|
Neonatal Red Cell Transfusion
Neonates are defined as babies up to 28 days after birth. Most extremely preterm babies (less than 28 weeks) require at least one red cell transfusion; this is partly due to the amount of blood removed with blood samples compared to the baby's total blood volume (iatrogenic anemia) and partly due to anemia of prematurity. Most transfusions are given as small volume top-up transfusions to increase the baby's hemoglobin above a certain pre-defined level, or because the baby is unwell due to the anemia. Possible side-effects of anemia in babies can be poor growth, lethargy and episodes of apnea. Exchange blood transfusion is used to treat a rapidly rising bilirubin that does not respond to treatment with phototherapy or intravenous immunoglobulin. This is usually due to hemolytic disease of the newborn, but may also be due to other causes, e.g., G6PD deficiency. When to transfuse Below are suggested transfusion thresholds for very preterm neonates (less than 32 weeks gestation) by th ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |
Anemia Of Prematurity
Anemia of prematurity (AOP) refers to a form of anemia affecting preterm infants with decreased hematocrit. AOP is a normochromic, normocytic hypoproliferative anemia. The primary mechanism of AOP is a decrease in erythropoietin (EPO), a red blood cell growth factor. Pathophysiology Preterm infants are often anemic and typically experience heavy blood losses from frequent laboratory testing in the first few weeks of life. Although their anemia is multifactorial, repeated blood sampling and reduced erythropoiesis with extremely low serum levels of erythropoietin (EPO) are major causative factors. Blood sampling done for laboratory testing can easily remove enough blood to produce anemia. Obladen, Sachsenweger and Stahnke (1987) studied 60 very low birth weight infants during the first 28 days of life. Infants were divided into 3 groups, group 1 (no ventilator support, 24 ml/kg blood loss), group 2(minor ventilated support, 60 ml/kg blood loss), and group 3(ventilated support for re ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |
Hyperbilirubinemia
Bilirubin (BR) (Latin for "red bile") is a red-orange compound that occurs in the normal catabolic pathway that breaks down heme in vertebrates. This catabolism is a necessary process in the body's clearance of waste products that arise from the destruction of aged or abnormal red blood cells. In the first step of bilirubin synthesis, the heme molecule is stripped from the hemoglobin molecule. Heme then passes through various processes of porphyrin catabolism, which varies according to the region of the body in which the breakdown occurs. For example, the molecules excreted in the urine differ from those in the feces. The production of biliverdin from heme is the first major step in the catabolic pathway, after which the enzyme biliverdin reductase performs the second step, producing bilirubin from biliverdin.Boron W, Boulpaep E. Medical Physiology: a cellular and molecular approach, 2005. 984–986. Elsevier Saunders, United States. Ultimately, bilirubin is broken down within t ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |
Blood
Blood is a body fluid in the circulatory system of humans and other vertebrates that delivers necessary substances such as nutrients and oxygen to the cells, and transports metabolic waste products away from those same cells. Blood in the circulatory system is also known as ''peripheral blood'', and the blood cells it carries, ''peripheral blood cells''. Blood is composed of blood cells suspended in blood plasma. Plasma, which constitutes 55% of blood fluid, is mostly water (92% by volume), and contains proteins, glucose, mineral ions, hormones, carbon dioxide (plasma being the main medium for excretory product transportation), and blood cells themselves. Albumin is the main protein in plasma, and it functions to regulate the colloidal osmotic pressure of blood. The blood cells are mainly red blood cells (also called RBCs or erythrocytes), white blood cells (also called WBCs or leukocytes) and platelets (also called thrombocytes). The most abundant cells in verte ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |
Transfusion Medicine
