parathyroid hormone on:
[Wikipedia]
[Google]
[Amazon]
Parathyroid hormone (PTH), also called parathormone or parathyrin, is a peptide hormone secreted by the parathyroid glands that regulates serum calcium and

 Parathyroid hormone regulates serum calcium through its effects on bone, kidney, and the intestine:
In bone, PTH enhances the release of calcium from the large reservoir contained in the bones. Bone resorption is the normal destruction of bone by osteoclasts, which are indirectly stimulated by PTH. Stimulation is indirect since osteoclasts do not have a receptor for PTH; rather, PTH binds to
Parathyroid hormone regulates serum calcium through its effects on bone, kidney, and the intestine:
In bone, PTH enhances the release of calcium from the large reservoir contained in the bones. Bone resorption is the normal destruction of bone by osteoclasts, which are indirectly stimulated by PTH. Stimulation is indirect since osteoclasts do not have a receptor for PTH; rather, PTH binds to
Parathyroid Hormone (PTH) Plus Calcium
LabCorp. Accessed 2019-07-02.
Parathyroid hormone: analyte monograph
- the Association for Clinical Biochemistry and Laboratory Medicine * {{Authority control Parathyroid hormone receptor agonists Peptide hormones Hormones of the parathyroid glands Hormones of calcium metabolism
phosphate
Phosphates are the naturally occurring form of the element phosphorus.
In chemistry, a phosphate is an anion, salt, functional group or ester derived from a phosphoric acid. It most commonly means orthophosphate, a derivative of orthop ...
through its actions on the bone
A bone is a rigid organ that constitutes part of the skeleton in most vertebrate animals. Bones protect the various other organs of the body, produce red and white blood cells, store minerals, provide structure and support for the body, ...
, kidneys, and small intestine. PTH increases serum calcium levels and is counteracted by calcitonin. Additionally, it promotes the synthesis of calcitriol, the active form of vitamin D.
PTH influences bone remodeling, which is an ongoing process in which bone tissue is alternately resorbed and rebuilt over time. PTH is secreted in response to low blood serum calcium (Ca2+) levels. PTH indirectly stimulates osteoclast activity within the bone matrix ( osteon), in an effort to release more ionic calcium (Ca2+) into the blood to elevate a low serum calcium level. The bone
A bone is a rigid organ that constitutes part of the skeleton in most vertebrate animals. Bones protect the various other organs of the body, produce red and white blood cells, store minerals, provide structure and support for the body, ...
s store calcium from which the body can release into the blood as needed as needed to keep the amount of calcium in the blood at appropriate levels despite the ever-present challenges of metabolism
Metabolism (, from ''metabolē'', "change") is the set of life-sustaining chemical reactions in organisms. The three main functions of metabolism are: the conversion of the energy in food to energy available to run cellular processes; the co ...
, stress, and nutrition
Nutrition is the biochemistry, biochemical and physiology, physiological process by which an organism uses food and water to support its life. The intake of these substances provides organisms with nutrients (divided into Macronutrient, macro- ...
al variations. PTH is the trigger for the bones to release the stored calcium into the blood.
PTH is secreted primarily by the chief cells of the parathyroid glands. The gene for PTH is located on chromosome 11. It is a polypeptide containing 84 amino acids
Amino acids are organic compounds that contain both amino and carboxylic acid functional groups. Although over 500 amino acids exist in nature, by far the most important are the Proteinogenic amino acid, 22 α-amino acids incorporated into p ...
, which is a prohormone. It has a molecular mass around 9500 Da.
There are two types of PTH receptors. Parathyroid hormone 1 receptors, activated by the 34 N-terminal amino acids of PTH, are present at high levels on the cells of bone and kidney. Parathyroid hormone 2 receptors are present at high levels on the cells of central nervous system, pancreas, testes, and placenta. The half-life of PTH is about 4 minutes.
Disorders that yield too little or too much PTH, such as hypoparathyroidism, hyperparathyroidism, and paraneoplastic syndromes can cause bone disease, hypocalcemia, and hypercalcemia.
Structure
hPTH-(1-84) crystallizes as a slightly bent, long, helical dimer. The extended helical conformation of hPTH-(1-84) is the likely bioactive conformation. The N-terminal fragment 1-34 of parathyroid hormone (PTH) has been crystallized and the structure has been refined to 0.9 Å resolution.Function
Regulation of serum calcium
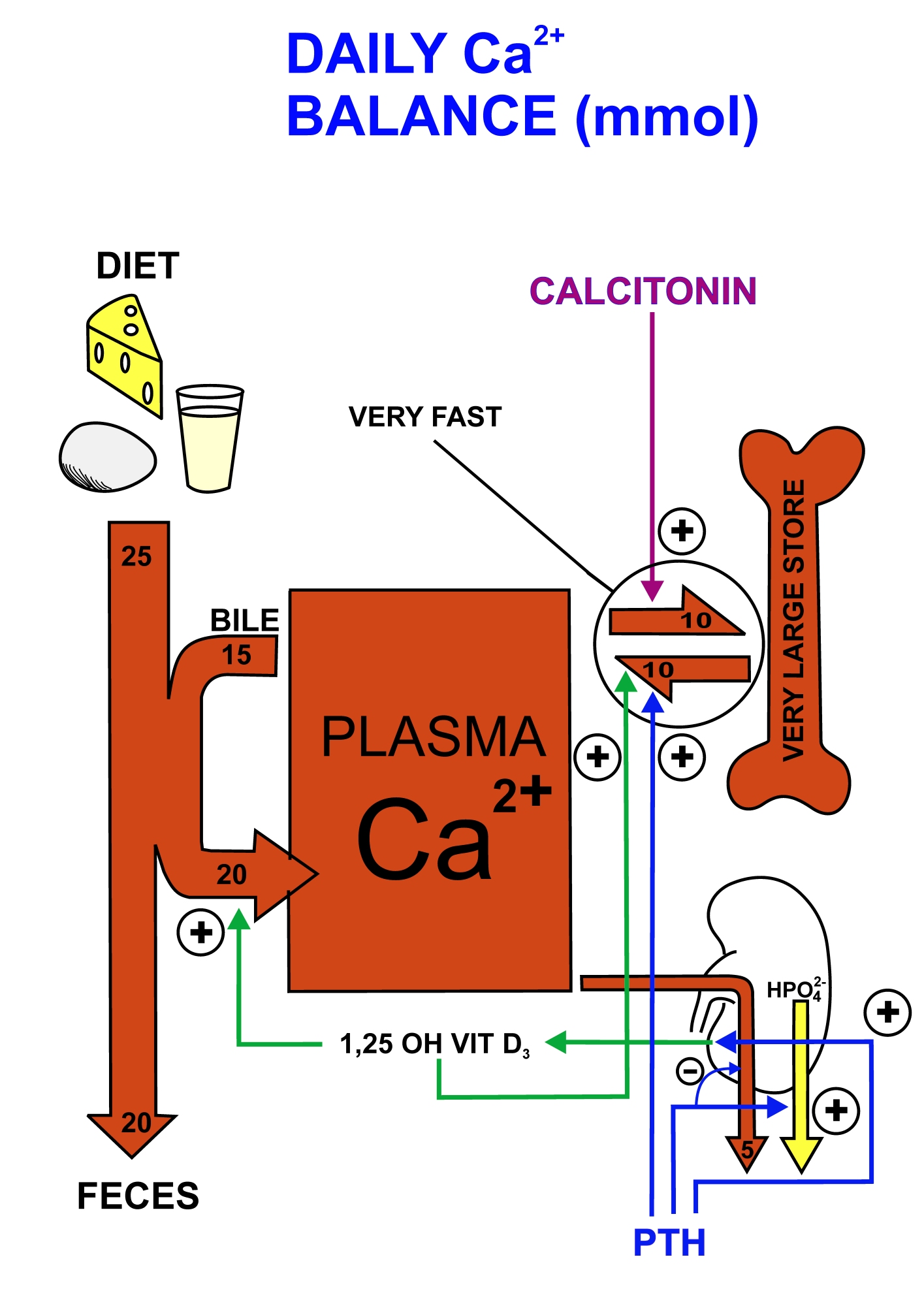
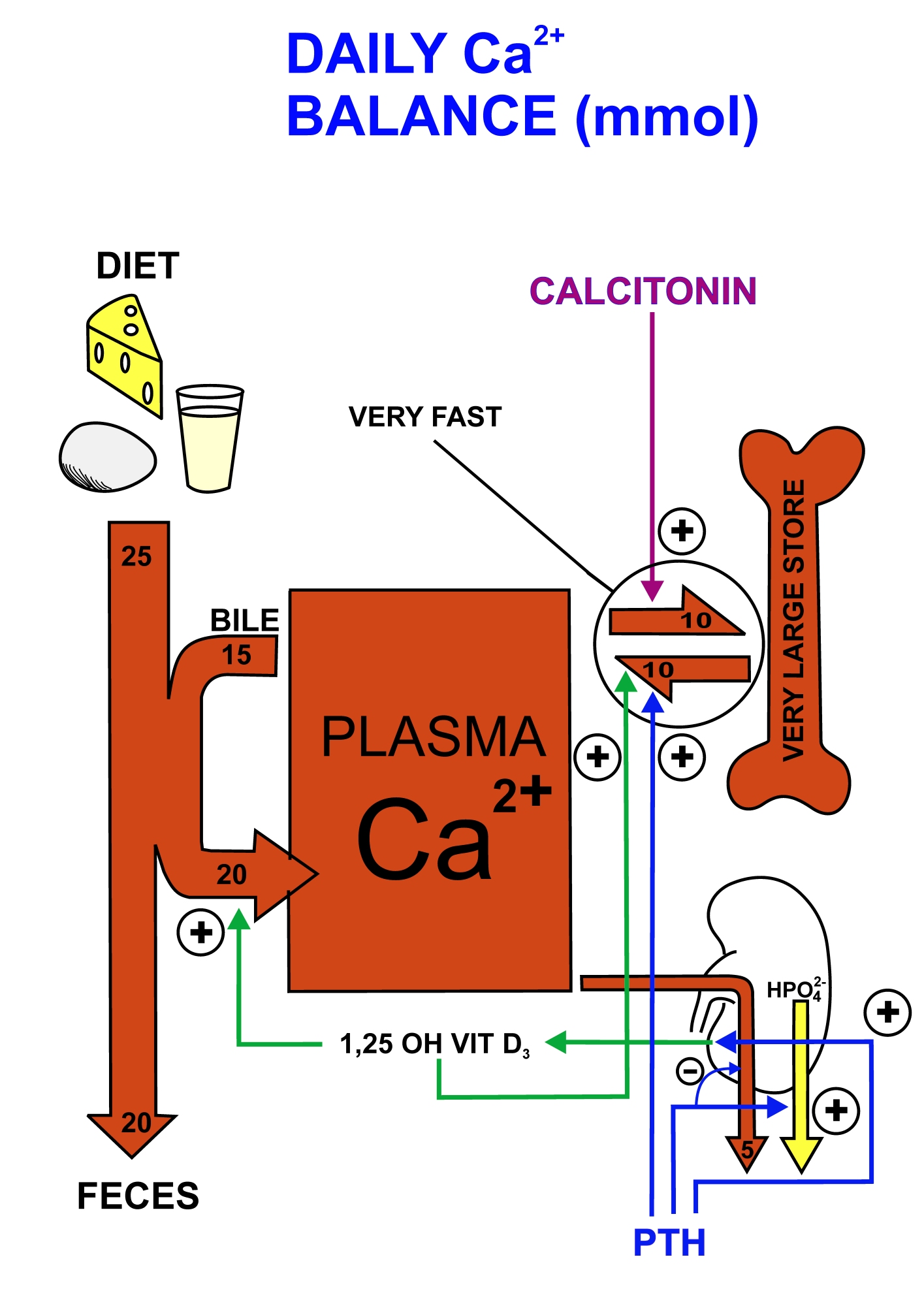 Parathyroid hormone regulates serum calcium through its effects on bone, kidney, and the intestine:
In bone, PTH enhances the release of calcium from the large reservoir contained in the bones. Bone resorption is the normal destruction of bone by osteoclasts, which are indirectly stimulated by PTH. Stimulation is indirect since osteoclasts do not have a receptor for PTH; rather, PTH binds to
Parathyroid hormone regulates serum calcium through its effects on bone, kidney, and the intestine:
In bone, PTH enhances the release of calcium from the large reservoir contained in the bones. Bone resorption is the normal destruction of bone by osteoclasts, which are indirectly stimulated by PTH. Stimulation is indirect since osteoclasts do not have a receptor for PTH; rather, PTH binds to osteoblast
Osteoblasts (from the Greek combining forms for " bone", ὀστέο-, ''osteo-'' and βλαστάνω, ''blastanō'' "germinate") are cells with a single nucleus that synthesize bone. However, in the process of bone formation, osteoblasts fu ...
s, the cells responsible for creating bone. Binding stimulates osteoblasts to increase their expression of RANKL and inhibits their secretion of osteoprotegerin
Osteoprotegerin (OPG), also known as osteoclastogenesis inhibitory factor (OCIF) or tumour necrosis factor receptor superfamily member 11B (TNFRSF11B), is a cytokine receptor of the tumour necrosis factor (TNF) receptor superfamily encoded by th ...
