local anesthetic nerve block on:
[Wikipedia]
[Google]
[Amazon]
Nerve block or regional nerve blockade is any deliberate interruption of signals traveling along a nerve, often for the purpose of
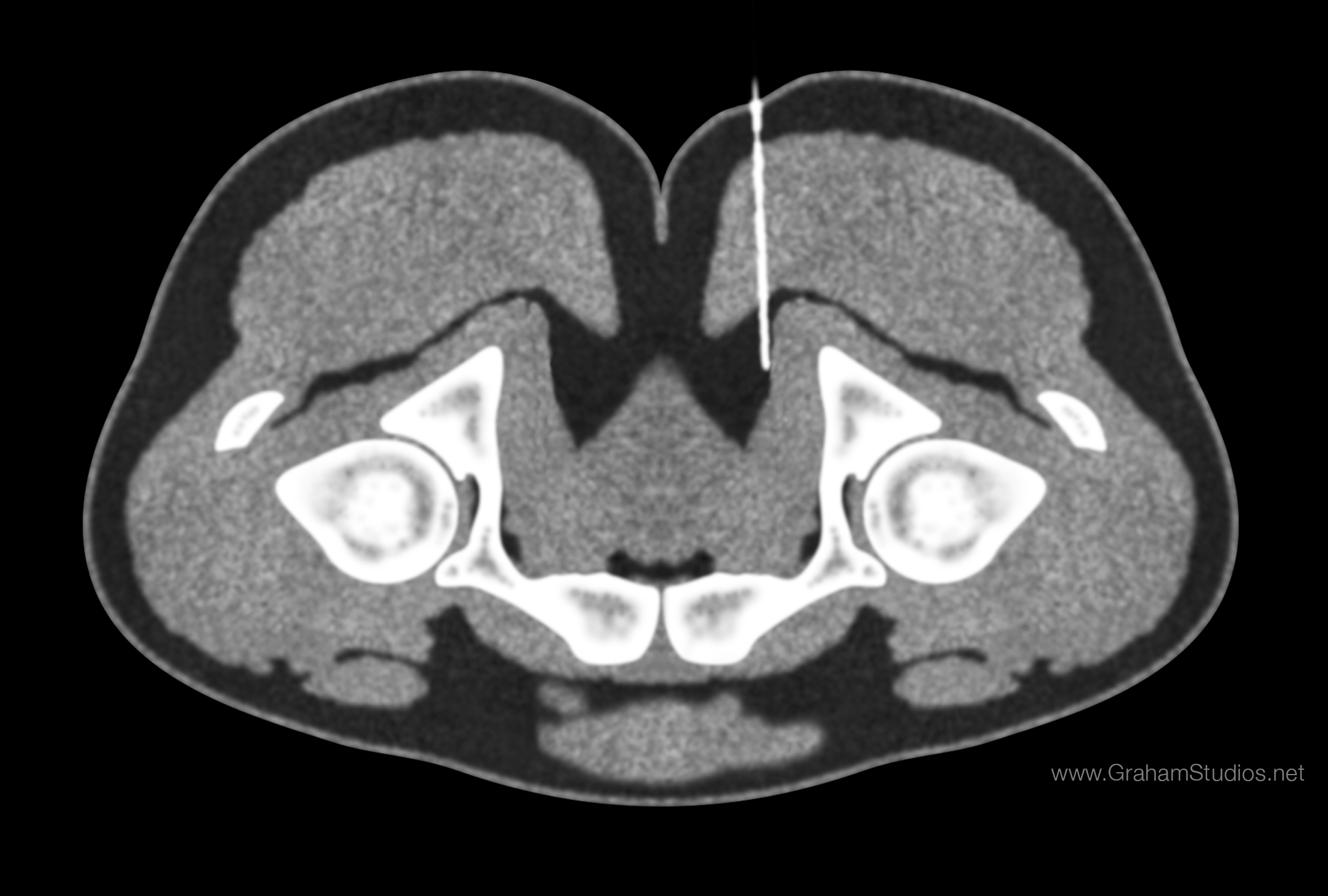 The use of CT guidance is largely predicated on the limitations of lower cost image-guided injections such as fluoroscopy and ultrasound, as well as the cost considerations and availability of more precise imaging such as MRI-guidance.
CT provides excellent spatial resolution and good soft-tissue contrast. This makes it easy to verify the anatomic level. While the use of CT does expose the patient to radiation, the amount of radiation is less than a full scan. For example, the radiation from a lumbar spine CT is approximately 7.5 mSv, but the radiation from standard protocols for CT-guided epidurals is about 1.3-1.5 mSv. A low-dose CT protocol may still provide the required resolution, and if used can reduce the radiation exposure by another 85%, bringing the radiation exposure to about 0.2 mSv.
The machine cost of CT is a barrier to availability and more widespread use, though still more cost-effective than an MRI. CT machine costs can range from $415,000 to $615,000 USD.
The use of CT guidance is largely predicated on the limitations of lower cost image-guided injections such as fluoroscopy and ultrasound, as well as the cost considerations and availability of more precise imaging such as MRI-guidance.
CT provides excellent spatial resolution and good soft-tissue contrast. This makes it easy to verify the anatomic level. While the use of CT does expose the patient to radiation, the amount of radiation is less than a full scan. For example, the radiation from a lumbar spine CT is approximately 7.5 mSv, but the radiation from standard protocols for CT-guided epidurals is about 1.3-1.5 mSv. A low-dose CT protocol may still provide the required resolution, and if used can reduce the radiation exposure by another 85%, bringing the radiation exposure to about 0.2 mSv.
The machine cost of CT is a barrier to availability and more widespread use, though still more cost-effective than an MRI. CT machine costs can range from $415,000 to $615,000 USD.
 Local anesthetics are broken down into two categories: ester-linked and amide-linked. The esters include
Local anesthetics are broken down into two categories: ester-linked and amide-linked. The esters include
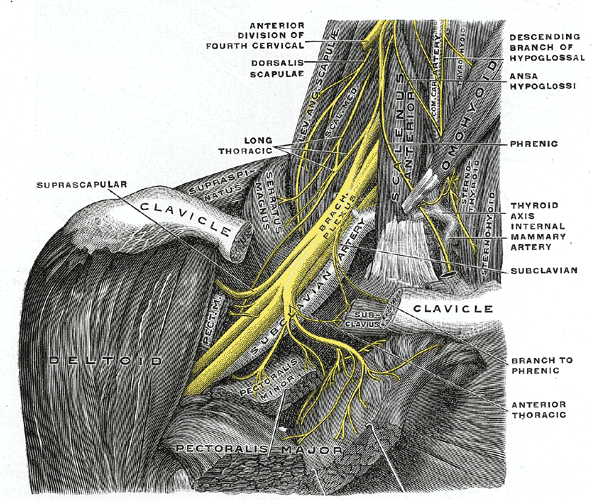 The brachial plexus is a bundle of nerves innervating the shoulder and arm and can be blocked at different levels depending on the type of upper extremity surgery being performed. Interscalene brachial plexus blocks can be done before shoulder, arm, and elbow surgery. The interscalene block is done at the neck where the brachial plexus emerges between the anterior and middle scalene muscles. Lidocaine is injected first to numb the skin and then a blunt needle is used to protect the nerves from damage as the physician places the needle very close to the nerves. The needle goes in about 3–4 cm and a single shot of local anesthetic is injected or a catheter is placed. The most common local anesthetics used at the site of the nerves are bupivicaine, mepivicaine, and chloroprocaine. There is a very high chance that the
The brachial plexus is a bundle of nerves innervating the shoulder and arm and can be blocked at different levels depending on the type of upper extremity surgery being performed. Interscalene brachial plexus blocks can be done before shoulder, arm, and elbow surgery. The interscalene block is done at the neck where the brachial plexus emerges between the anterior and middle scalene muscles. Lidocaine is injected first to numb the skin and then a blunt needle is used to protect the nerves from damage as the physician places the needle very close to the nerves. The needle goes in about 3–4 cm and a single shot of local anesthetic is injected or a catheter is placed. The most common local anesthetics used at the site of the nerves are bupivicaine, mepivicaine, and chloroprocaine. There is a very high chance that the
 Fascia iliaca block is indicated for pain relief for hip fractures in adults and femoral fractures in children. It works by affecting the femoral, obturator and the lateral cutaneous nerves.
3-in-1 nerve block is indicated for pain relief for hip fractures.
The
Fascia iliaca block is indicated for pain relief for hip fractures in adults and femoral fractures in children. It works by affecting the femoral, obturator and the lateral cutaneous nerves.
3-in-1 nerve block is indicated for pain relief for hip fractures.
The
pain relief
Pain management is an aspect of medicine and health care involving relief of pain (pain relief, analgesia, pain control) in various dimensions, from acute and simple to chronic and challenging. Most physicians and other health professionals ...
. Local anesthetic nerve block (sometimes referred to as simply "nerve block") is a short-term block, usually lasting hours or days, involving the injection of an anesthetic, a corticosteroid
Corticosteroids are a class of steroid hormones that are produced in the adrenal cortex of vertebrates, as well as the synthetic analogues of these hormones. Two main classes of corticosteroids, glucocorticoids and mineralocorticoids, are invo ...
, and other agents onto or near a nerve. Neurolytic block, the deliberate temporary degeneration of nerve fibers through the application of chemicals, heat, or freezing, produces a block that may persist for weeks, months, or indefinitely. Neurectomy, the cutting through or removal of a nerve or a section of a nerve, usually produces a permanent block. Because neurectomy of a sensory nerve
A sensory nerve, or afferent nerve, is a nerve that contains exclusively afferent nerve fibers. Nerves containing also motor fibers are called mixed nerve, mixed. Afferent nerve fibers in a sensory nerve carry sensory system, sensory information ...
is often followed, months later, by the emergence of new, more intense pain, sensory nerve neurectomy is rarely performed.
The concept of nerve block sometimes includes ''central nerve block'', which includes epidural
Epidural administration (from Ancient Greek ἐπί, "upon" + '' dura mater'') is a method of medication administration in which a medicine is injected into the epidural space around the spinal cord. The epidural route is used by physicians ...
and spinal anaesthesia
Spinal anaesthesia (or spinal anesthesia), also called spinal block, subarachnoid block, intradural block and intrathecal block, is a form of neuraxial regional anaesthesia involving the injection of a local anaesthetic with or without an opi ...
.
Local anesthetic nerve block
Local anesthetic nerve block (local anesthetic regional nerve blockade, or often simply nerve block) is a short-term nerve block involving theinjection
Injection or injected may refer to:
Science and technology
* Injective function, a mathematical function mapping distinct arguments to distinct values
* Injection (medicine), insertion of liquid into the body with a syringe
* Injection, in broadca ...
of local anesthetic
A local anesthetic (LA) is a medication that causes absence of all sensation (including pain) in a specific body part without loss of consciousness, providing local anesthesia, as opposed to a general anesthetic, which eliminates all sensati ...
as close to the nerve
A nerve is an enclosed, cable-like bundle of nerve fibers (called axons). Nerves have historically been considered the basic units of the peripheral nervous system. A nerve provides a common pathway for the Electrochemistry, electrochemical nerv ...
as possible for pain relief
Pain management is an aspect of medicine and health care involving relief of pain (pain relief, analgesia, pain control) in various dimensions, from acute and simple to chronic and challenging. Most physicians and other health professionals ...
. The local anesthetic bathes the nerve and numbs the area of the body that is supplied by that nerve. The goal of the nerve block is to prevent pain by blocking the transmission of pain signals from the affected area. Local anesthetic is often combined with other drugs to potentiate or prolong the analgesia produced by the nerve block. These adjuvants may include epinephrine
Adrenaline, also known as epinephrine, is a hormone and medication which is involved in regulating visceral functions (e.g., respiration). It appears as a white microcrystalline granule. Adrenaline is normally produced by the adrenal glands a ...
(or more specific alpha-adrenergic agonists), corticosteroids
Corticosteroids are a class of steroid hormones that are produced in the adrenal cortex of vertebrates, as well as the synthetic analogues of these hormones. Two main classes of corticosteroids, glucocorticoids and mineralocorticoids, are invol ...
, opioids
Opioids are a class of Drug, drugs that derive from, or mimic, natural substances found in the Papaver somniferum, opium poppy plant. Opioids work on opioid receptors in the brain and other organs to produce a variety of morphine-like effects, ...
, or ketamine
Ketamine is a cyclohexanone-derived general anesthetic and NMDA receptor antagonist with analgesic and hallucinogenic properties, used medically for anesthesia, depression, and pain management. Ketamine exists as its S- (esketamine) a ...
. These blocks can be either single treatments, multiple injections over a period of time, or continuous infusions. A continuous peripheral nerve block can be introduced into a limb undergoing surgery – for example, a femoral nerve block
A femoral nerve block is a nerve block that uses local anesthetic to achieve analgesia in the leg. The block works by affecting the femoral nerve.
A femoral nerve block (FNB) results in anesthesia of the skin and muscles of the anterior thigh and ...
to prevent pain in knee replacement
Knee replacement, also known as knee arthroplasty, is a surgical procedure to replace the weight-bearing surfaces of the knee joint to relieve pain and disability, most commonly offered when joint pain is not diminished by conservative sources. ...
.
Uses
Regional analgesia
Regional blocks can be used for procedural anesthesia, post-operative analgesia, and treatment of acute pain in the emergency room. Consequently they can be an alternative to general anesthesia as well as oral pain medications. An advantage over oral pain medications is that regional blocks can provide complete relief of pain along a nerve distribution. This can lead to a reduction in the amount ofopiates
An opiate is an alkaloid substance derived from opium (or poppy straw). It differs from the similar term ''opioid'' in that the latter is used to designate all substances, both natural and synthetic, that bind to opioid receptors in the brain ( ...
needed. Advantages over general anesthesia include faster recovery and less need for monitoring.
Diagnostic blocks
Nerve blocks can be used for the diagnosis of surgically treatable chronic pain, such asnerve compression syndrome
Nerve compression syndrome, or compression neuropathy, or nerve entrapment syndrome, is a medical condition caused by chronic, direct pressure on a peripheral nerve. It is known colloquially as a ''trapped nerve'', though this may also refer to ...
. Advances in surgical techniques such as minimally invasive surgery have made virtually all peripheral nerves surgically accessible since the invention of open surgery. Any nerve that can be blocked can now be treated with a nerve decompression
A nerve decompression is a neurosurgical procedure to relieve chronic, direct pressure on a nerve to treat nerve entrapment, a pain syndrome characterized by severe chronic pain and muscle weakness. In this way a nerve decompression targets the ...
. Imaging such as MRI has poor correlation with clinical diagnosis of nerve entrapment as well as intraoperative findings of decompression surgeries and so diagnostic blocks are used for surgical planning.
Technique
Local anesthetic nerve blocks are sterile procedures usually performed in anoutpatient
A patient is any recipient of health care services that are performed by healthcare professionals. The patient is most often ill or injured and in need of treatment by a physician, nurse, optometrist, dentist, veterinarian, or other healt ...
facility or hospital. The procedure can be performed with the help of ultrasound
Ultrasound is sound with frequency, frequencies greater than 20 Hertz, kilohertz. This frequency is the approximate upper audible hearing range, limit of human hearing in healthy young adults. The physical principles of acoustic waves apply ...
, fluoroscopy
Fluoroscopy (), informally referred to as "fluoro", is an imaging technique that uses X-rays to obtain real-time moving images of the interior of an object. In its primary application of medical imaging, a fluoroscope () allows a surgeon to see t ...
, CT, or MRI
Magnetic resonance imaging (MRI) is a medical imaging technique used in radiology to generate pictures of the anatomy and the physiological processes inside the body. MRI scanners use strong magnetic fields, magnetic field gradients, and rad ...
/ MRN to guide the practitioner in the placement of the needle. The various imaging modalities differ in their availability, cost, spatial resolution, soft tissue resolution, bone resolution, radiation exposure, accuracy, real-time imaging capabilities, and ability to visualize small or deep nerves.
Landmark-guided peripheral nerve block
Landmark-guided (or "blind") nerve blocks use palpable anatomical landmarks and a working knowledge of the superficial and deep anatomy to determine where to place the needle. Although a peripheral nerve stimulator can be used to facilitate placement of the block, it is designed to elicit a motor response rather than creating aparesthesia
Paresthesia is a sensation of the skin that may feel like numbness (''hypoesthesia''), tingling, pricking, chilling, or burning. It can be temporary or Chronic condition, chronic and has many possible underlying causes. Paresthesia is usually p ...
, making it less effective for identifying purely sensory nerves. Landmark-guided injections have largely been replaced with image guidance due to increased accuracy, but there are some nerves for which landmark-guidance still has comparable accuracy, such as the pudendal nerve.
Fluoroscopy-guided peripheral nerve block
Fluoroscopy
Fluoroscopy (), informally referred to as "fluoro", is an imaging technique that uses X-rays to obtain real-time moving images of the interior of an object. In its primary application of medical imaging, a fluoroscope () allows a surgeon to see t ...
is an imaging technique that uses X-rays to obtain real-time moving planar images of the interior of an object. In this sense, fluoroscopy is a continuous x-ray. Fluoroscopy is broadly similar to landmark-guided injections except that the landmarks are based on radiographic anatomy. However, there is poor soft tissue contrast, meaning that nerves cannot be clearly visualized. Nerves that are situated by bony landmarks can be good candidates, such as epidural steroid injections, which target the spinal nerves.
The radiation involved is higher than an x-ray, but lower than a CT-guided injection (which is itself lower than a full CT scan). One study found about 0.40 mSv exposure per minute of fluoroscopy for up to 3 minutes and another found that 3711 epidural injections took a maximum of 47 seconds.
Ultrasound-guided peripheral nerve block
Ultrasound
Ultrasound is sound with frequency, frequencies greater than 20 Hertz, kilohertz. This frequency is the approximate upper audible hearing range, limit of human hearing in healthy young adults. The physical principles of acoustic waves apply ...
-guided peripheral nerve block is a procedure that allows real-time
Real-time, realtime, or real time may refer to:
Computing
* Real-time computing, hardware and software systems subject to a specified time constraint
* Real-time clock, a computer clock that keeps track of the current time
* Real-time Control Syst ...
imaging
Imaging is the representation or reproduction of an object's form; especially a visual representation (i.e., the formation of an image).
Imaging technology is the application of materials and methods to create, preserve, or duplicate images.
...
of the positions of the targeted nerve
A nerve is an enclosed, cable-like bundle of nerve fibers (called axons). Nerves have historically been considered the basic units of the peripheral nervous system. A nerve provides a common pathway for the Electrochemistry, electrochemical nerv ...
, needle, and surrounding vasculature
In vertebrates, the circulatory system is a system of organs that includes the heart, blood vessels, and blood which is circulated throughout the body. It includes the cardiovascular system, or vascular system, that consists of the heart an ...
and other anatomical structures. This visual aid increases the success rate of the block and may reduce the risk of complications. It may also reduce the amount of local anesthetic
A local anesthetic (LA) is a medication that causes absence of all sensation (including pain) in a specific body part without loss of consciousness, providing local anesthesia, as opposed to a general anesthetic, which eliminates all sensati ...
required, while reducing the onset time of blocks. Ultrasound has also resulted in an exponential rise in fascial plane blocks. Ultrasound is particularly well-suited for regional anesthesia, since many of the anesthesia targets (e.g., brachial plexus, femoral nerve) have large blood vessels that travel with the target nerves. Direct visualization of nerves is not just important for localization, but also to ensure that the injected material surrounds the nerve. Likewise, visualization of blood vessels is important to ensure that needle placement avoids blood vessels, which often travel directly parallel to nerves.