Transfusion medicine (or transfusiology) is the branch of medicine that encompasses all aspects of the transfusion of blood and blood components including aspects related to hemovigilance. It includes issues of blood donation, immunohematology and other laboratory testing for transfusion-transmitted diseases, management and monitoring of clinical transfusion practices, patient blood management, therapeutic apheresis, stem cell collections, cellular therapy, and coagulation. Laboratory management and understanding of state and federal regulations related to blood products are also a large part of the field. Overview In most countries, immunohematology and transfusion medicine specialists provide expert opinion on massive transfusions, difficult/incompatible transfusions and rational use of specialised blood product therapy like irradiated blood/ leukodepleted/washed blood products. The blood donor center is the facility that collects blood components from screened blood don ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |
Exchange Transfusion
An exchange transfusion is a blood transfusion in which the patient's blood or components of it are exchanged with (replaced by) other blood or blood products. The patient's blood is removed and replaced by donated blood or blood components. This exchange transfusion can be performed manually or using a machine (apheresis). Most blood transfusions involve adding blood or blood products without removing any blood, these are also known as simple transfusions or top-up transfusions. Exchange transfusion is used in the treatment of a number of diseases, including sickle-cell disease and hemolytic disease of the newborn. Partial exchange might be required for polycythemia. Nearly all exchange transfusions are allogeneic (that is, the new blood or blood products come from another person or persons, via donated blood); autologous exchange transfusion is possible (using autologous blood banking), but there are not many situations in which a need for it arises, as most autologous transfus ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |
Hemolytic Disease Of The Newborn
Hemolytic disease of the newborn, also known as hemolytic disease of the fetus and newborn, HDN, HDFN, or erythroblastosis foetalis, is an alloimmune condition that develops in a fetus at or around birth, when the IgG molecules (one of the five main types of antibodies) produced by the mother pass through the placenta. Among these antibodies are some which attack antigens on the red blood cells in the fetal circulation, breaking down and destroying the cells. The fetus can develop reticulocytosis and anemia. The intensity of this fetal disease ranges from mild to very severe, and fetal death from heart failure ( hydrops fetalis) can occur. When the disease is moderate or severe, many erythroblasts (immature red blood cells) are present in the fetal blood, earning these forms of the disease the name ''erythroblastosis fetalis'' (). HDFN represents a breach of immune privilege for the fetus or some other form of impairment of the immune tolerance in pregnancy. Various typ ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |
Necrotizing Enterocolitis
Necrotizing enterocolitis (NEC) is a devastating intestinal disease that affects premature or very low birth weight infants.Gephart S.M., Quinn M. A call to action to fight for equity and end necrotizing enterocolitis disparities. ''Adv. Neonatal Care.'' 2021;21(5):333-335. doi:10.1097/ANC.0000000000000940 Symptoms may include poor feeding, bloating, decreased activity, blood in the stool, vomiting of bile, bowel death, multiorgan failure, and even death. The exact cause is unclear. However, several risk factors have been identified. Consistently described risk factors include formula feeding, intestinal dysbiosis, low birth weight, and prematurity. Maternal factors such as chorioamnionitis, cocaine abuse, ''in utero'' growth restriction, intrahepatic cholestasis during pregnancy, increased body mass index, lack of prenatal steroids, mode of delivery, placental abruption, preeclampsia, and smoking have not been consistently implicated with the development of NEC. Other risk fact ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |
Serious Hazards Of Transfusion
Serious Hazards of Transfusion (SHOT) is the United Kingdom's haemovigilance scheme. It collects and analyses anonymized information on adverse events and blood transfusion reactions. When SHOT has identified risks related to transfusion, it produces recommendations within its annual reports to improve patient safety. These reports are freely available on its website. SHOT, together with the Medicines and Healthcare products Regulatory Agency (MHRA), works to support haemovigilance reporting in the UK. Results SHOT's statistical data has been used to decrease bacterial infections through better skin cleansing procedures and the incidence of life-threatening transfusion-related acute lung injury (TRALI) in the UK, by discouraging the use of fresh frozen plasma from female donors. The cause of TRALI is not fully understood, and may have more than one mechanism, but most cases are associated with transfusion of plasma or other blood products that contain some antibodies that the ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |
Glucose-6-phosphate Dehydrogenase Deficiency
Glucose-6-phosphate dehydrogenase deficiency (G6PDD), which is the most common enzyme deficiency worldwide, is an inborn error of metabolism that predisposes to red blood cell breakdown. Most of the time, those who are affected have no symptoms. Following a specific trigger, symptoms such as yellowish skin, dark urine, shortness of breath, and feeling tired may develop. Complications can include anemia and newborn jaundice. Some people never have symptoms. It is an X-linked recessive disorder that results in defective glucose-6-phosphate dehydrogenase enzyme. Glucose-6-phosphate dehydrogenase is an enzyme which protects red blood cells, which carry oxygen from the lungs to tissues throughout the body. A defect of the enzyme results in the premature breakdown of red blood cells. This destruction of red blood cells is called hemolysis. Red blood cell breakdown may be triggered by infections, certain medication, stress, or foods such as fava beans. Depending on the specific mutati ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |
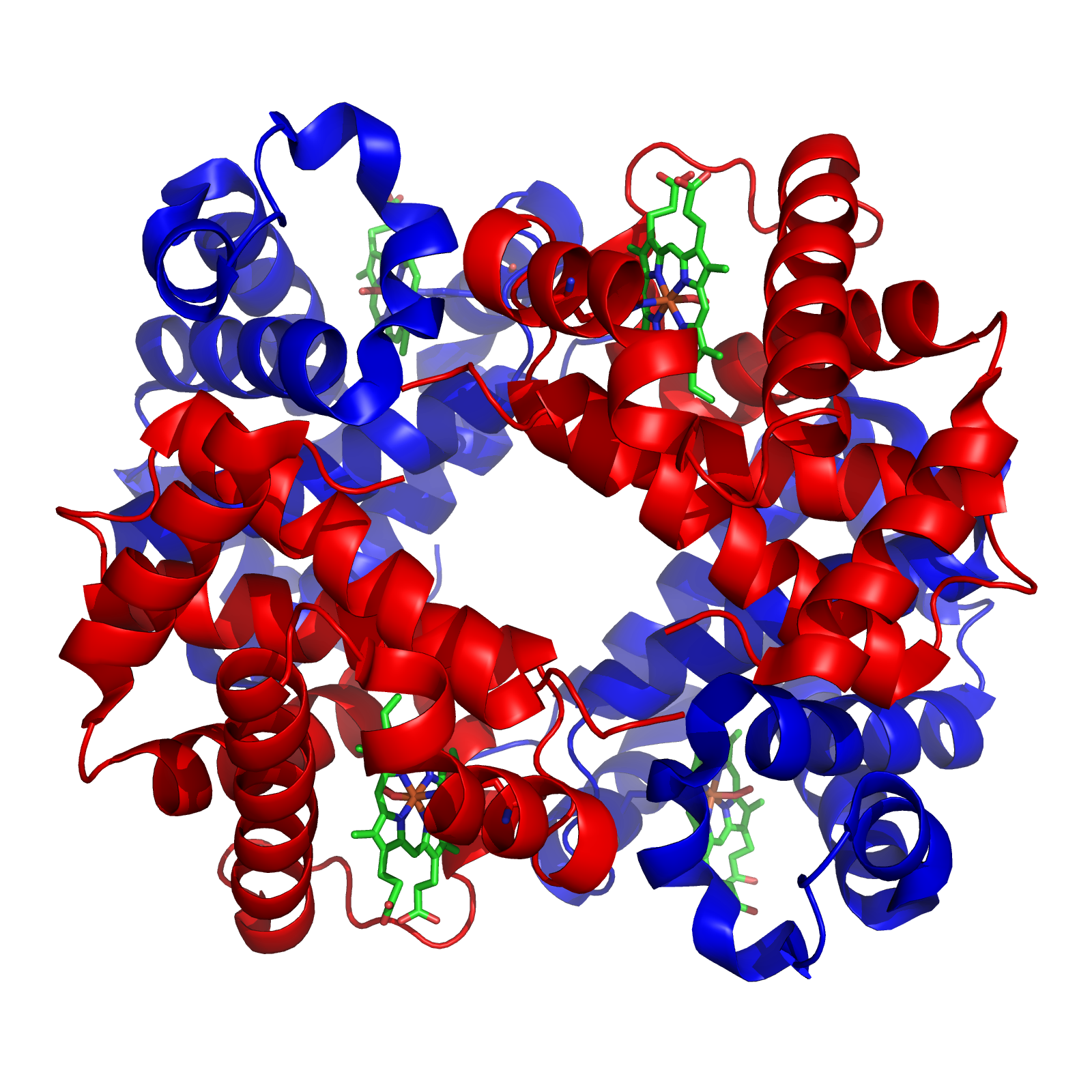
Hemoglobin
Hemoglobin (haemoglobin BrE) (from the Greek word αἷμα, ''haîma'' 'blood' + Latin ''globus'' 'ball, sphere' + ''-in'') (), abbreviated Hb or Hgb, is the iron-containing oxygen-transport metalloprotein present in red blood cells (erythrocytes) of almost all vertebrates (the exception being the fish family Channichthyidae) as well as the tissues of some invertebrates. Hemoglobin in blood carries oxygen from the respiratory organs (''e.g.'' lungs or gills) to the rest of the body (''i.e.'' tissues). There it releases the oxygen to permit aerobic respiration to provide energy to power functions of an organism in the process called metabolism. A healthy individual human has 12to 20grams of hemoglobin in every 100mL of blood. In mammals, the chromoprotein makes up about 96% of the red blood cells' dry content (by weight), and around 35% of the total content (including water). Hemoglobin has an oxygen-binding capacity of 1.34mL O2 per gram, which increases the total blood oxygen ca ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |
Hemolytic Disease Of The Newborn
Hemolytic disease of the newborn, also known as hemolytic disease of the fetus and newborn, HDN, HDFN, or erythroblastosis foetalis, is an alloimmune condition that develops in a fetus at or around birth, when the IgG molecules (one of the five main types of antibodies) produced by the mother pass through the placenta. Among these antibodies are some which attack antigens on the red blood cells in the fetal circulation, breaking down and destroying the cells. The fetus can develop reticulocytosis and anemia. The intensity of this fetal disease ranges from mild to very severe, and fetal death from heart failure ( hydrops fetalis) can occur. When the disease is moderate or severe, many erythroblasts (immature red blood cells) are present in the fetal blood, earning these forms of the disease the name ''erythroblastosis fetalis'' (). HDFN represents a breach of immune privilege for the fetus or some other form of impairment of the immune tolerance in pregnancy. Various typ ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |
Immunoglobulin Therapy
Immunoglobulin therapy is the use of a mixture of antibodies (normal human immunoglobulin or NHIG) to treat several health conditions. These conditions include primary immunodeficiency, immune thrombocytopenic purpura, chronic inflammatory demyelinating polyneuropathy, Kawasaki disease, certain cases of HIV/AIDS and measles, Guillain-Barré syndrome, and certain other infections when a more specific immunoglobulin is not available. Depending on the formulation it can be given by injection into muscle, a vein, or under the skin. The effects last a few weeks. Common side effects include pain at the site of injection, muscle pain, and allergic reactions. Other severe side effects include kidney problems, anaphylaxis, blood clots, and red blood cell breakdown. Use is not recommended in people with some types of IgA deficiency. Use appears to be relatively safe during pregnancy. Human immunoglobulin is made from human blood plasma. It contains antibodies against many viruses. H ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |