP). The function of amylin is to slow the rate of glucose entering the bloodstream. Amylin can be described as a synergistic partner to insulin, where insulin regulates long term food intake and amylin regulates short term food intake.
Clinical significance
Beta cells have significant clinical relevance as their proper function is essential for glucose regulation, and dysfunction is a key factor in the development and progression of diabetes and its associated complications. Here are some key clinical significances of beta cells:Type 1 diabetes
Type 1 diabetes mellitus
Type 1 diabetes (T1D), formerly known as juvenile diabetes, is an autoimmune disease that occurs when the body's immune system destroys pancreatic cells (beta cells). In healthy persons, beta cells produce insulin. Insulin is a hormone required ...
, also known as insulin-dependent diabetes, is believed to be caused by an auto-immune mediated destruction of the insulin-producing beta cells in the body. The process of beta-cell destruction begins with insulitis activating antigen-presenting cells (APCs). APCs then trigger activation of CD4+ helper-T cells and chemokines/cytokines release. Then, the cytokines activate CD8+ cytotoxicãT cells which leads to beta-cell destruction. The destruction of these cells reduces the body's ability to respond to glucose levels in the body, therefore making it nearly impossible to properly regulate glucose and glucagon levels in the bloodstream. The body destroys 70ã80% of beta cells, leaving only 20ã30% of functioning cells. This can cause the patient to experience hyperglycemia, which leads to other adverse short-term and long-term conditions. The symptoms of diabetes can potentially be controlled with methods such as regular doses of insulin and sustaining a proper diet. However, these methods can be tedious and cumbersome to continuously perform on a daily basis.
Type 2 diabetes
Type 2 diabetes
Type 2 diabetes (T2D), formerly known as adult-onset diabetes, is a form of diabetes mellitus that is characterized by high blood sugar, insulin resistance, and relative lack of insulin. Common symptoms include increased thirst, frequent ...
, also known as non insulin dependent diabetes and as chronic hyperglycemia, is caused primarily by genetics and the development of metabolic syndrome. The beta cells can still secrete insulin but the body has developed a resistance and its response to insulin has declined. It is believed to be due to the decline of specific receptors on the surface of the liver
The liver is a major metabolic organ (anatomy), organ exclusively found in vertebrates, which performs many essential biological Function (biology), functions such as detoxification of the organism, and the Protein biosynthesis, synthesis of var ...
, adipose
Adipose tissue (also known as body fat or simply fat) is a loose connective tissue composed mostly of adipocytes. It also contains the stromal vascular fraction (SVF) of cells including preadipocytes, fibroblasts, Blood vessel, vascular endothel ...
, and muscle cells
A muscle cell, also known as a myocyte, is a mature contractile cell in the muscle of an animal. In humans and other vertebrates there are three types: skeletal, smooth, and cardiac (cardiomyocytes). A skeletal muscle cell is long and threadli ...
which lose their ability to respond to insulin that circulates in the blood. In an effort to secrete enough insulin to overcome the increasing insulin resistance, the beta cells increase their function, size and number. Increased insulin secretion leads to hyperinsulinemia, but blood glucose levels remain within their normal range due to the decreased efficacy of insulin signaling. However, the beta cells can become overworked and exhausted from being overstimulated, leading to a 50% reduction in function along with a 40% decrease in beta-cell volume. At this point, not enough insulin can be produced and secreted to keep blood glucose levels within their normal range, causing overt type 2 diabetes.
Insulinoma
Insulinoma
An insulinoma is a tumour of the pancreas that is derived from beta cells and secretes insulin. It is a rare form of a neuroendocrine tumour. Most insulinomas are benign in that they grow exclusively at their origin within the pancreas, but a m ...
is a rare tumor derived from the neoplasia of beta cells. Insulinomas are usually benign
Malignancy () is the tendency of a medical condition to become progressively worse; the term is most familiar as a characterization of cancer.
A ''malignant'' tumor contrasts with a non-cancerous benign tumor, ''benign'' tumor in that a malig ...
, but may be medically significant and even life-threatening due to recurrent and prolonged attacks of hypoglycemia
Hypoglycemia (American English), also spelled hypoglycaemia or hypoglycûÎmia (British English), sometimes called low blood sugar, is a fall in blood sugar to levels below normal, typically below 70 mg/dL (3.9 mmol/L). Whipple's tria ...
.
Medications
Many drugs to combat diabetes are aimed at modifying the function of the beta cell. * Sulfonylureas are insulin secretagogues that act by closing the ATP-sensitive potassium channels, thereby causing insulin release. These drugs are known to cause hypoglycemia and can lead to beta-cell failure due to overstimulation. Second-generation versions of sulfonylureas are shorter acting and less likely to cause hypoglycemia. * GLP-1 receptor agonists stimulate insulin secretion by simulating activation of the body's endogenous incretin system. The incretin system acts as an insulin secretion amplifying pathway. * DPP-4 inhibitors block DPP-4 activity which increases postprandial incretin hormone concentration, therefore increasing insulin secretion.Research
Experimental techniques
Many researchers around the world are investigating the pathogenesis of diabetes and beta-cell failure. Tools used to study beta-cell function are expanding rapidly with technology. For instance, transcriptomics have allowed researchers to comprehensively analyze gene transcription in beta-cells to look for genes linked to diabetes. A more common mechanism of analyzing cellular function is calcium imaging. Fluorescent dyes bind to calcium and allow ''in vitro'' imaging of calcium activity which correlates directly with insulin release. A final tool used in beta-cell research are ''in vivo'' experiments. Diabetes mellitus can be experimentally induced ''in vivo'' for research purposes bystreptozotocin
Streptozotocin or streptozocin ( INN, USP) (STZ) is a naturally occurring alkylating antineoplastic agent that is particularly toxic to the insulin-producing beta cells of the pancreas in mammals. It is used in medicine for treating certain can ...