Ultrasound machine is generally portable and inexpensive in comparison to the CT scanner, fluoroscopic machine, and MRI scanner. The relatively low cost of an ultrasound machine compared to other imaging machines allows for its widespread availability.
Ultrasound has a few limitations. First an acoustic window is required, and certain tissue types such as bone can interfere with image acquisition. Next hand-operated probe can make the images challenging for surgical planning when the exact needle location must be known. CT and MRI have standard slicing orientations (sagittal, coronal, axial), but for ultrasound the orientation of the 2D image depends on the position and orientation of a probe held by the operator. Lastly ultrasound has a tradeoff between penetration depth and resolution. Higher frequencies provide better resolution but have less penetration depth. You may be able to acquire good resolution at shallow depths or see deep structures only with poor resolution. The limited penetration depth and resolution tends to make ultrasound a poor choice in particular for deeply situated pelvic nerves.
CT-guided peripheral nerve block
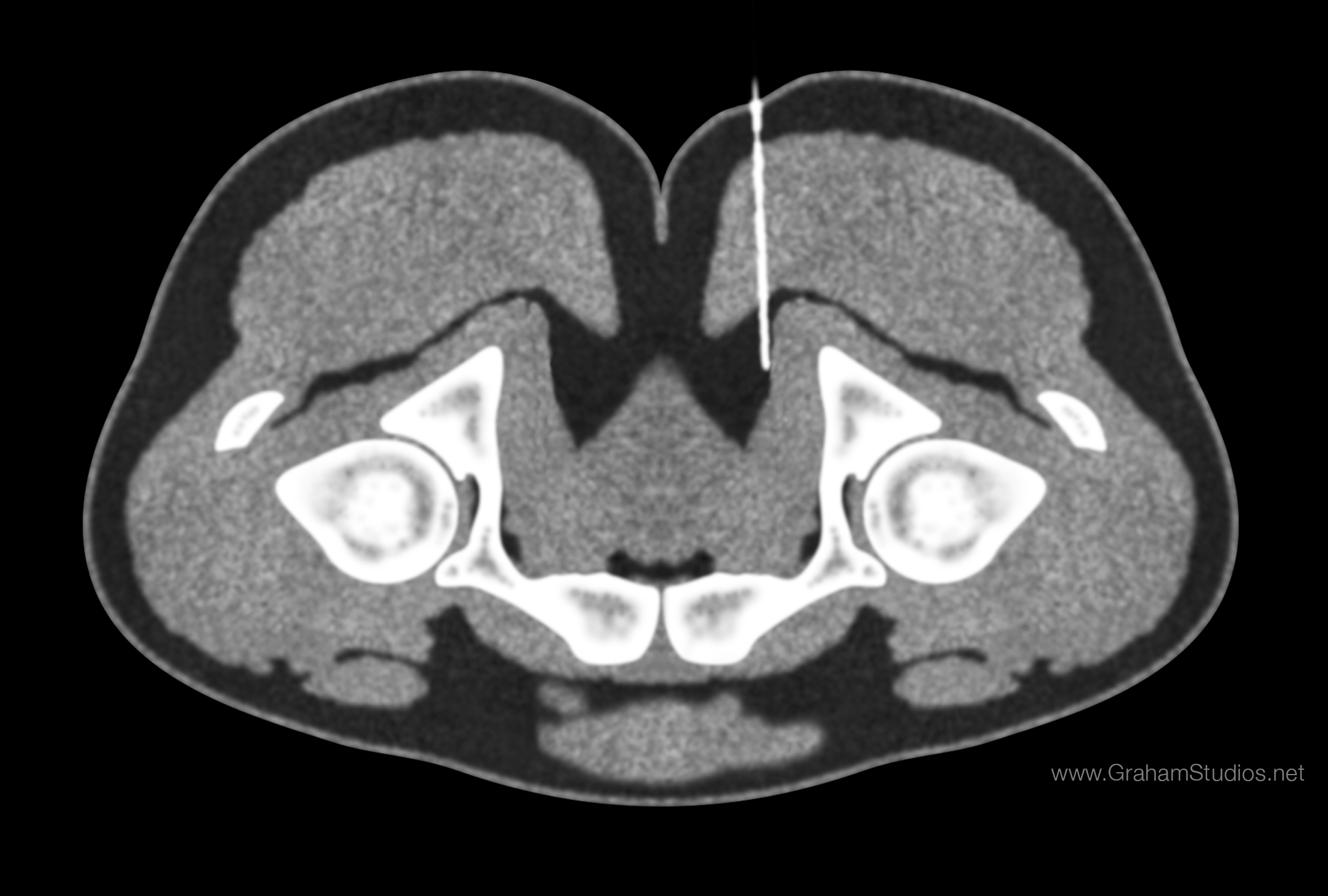 The use of CT guidance is largely predicated on the limitations of lower cost image-guided injections such as fluoroscopy and ultrasound, as well as the cost considerations and availability of more precise imaging such as MRI-guidance.
CT provides excellent spatial resolution and good soft-tissue contrast. This makes it easy to verify the anatomic level. While the use of CT does expose the patient to radiation, the amount of radiation is less than a full scan. For example, the radiation from a lumbar spine CT is approximately 7.5 mSv, but the radiation from standard protocols for CT-guided epidurals is about 1.3-1.5 mSv. A low-dose CT protocol may still provide the required resolution, and if used can reduce the radiation exposure by another 85%, bringing the radiation exposure to about 0.2 mSv.
The machine cost of CT is a barrier to availability and more widespread use, though still more cost-effective than an MRI. CT machine costs can range from $415,000 to $615,000 USD.
The use of CT guidance is largely predicated on the limitations of lower cost image-guided injections such as fluoroscopy and ultrasound, as well as the cost considerations and availability of more precise imaging such as MRI-guidance.
CT provides excellent spatial resolution and good soft-tissue contrast. This makes it easy to verify the anatomic level. While the use of CT does expose the patient to radiation, the amount of radiation is less than a full scan. For example, the radiation from a lumbar spine CT is approximately 7.5 mSv, but the radiation from standard protocols for CT-guided epidurals is about 1.3-1.5 mSv. A low-dose CT protocol may still provide the required resolution, and if used can reduce the radiation exposure by another 85%, bringing the radiation exposure to about 0.2 mSv.
The machine cost of CT is a barrier to availability and more widespread use, though still more cost-effective than an MRI. CT machine costs can range from $415,000 to $615,000 USD.