(OPG). Free OPG competitively binds to RANKL as a decoy receptor, preventing RANKL from interacting with RANK, a receptor for RANKL. The binding of RANKL to RANK (facilitated by the decreased amount of OPG available for binding the excess RANKL) stimulates osteoclast precursors, which are of a monocyte lineage, to fuse. The resulting multinucleated cells are osteoclasts, which ultimately mediate bone resorption. Estrogen also regulates this pathway through its effects on PTH. Estrogen suppresses T cell TNF production by regulating T cell differentiation and activity in the bone marrow, thymus, and peripheral lymphoid organs. In the bone marrow, estrogen downregulates the proliferation of hematopoietic stem cells through an IL-7 dependent mechanism.
In the kidney, around 250 mmol of calcium ions are filtered into the glomerular filtrate per day. Most of this (245 mmol/d) is reabsorbed from the tubular fluid, leaving about 5 mmol/d to be excreted in the urine. This reabsorption occurs throughout the tubule (most, 60–70%, of it in the proximal tubule), except in the thin segment of the loop of Henle. Circulating parathyroid hormone only influences the reabsorption that occurs in the distal tubule
The distal convoluted tubule (DCT) is a portion of kidney nephron between the loop of Henle and the collecting tubule.
Physiology
It is partly responsible for the regulation of potassium, sodium, calcium, and pH.
On its Apical membrane, apica ...
s and the renal collecting ducts (but see Footnote). A more important effect of PTH on the kidney is, however, its inhibition of the reabsorption of phosphate
Phosphates are the naturally occurring form of the element phosphorus.
In chemistry, a phosphate is an anion, salt, functional group or ester derived from a phosphoric acid. It most commonly means orthophosphate, a derivative of orthop ...
(HPO42−) from the tubular fluid, resulting in a decrease in the plasma phosphate concentration. Phosphate ions form water-insoluble salts with calcium. Thus, a decrease in the phosphate concentration of the blood plasma (for a given total calcium concentration) increases the amount of calcium that is ionized. A third important effect of PTH on the kidney is its stimulation of the conversion of 25-hydroxy vitamin D into 1,25-dihydroxy vitamin D ( calcitriol), which is released into the circulation. This latter form of vitamin D is the active hormone which stimulates calcium uptake from the intestine.
Via the kidney, PTH enhances the absorption of calcium in the intestine by increasing the production of activated vitamin D. Vitamin D activation occurs in the kidney. PTH up-regulates 25-hydroxyvitamin D3 1-alpha-hydroxylase, the enzyme responsible for 1-alpha hydroxylation of 25-hydroxy vitamin D, converting vitamin D to its active form (1,25-dihydroxy vitamin D). This activated form of vitamin D increases the absorption of calcium (as Ca2+ ions) by the intestine via calbindin.
PTH was one of the first hormones to be shown to use the G-protein adenylyl cyclase second messenger system.
Regulation of serum phosphate
PTH reduces the reabsorption ofphosphate
Phosphates are the naturally occurring form of the element phosphorus.
In chemistry, a phosphate is an anion, salt, functional group or ester derived from a phosphoric acid. It most commonly means orthophosphate, a derivative of orthop ...
from the proximal tubule of the kidney, which means more phosphate is excreted through the urine.
However, PTH enhances the uptake of phosphate from the intestine and bones into the blood. In the bone, slightly more calcium than phosphate is released from the breakdown of bone. In the intestines, absorption of both calcium and phosphate is mediated by an increase in activated vitamin D. The absorption of phosphate is not as dependent on vitamin D as is that of calcium. The result of PTH release is a small net drop in the serum concentration of phosphate.
Vitamin D synthesis
PTH upregulates the activity of 1-α-hydroxylase enzyme, which converts 25-hydroxycholecalciferol, the major circulating form of inactive vitamin D, into 1,25-dihydroxycholecalciferol, the active form of vitamin D, in the kidney.Interactive pathway map
Regulation of PTH secretion
Secretion of parathyroid hormone is determined chiefly by serum ionized calcium concentration throughnegative feedback
Negative feedback (or balancing feedback) occurs when some function (Mathematics), function of the output of a system, process, or mechanism is feedback, fed back in a manner that tends to reduce the fluctuations in the output, whether caused ...
. Parathyroid cells express calcium-sensing receptors on the cell surface. PTH is secreted when a2+is decreased (calcitonin is secreted when serum calcium levels are elevated). The G-protein-coupled calcium receptors bind extracellular calcium and may be found on the surface on a wide variety of cells distributed in the brain
The brain is an organ (biology), organ that serves as the center of the nervous system in all vertebrate and most invertebrate animals. It consists of nervous tissue and is typically located in the head (cephalization), usually near organs for ...
, heart
The heart is a muscular Organ (biology), organ found in humans and other animals. This organ pumps blood through the blood vessels. The heart and blood vessels together make the circulatory system. The pumped blood carries oxygen and nutrie ...
, skin, stomach, C cells, and other tissues. In the parathyroid gland, high concentrations of extracellular calcium result in activation of the Gq G-protein coupled cascade through the action of phospholipase C. This hydrolyzes phosphatidylinositol 4,5-bisphosphate (PIP2) to liberate intracellular messengers IP3 and diacylglycerol (DAG). Ultimately, these two messengers result in a release of calcium from intracellular stores into the cytoplasmic space. Hence a high extracellular calcium concentration leads to an increase in the cytoplasmic calcium concentration. In contrast to the mechanism that most secretory cells use, this high cytoplasmic calcium concentration inhibits the fusion of vesicles containing granules of preformed PTH with the membrane of the parathyroid cell, and thus inhibits release of PTH.
In the parathyroids, magnesium serves this role in stimulus-secretion coupling. A mild decrease in serum magnesium levels stimulates the reabsorptive activity PTH has on the kidneys. Severe hypomagnesemia inhibits PTH secretion and also causes resistance to PTH, leading to a form of hypoparathyroidism that is reversible.
Stimulators
* Decreased serum a2+ * Mild decreases in serum g2+ * An increase in serum phosphate (increased phosphate causes it to complex with serum calcium, forming calcium phosphate, which reduces stimulation of Ca-sensitive receptors (CaSr) that do not sense calcium phosphate, triggering an increase in PTH). * Adrenaline * HistamineInhibitors
* Increased serum a2+ * Severe decreases in serum g2+ which also produces symptoms of hypoparathyroidism (such as hypocalcemia). * Calcitriol *Increase in serum phosphate. Fibroblast growth factor-23 (FGF23) is produced in osteoblasts (from bone) in response to increases in serum phosphate (Pi). It binds to the fibroblast growth factor receptor of the parathyroid and suppresses PTH release. This may seem contradictory because PTH actually helps rid the blood of phosphates but it is also causes release of phosphate into the blood from bone resorption. FGF23 inhibits PTH and then takes its place helping inhibit re-absorption of phosphate in the kidney without the phosphate releasing effect on bones.Disorders
Hyperparathyroidism, the presence of excessive amounts of parathyroid hormone in the blood, occurs in two very distinct sets of circumstances. Primary hyperparathyroidism is due to autonomous, abnormal hypersecretion of PTH from the parathyroid gland, while secondary hyperparathyroidism is an appropriately high PTH level seen as a physiological response to hypocalcemia. A low level of PTH in the blood is known as hypoparathyroidism and is most commonly due to damage to or removal of parathyroid glands during thyroid surgery. There are a number of rare but well-described genetic conditions affecting parathyroid hormone metabolism, including pseudohypoparathyroidism, familial hypocalciuric hypercalcemia, and autosomal dominant hypercalciuric hypocalcemia. Of note, PTH is unchanged in pseudopseudohypoparathyroidism. In osteoporotic women, administration of an exogenous parathyroid hormone analogue ( teriparatide, by daily injection) superimposed on estrogen therapy produced increases in bone mass and reduced vertebral and nonvertebral fractures by 45–65%.Measurement
PTH can be measured in the blood in several different forms: intact PTH; N-terminal PTH; mid-molecule PTH, and C-terminal PTH, and different tests are used in different clinical situations. The level may be stated in pg/dL or pmol/L (sometimes abbreviated mmol/L); multiply by 0.1060 to convert from pg/dL to pmol/L. A US source states the average PTH level to be 8–51 pg/mL. In the UK the biological reference range is considered to be 1.6–6.9 pmol/L. Normal total plasma calcium level ranges from 8.5 to 10.2 mg/dL (2.12 mmol/L to 2.55 mmol/L).Interpretive guide
The intact PTH and calcium normal ranges are different for age; calcium is also different for sex.LabCorp. Accessed 2019-07-02.
Medical uses
Recombinant human parathyroid hormone
Teriparatide
See also
* Disorders of calcium metabolism * Parathyroid hormone family * Parathyroid hormone-related proteinFootnote
References
Further reading
* * * * * * * * * * * * * * * * * * * *External links
*Parathyroid hormone: analyte monograph
- the Association for Clinical Biochemistry and Laboratory Medicine * {{Authority control Parathyroid hormone receptor agonists Peptide hormones Hormones of the parathyroid glands Hormones of calcium metabolism