or alloxan
Alloxan, sometimes referred to as alloxan monohydrate, is an organic compound with the formula . It is classified as a derivative of pyrimidine. The anhydrous derivative is also known, as well as a dimeric derivative. These are some of the earlie ...
, which are specifically toxic to beta cells. Mouse and rat models of diabetes also exist including ob/ob and db/db mice which are a type 2 diabetes model, and non-obese diabetic mice (NOD) which are a model for type 1 diabetes.
Type 1 diabetes
Research has shown that beta cells can be differentiated from human pancreas progenitor cells. These differentiated beta cells, however, often lack much of the structure and markers that beta cells need to perform their necessary functions. Examples of the anomalies that arise from beta cells differentiated from progenitor cells include a failure to react to environments with high glucose concentrations, an inability to produce necessary beta cell markers, and abnormal expression of glucagon along with insulin. In order to successfully re-create functional insulin producing beta cells, studies have shown that manipulating cell-signal pathways in early stem cell development will lead to those stem cells differentiating into viable beta cells. Two key signal pathways have been shown to play a vital role in the differentiation of stem cells into beta cells: the BMP4 pathway and the kinase C. Targeted manipulation of these two pathways has shown that it is possible to induce beta cell differentiation from stem cells. These variations of artificial beta cells have shown greater levels of success in replicating the functionality of natural beta cells, although the replication has not been perfectly re-created yet. Studies have shown that it is possible to regenerate beta cells ''in vivo'' in some animal models. Research in mice has shown that beta cells can often regenerate to the original quantity number after the beta cells have undergone some sort of stress test, such as the intentional destruction of the beta cells in the mice subject or once the auto-immune response has concluded. While these studies have conclusive results in mice, beta cells in human subjects may not possess this same level of versatility. Investigation of beta cells following acute onset of Type 1 diabetes has shown little to no proliferation of newly synthesized beta cells, suggesting that human beta cells might not be as versatile as rat beta cells, but there is actually no comparison that can be made here because healthy (non-diabetic) rats were used to prove that beta cells can proliferate after intentional destruction of beta cells, while diseased (type-1 diabetic) humans were used in the study which was attempted to use as evidence against beta cells regenerating. It appears that much work has to be done in the field of regenerating beta cells. Just as in the discovery of creating insulin through the use of recombinant DNA, the ability to artificially create stem cells that would differentiate into beta cells would prove to be an invaluable resource to patients with Type 1 diabetes. An unlimited amount of beta cells produced artificially could potentially provide therapy to many of the patients who are affected by Type 1 diabetes.Type 2 diabetes
Research focused on non insulin dependent diabetes encompasses many areas of interest. Degeneration of the beta cell as diabetes progresses has been a broadly reviewed topic. Another topic of interest for beta-cell physiologists is the mechanism of insulin pulsatility which has been well investigated. Many genome studies have been completed and are advancing the knowledge of beta-cell function exponentially. Indeed, the area of beta-cell research is very active yet many mysteries remain.See also
*Gastric inhibitory polypeptide receptor
The gastric inhibitory polypeptide receptor (GIP-R), also known as the glucose-dependent insulinotropic polypeptide receptor, is a protein that in humans is encoded by the ''GIPR'' gene.
GIP-R is a member of the class B family of G protein ...
* List of terms associated with diabetes
* Guangxitoxin
* Alpha cell
Alpha cells (öÝ-cells) are endocrine cells that are found in the Islets of Langerhans in the pancreas. Alpha cells secrete the peptide hormone glucagon in order to increase glucose levels in the blood stream.
Discovery
Islets of Langerhans we ...
* Pancreatic development
The pancreas (plural pancreases, or pancreata) is an organ of the digestive system and endocrine system of vertebrates. In humans, it is located in the abdomen behind the stomach and functions as a gland. The pancreas is a mixed or heterocrine ...
* Islets of Langerhans
The pancreatic islets or islets of Langerhans are the regions of the pancreas that contain its endocrine (hormone-producing) cells, discovered in 1869 by German pathological anatomist Paul Langerhans. The pancreatic islets constitute 1ã2% o ...
* List of distinct cell types in the adult human body
The list of human cell types provides an enumeration and description of the various specialized cells found within the human body, highlighting their distinct functions, characteristics, and contributions to overall physiological processes. Cell ...
* Pancreatic beta cell function
Pancreatic beta cell function (synonyms ''Göý'' or, if calculated from fasting concentrations of insulin and glucose, HOMA-Beta or SPINA-GBeta) is one of the preconditions of euglycaemia, i.e. normal blood sugar regulation. It is defined as insulin ...
References
{{DEFAULTSORT:Beta Cell Endocrine system anatomy Peptide hormone secreting cells