MRI-guided peripheral nerve block
MRI
Magnetic resonance imaging (MRI) is a medical imaging technique used in radiology to generate pictures of the anatomy and the physiological processes inside the body. MRI scanners use strong magnetic fields, magnetic field gradients, and rad ...
provides excellent visualization of soft tissues, but the detail is not usually enough to see the small nerves that are often entrapped. Newer technology ( MR neurography), however, has increased the level of nerve details seen and allowed for more accurate MRI-directed injections. The ability to visualize nerves is important for localization and also for ensuring that injected material properly surrounds the nerve. The good soft tissue contrast also makes it easier to avoid injuring other tissue structures such as blood vessels and in the case of pelvic injections, the large intestines.
MRN-guided blocks are especially effective for deep, small nerves which are otherwise difficult to visualize with ultrasound and CT. The use of radiation-free MRI complies with ALARP (As Low As Reasonably Practical) practice mandate and can be a better choice for radiation-sensitive patients such as children and pregnant women. However, due to the expense of MRI machines, MRN-guidance is not a substitute for other imaging modalities but rather a specialized tool which higher accuracy is required. The cost of an MRI machine limits more widespread use and is significant, at about $1,000,000 USD per Tesla. Often a 1.5T machine with a wide bore will be used, but a 3T machine should provide the highest resolution.
Common local anesthetics
benzocaine
Benzocaine, sold under the brand name Orajel amongst others, is a local anesthetic, belonging to the amino ester drug class, commonly used as a topical painkiller or in cough drops. It is the active ingredient in many over-the-counter ...
, procaine
Procaine is a local anesthetic drug of the amino ester group. It is most commonly used in dental procedures to numb the area around a tooth and is also used to reduce the pain of intramuscular injection of penicillin. Owing to the ubiquity of ...
, tetracaine
Tetracaine, also known as amethocaine, is an ester local anesthetic used to numb the eyes, nose, or throat. It may also be applied to the skin before starting intravenous therapy to decrease pain from the procedure. Typically it is applied as a l ...
, and chloroprocaine. The amides include lidocaine
Lidocaine, also known as lignocaine and sold under the brand name Xylocaine among others, is a local anesthetic of the amino amide type. It is also used to treat ventricular tachycardia and ventricular fibrillation. When used for local anae ...
, mepivacaine, prilocaine
Prilocaine () is a local anesthetic of the amino amide type first prepared by Claes Tegner and Nils Löfgren. In its injectable form (trade name Citanest), it is often used in dentistry. It is also often combined with lidocaine as a topical ...
, bupivacaine
Bupivacaine, marketed under the brand name Marcaine among others, is a medication used to decrease sensation in a specific small area. In nerve blocks, it is injected around a nerve that supplies the area, or into the spinal canal's epidural ...
, ropivacaine
Ropivacaine (International Nonproprietary Name, rINN) is a local anaesthetic drug belonging to the amino amide group. The name ropivacaine refers to both the racemate and the marketed ''S''-enantiomer. Ropivacaine hydrochloride is commonly mark ...
, and levobupivacaine
Levobupivacaine (International nonproprietary name, rINN) is a Local anesthetic, local anaesthetic drug indicated for minor and major General anaesthesia, surgical anaesthesia and pain management. It is a long-acting amide-type local anaesthetic ...
. Chloroprocaine is a short-acting drug (45–90 minutes), lidocaine and mepivacaine are intermediate duration (90–180 minutes), and bupivacaine, levobupivacaine, and ropivacaine are long-acting (4–18 hours). Drugs commonly used for peripheral nerve blocks include lidocaine, ropivacaine, bupivacaine, and mepivacaine.
Mechanism of action
Local anesthetics act on the voltage-gated sodium channels that conduct electrical impulses and mediate fastdepolarization
In biology, depolarization or hypopolarization is a change within a cell (biology), cell, during which the cell undergoes a shift in electric charge distribution, resulting in less negative charge inside the cell compared to the outside. Depolar ...
along nerves. Local anesthetics also act on potassium channel
Potassium channels are the most widely distributed type of ion channel found in virtually all organisms. They form potassium-selective pores that span cell membranes. Potassium channels are found in most cell types and control a wide variety of ...
s, but they block sodium channels more.
Lidocaine
Lidocaine, also known as lignocaine and sold under the brand name Xylocaine among others, is a local anesthetic of the amino amide type. It is also used to treat ventricular tachycardia and ventricular fibrillation. When used for local anae ...
preferentially binds to the inactivated state of voltage-gated sodium channels, but has also been found to bind potassium channels, G protein-coupled receptor
G protein-coupled receptors (GPCRs), also known as seven-(pass)-transmembrane domain receptors, 7TM receptors, heptahelical receptors, serpentine receptors, and G protein-linked receptors (GPLR), form a large group of evolutionarily related ...
s, NMDA receptor
The ''N''-methyl-D-aspartate receptor (also known as the NMDA receptor or NMDAR), is a glutamate receptor and predominantly Ca2+ ion channel found in neurons. The NMDA receptor is one of three types of ionotropic glutamate receptors, the other ...
s, and calcium channel
A calcium channel is an ion channel which shows selective permeability to calcium ions. It is sometimes synonymous with voltage-gated calcium channel, which are a type of calcium channel regulated by changes in membrane potential. Some calcium chan ...
s ''in vitro
''In vitro'' (meaning ''in glass'', or ''in the glass'') Research, studies are performed with Cell (biology), cells or biological molecules outside their normal biological context. Colloquially called "test-tube experiments", these studies in ...
''. The duration of the block is mostly influenced by the amount of time the anesthetic is near the nerve. Lipid solubility, blood flow in the tissue, and presence of vasoconstrictors with the anesthetic all play a role in this. A higher lipid solubility makes the anesthetic more potent and have a longer duration of action; however, it also increases the toxicity of the drug.
Adjuvants
Local anaesthetics are often combined with adjuvants, drugs that boost the effect of each other, with the end goal of increasing the duration of theanalgesia
Pain management is an aspect of medicine and health care involving relief of pain (pain relief, analgesia, pain control) in various dimensions, from acute and simple to chronic and challenging. Most physicians and other health professionals ...
or shortening time of onset. Adjuvants may include epinephrine
Adrenaline, also known as epinephrine, is a hormone and medication which is involved in regulating visceral functions (e.g., respiration). It appears as a white microcrystalline granule. Adrenaline is normally produced by the adrenal glands a ...
, clonidine
Clonidine, sold under the brand name Catapres among others, is an α2A-adrenergic receptor agonist medication used to treat high blood pressure, attention deficit hyperactivity disorder (ADHD), drug withdrawal (e.g., alcohol, opioids, or nic ...
, and dexmedetomidine. Vasoconstriction
Vasoconstriction is the narrowing of the blood vessels resulting from contraction of the muscular wall of the vessels, in particular the large arteries and small arterioles. The process is the opposite of vasodilation, the widening of blood vesse ...
caused by local anesthetic may be further enhanced synergistically with the addition of epinephrine, the most widely used additive. Epinephrine increases the length of analgesic duration and decreases blood flow by acting as an agonist at the α1-adrenoceptor. Dexmedetomidine is not as widely used as epinephrine. Studies in humans indicate improved onset time and increased duration of analgesia.
It is unclear if the use of epinephrine in addition to lidocaine is safe for nerve blocks of fingers and toes due to insufficient evidence. Another 2015 review states that it is safe in those who are otherwise healthy. The addition of dexamethasone to a nerve block or if given intravenously for surgery can prolong the duration of an upper limb nerve block leading to reduction in postoperative opioid consumption.
Duration of action
The duration of the nerve block depends on the type of local anesthetics used and the amount injected around the target nerve. There are short acting (45–90 minutes), intermediate duration (90–180 minutes), and long acting anesthetics (4–18 hours). Block duration can be prolonged with use of a vasoconstrictor such as epinephrine, which decreases the diffusion of the anesthetic away from the nerve. There are various types of nerve blocks currently performed. Therapeutic blocks may be used for acute pain patients, diagnostic blocks are used to find pain sources, prognostic blocks are used to determine subsequent pain management options, preemptive blocks minimize postoperative pain, and some blocks can be used in place of surgery. Certain surgeries may benefit from placing a catheter that stays in place for 2–3 days postoperatively. Catheters are indicated for some surgeries where the expected postoperative pain lasts longer than 15–20 hours. Pain medication can be injected through the catheter to prevent a spike in pain when the initial block wears off. Nerve blocks may also reduce the risk of developing persistent postoperative pain several months after surgery. Local anesthetic nerve blocks are sterile procedures that can be performed with the help of anatomical landmarks,ultrasound
Ultrasound is sound with frequency, frequencies greater than 20 Hertz, kilohertz. This frequency is the approximate upper audible hearing range, limit of human hearing in healthy young adults. The physical principles of acoustic waves apply ...
, fluoroscopy
Fluoroscopy (), informally referred to as "fluoro", is an imaging technique that uses X-rays to obtain real-time moving images of the interior of an object. In its primary application of medical imaging, a fluoroscope () allows a surgeon to see t ...
(a live X-ray), or CT. Use of any one of these imaging modalities enables the physician to view the placement of the needle. Electrical stimulation
Functional electrical stimulation (FES) is a technique that uses low-energy electrical pulses to artificially generate body movements in individuals who have been paralyzed due to injury to the central nervous system. More specifically, FES ca ...
can also provide feedback on the proximity of the needle to the target nerve.
Complications
Complications of nerve blocks most commonly include infection, bleeding, and block failure. Nerve injury is a rare side effect occurring roughly 0.03–0.2% of the time. Regarding block failure, patients can differ in their local response to anesthetic and resistance is an under-recognized cause of injection failure. In 2003, Trescot interviewed 1198 consecutive patients; 250 patients noted failure of relief from an injection of bupivacaine or had a history of difficulty getting numb at the dentist. Skin testing with lidocaine, bupivacaine, and mepivacaine was performed to identify the most effective local anesthetic (i.e. the local anesthetic that caused the most skin numbness). Ninety of those patients (7.5% of the total patients, but 36% of the test group) were numb only to mepivacaine, and an additional 43 patients (3.8% of the total patients, but 17% of the test group) only got numb to lidocaine. Thus, 133 of 250 patients with a history of difficulty with local anesthetic analgesia (53%) and 11% of the total patients, did not get numb with bupivacaine (the most commonly used anesthetic), suggesting a significant potential false-negative response to diagnostic injections.Local anesthetic toxicity
A local anesthetic (LA) is a medication that causes absence of all sensation (including pain) in a specific body part without loss of consciousness, providing local anesthesia, as opposed to a general anesthetic, which eliminates all sensation ...
, the most dangerous complication, is often first detected by symptoms of numbness and tingling around the mouth, metallic taste, or ringing in the ears. Additionally, it may lead to seizures, arrhythmias
Arrhythmias, also known as cardiac arrhythmias, are irregularities in the heartbeat, including when it is too fast or too slow. Essentially, this is anything but normal sinus rhythm. A resting heart rate that is too fast – above 100 beats ...
, and may progress to cardiac arrest. This reaction may stem from an allergy, excessive dose, or intravascular injection. Local anesthetic systemic toxicity (LAST) can include neurologic and cardiovascular symptoms including cardiovascular collapse and death. Other side effects can result from the specific medications used; for example, transient tachycardia may result if epinephrine is administered in the block. Despite these possible complications, procedures done under regional anesthesia (nerve block with or without intravenous sedation) carry a lower anesthetic risk than general anesthesia.
Other complications include nerve injury which has an extremely low rate of 0.029–0.2%. Some research even suggests that ultrasound lowers the risk to 0.0037%. The use of ultrasound and nerve stimulation has greatly improved practitioners' ability to safely administer nerve blocks. Nerve injury most often occurs from ischaemia
Ischemia or ischaemia is a restriction in blood supply to any tissue, muscle group, or organ of the body, causing a shortage of oxygen that is needed for cellular metabolism (to keep tissue alive). Ischemia is generally caused by problems ...
, compression, direct neurotoxicity, needle laceration, and inflammation.
Neurolytic block
A neurolytic block can be: * A form of nerve block involving the deliberate injury of a nerve by freezing or heating (" neurotomy"). * Application of chemicals as alcohol or phenol in glycerin (" neurolysis"). These interventions cause degeneration of the nerve's fibers and temporary (a few months, usually) interference with the transmission of nerve signals. In these procedures, the thin protective layer around the nerve fiber, thebasal lamina
The basal lamina is a layer of extracellular matrix secreted by the epithelial cells, on which the epithelium sits. It is often incorrectly referred to as the basement membrane, though it does constitute a portion of the basement membrane. The b ...
, is preserved so that, as a damaged fiber regrows, it travels within its basal lamina tube and connects with the correct loose end, and function may be restored.
* Surgical cutting of a nerve ( neurectomy), severs these basal lamina tubes, and without them to channel the regrowing fibers to their lost connections, over time a painful neuroma or deafferentation pain may develop. This is why the neurolytic is usually preferred over the surgical block.
The neurolytic block is sometimes used to temporarily reduce or eliminate pain in part of the body. Targets include
* the celiac plexus
The celiac plexus, also known as the solar plexus because of its radiating nerve fibers, is a nerve plexus, complex network of nerves located in the abdomen, near where the celiac trunk, superior mesenteric artery, and renal arteries branch fro ...
, most commonly for cancer of the gastrointestinal tract up to the transverse colon, and pancreatic cancer, but also for stomach cancer, gall bladder cancer, adrenal mass, common bile duct cancer, chronic pancreatitis and active intermittent porphyria
Porphyria ( or ) is a group of disorders in which substances called porphyrins build up in the body, adversely affecting the skin or nervous system. The types that affect the nervous system are also known as Porphyria#Acute porphyrias, acute p ...
* the splanchnic nerve
The splanchnic nerves are paired visceral nerves (nerves that contribute to the innervation of the internal organs), carrying fibers of the autonomic nervous system ( visceral efferent fibers) as well as sensory fibers from the organs ( viscera ...
, for retroperitoneal pain, and similar conditions to those addressed by the celiac plexus block but, because of its higher rate of complications, used only if the celiac plexus block is not producing adequate relief
* the hypogastric plexus, for cancer affecting the descending colon, sigmoid colon and rectum, as well as cancers of the bladder, prostatic urethra, prostate, seminal vesicles, testicles, uterus, ovary and vaginal fundus
* the ganglion impar
The pelvic portion of each sympathetic trunk is situated in front of the sacrum, medial to the anterior sacral foramina. It consists of four or five small sacral ganglia, connected together by interganglionic cords, and continuous above with the ...
, for the perinium, vulva, anus, distal rectum, distal urethra, and distal third of the vagina
* the stellate ganglion, usually for head and neck cancer, or sympathetically mediated arm and hand pain
* the triangle of auscultation
The triangle of auscultation is a relative thinning of the musculature of the back, situated along the medial border of the scapula which allows for improved listening to the lungs.
Boundaries
It has the following boundaries:
* medially, by the ...
for pain from rib fracture
A rib fracture is a break in a rib bone. This typically results in chest pain that is worse with inspiration. Bruising may occur at the site of the break. When several ribs are broken in several places a flail chest results. Potential complicat ...
s and post thoracotomy using a rhomboid intercostal block
* the intercostal nerves
The intercostal nerves are part of the somatic nervous system, and arise from the anterior rami of the thoracic spinal nerves from T1 to T11. The intercostal nerves are distributed chiefly to the thoracic pleura and abdominal peritoneum, and dif ...
, which serve the skin of the chest and abdomen
* and a dorsal root ganglion may be treated by targeting the root inside the subarachnoid cavity, most effective for pain in the chest or abdominal wall, but also used for other areas including arm/hand or leg/foot pain.
Neurectomy
Neurectomy is asurgical
Surgery is a medical specialty that uses manual and instrumental techniques to diagnose or treat pathological conditions (e.g., trauma, disease, injury, malignancy), to alter bodily functions (e.g., malabsorption created by bariatric surgery ...
procedure in which a nerve
A nerve is an enclosed, cable-like bundle of nerve fibers (called axons). Nerves have historically been considered the basic units of the peripheral nervous system. A nerve provides a common pathway for the Electrochemistry, electrochemical nerv ...
or section of a nerve is severed or removed. Cutting a sensory nerve severs its basal lamina tubes, and without them to channel the regrowing fibers to their lost connections, over time a painful neuroma or deafferentation pain may develop. This is why the neurolytic is usually preferred over the surgical sensory nerve block. This surgery is performed in rare cases of severe chronic pain
Chronic pain is pain that persists or recurs for longer than 3 months.https://icd.who.int/browse/2025-01/mms/en#1581976053 It is also known as gradual burning pain, electrical pain, throbbing pain, and nauseating pain. This type of pain is in cont ...
where no other treatments have been successful, and for other conditions such as involuntary twitching and excessive blushing or sweating.McMahon, M. (2012, November 6). What is a Neurectomy? (O. Wallace, Ed.) Retrieved from wise GEEK: http://www.wisegeek.com/what-is-a-neurectomy.htm#
A brief "rehearsal" local anesthetic nerve block is usually performed before the actual neurectomy to determine efficacy and detect side effects. The patient is typically under general anesthetic
General anaesthetics (or anesthetics) are often defined as compounds that induce a loss of consciousness in humans or loss of righting reflex in animals. Clinical definitions are also extended to include an induced coma that causes lack of aware ...
during the neurectomy, which is performed by a neurosurgeon
Neurosurgery or neurological surgery, known in common parlance as brain surgery, is the medical specialty that focuses on the surgical treatment or rehabilitation of disorders which affect any portion of the nervous system including the brain, ...
.
Regional blocks
Upper extremity
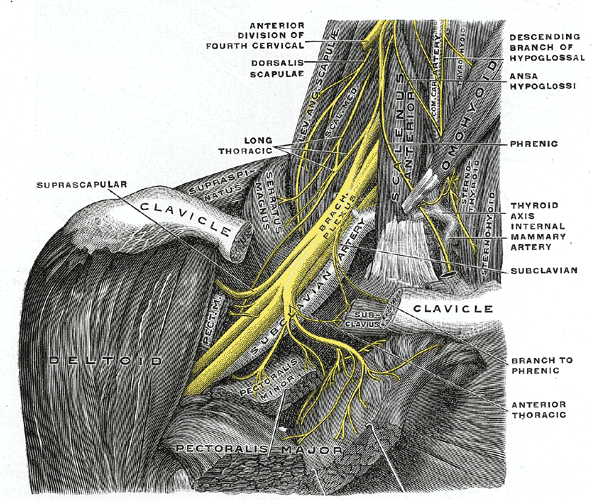 The brachial plexus is a bundle of nerves innervating the shoulder and arm and can be blocked at different levels depending on the type of upper extremity surgery being performed. Interscalene brachial plexus blocks can be done before shoulder, arm, and elbow surgery. The interscalene block is done at the neck where the brachial plexus emerges between the anterior and middle scalene muscles. Lidocaine is injected first to numb the skin and then a blunt needle is used to protect the nerves from damage as the physician places the needle very close to the nerves. The needle goes in about 3–4 cm and a single shot of local anesthetic is injected or a catheter is placed. The most common local anesthetics used at the site of the nerves are bupivicaine, mepivicaine, and chloroprocaine. There is a very high chance that the
The brachial plexus is a bundle of nerves innervating the shoulder and arm and can be blocked at different levels depending on the type of upper extremity surgery being performed. Interscalene brachial plexus blocks can be done before shoulder, arm, and elbow surgery. The interscalene block is done at the neck where the brachial plexus emerges between the anterior and middle scalene muscles. Lidocaine is injected first to numb the skin and then a blunt needle is used to protect the nerves from damage as the physician places the needle very close to the nerves. The needle goes in about 3–4 cm and a single shot of local anesthetic is injected or a catheter is placed. The most common local anesthetics used at the site of the nerves are bupivicaine, mepivicaine, and chloroprocaine. There is a very high chance that the phrenic nerve
The phrenic nerve is a mixed nerve that originates from the C3–C5 spinal nerves in the neck. The nerve is important for breathing because it provides exclusive motor control of the diaphragm, the primary muscle of respiration. In humans, t ...
, which innervates the diaphragm, will be blocked so this block should only be done on patients who have use of their accessory respiratory muscles. The block may not affect the C8 and T1 roots which supply part of the hand, so it is usually not done for hand surgeries.
The supraclavicular and infraclavicular blocks can be performed for surgeries on the humerus
The humerus (; : humeri) is a long bone in the arm that runs from the shoulder to the elbow. It connects the scapula and the two bones of the lower arm, the radius (bone), radius and ulna, and consists of three sections. The humeral upper extrem ...
, elbow, and hand. These blocks are indicated for the same surgeries but they provide different views of the nerves, so it depends on the individual patient's anatomy to determine which block should be performed. A pneumothorax
A pneumothorax is collection of air in the pleural space between the lung and the chest wall. Symptoms typically include sudden onset of sharp, one-sided chest pain and dyspnea, shortness of breath. In a minority of cases, a one-way valve is ...
is a risk with these blocks, so the pleura
The pleurae (: pleura) are the two flattened closed sacs filled with pleural fluid, each ensheathing each lung and lining their surrounding tissues, locally appearing as two opposing layers of serous membrane separating the lungs from the med ...
should be checked with ultrasound to make sure the lung was not punctured during the block.
The axillary block is indicated for elbow, forearm, and hand surgery. It anesthetizes the median, ulnar, and radial nerves. This block is useful because it has less risk than the interscalene (spinal cord or vertebral artery puncture) or supraclavicular (pneumothorax) brachial plexus blocks.
Lower extremity
femoral nerve block
A femoral nerve block is a nerve block that uses local anesthetic to achieve analgesia in the leg. The block works by affecting the femoral nerve.
A femoral nerve block (FNB) results in anesthesia of the skin and muscles of the anterior thigh and ...
is indicated for femur, anterior thigh, and knee surgery. It is performed slightly inferior to the inguinal ligament, and the nerve is under the fascia iliaca.
The sciatic nerve block is done for surgeries at or below the knee. The nerve is located in the gluteus maximus muscle. The popliteal block is done for ankle, achilles tendon, and foot surgery. It is done above the knee on the posterior leg where the sciatic nerve starts splitting into the common peroneal and tibial nerves.
The saphenous nerve block is often done in combination with the popliteal block for surgeries below the knee. The saphenous nerve is numbed at the medial part of the lower thigh under the sartorius muscle.
The lumbar plexus block is an advanced technique indicated for hip, anterior thigh, and knee surgery. The lumbar plexus is composed of nerves originating from L1 to L4 spinal roots such as the iliohypogastric, ilioinguinal, genitofemoral, lateral femoral cutaneous, femoral, and obturator nerves. Since the plexus is located deep, there is an increased risk of local anesthetic toxicity, so less toxic anesthetics like chloroprocaine or mepivacaine mixed with ropivacaine are often recommended. A curvilinear ultrasound probe can be used but it is often difficult to see the plexus, so a nerve stimulator is used to locate it.
Genicular nerve block
Temporary anesthesia of genicular (knee) sensory nerves is used as a diagnostic procedure to help determine whether or not a person with chronic severe knee pain may be a candidate for more durable treatment withradiofrequency ablation
Radiofrequency ablation (RFA), also called fulguration, is a medical procedure in which part of the electrical conduction system of the heart, tumor, sensory nerves or a dysfunctional tissue is ablated using the heat generated from medium fre ...
. Using imaging guidance, needles are placed near branches of the genicular nerves, which are then anesthetized with a short-lasting anesthetic, such as lidocaine
Lidocaine, also known as lignocaine and sold under the brand name Xylocaine among others, is a local anesthetic of the amino amide type. It is also used to treat ventricular tachycardia and ventricular fibrillation. When used for local anae ...
. Although selection of the genicular nerve branches or other sensory nerves may vary by clinician experience, blocking the superior lateral, superior medial, and inferior medial genicular nerves has proven successful for reducing knee pain.
Following genicular nerve block, knee pain is monitored over hours to days when the local anesthetic is blocking the knee joint pain. In people who experience a significant alleviation of knee pain with this diagnostic test, radiofrequency ablation of the same genicular nerves can then be performed as a treatment for long-lasting pain relief, which may persist over several months to two years.
Paravertebral nerve
The paravertebral block is versatile and can be used for various surgeries depending on the vertebral level it is done. A block at the neck in the cervical region is useful for thyroid gland and carotid artery surgery. At the chest and abdomen in the thoracic region, blocks are used for breast, thoracic, and abdominal surgery. One of the first instances on using continuous paravertebral blockade in the body was by the thoracic team led by Sabanathan in Bradford. A block at the hip in the lumbar region is indicated for hip, knee, and anterior thigh surgeries. The paravertebral block provides unilateral analgesia, but bilateral blocks can be performed for abdominal surgeries. Since it is a unilateral block, it may be chosen over epidurals for patients who cannot tolerate the hypotension that follows bilateral sympathectomy. The paravertebral space is located a couple centimeters lateral to the spinous process and is bounded posteriorly by the superior costotransverse ligament and anteriorly by the parietal pleura. Complications include pneumothorax, vascular puncture, hypotension, and pleural puncture.Erector spinae plane block
The erector spinae plan block is sometimes suggested for thoracic-related pain control to reduce the need for opioids after surgery. This block can provide pain control for a large part of the hemithorax region. Examples include breast surgery, rib fractures (including posterior fractures), and chest-wall related pain. This block may also be applied at lower levels of the spine (lumbar and sacral levels) to target pelvic abdominal regions of the body that require pain relief. There is also some evidence that this block may be helpful for managing pain in conditions and procedures such as pancreatitis andappendicitis
Appendicitis is inflammation of the Appendix (anatomy), appendix. Symptoms commonly include right lower abdominal pain, nausea, vomiting, fever and anorexia (symptom), decreased appetite. However, approximately 40% of people do not have these t ...
, thoracotomy, hernia
A hernia (: hernias or herniae, from Latin, meaning 'rupture') is the abnormal exit of tissue or an organ (anatomy), organ, such as the bowel, through the wall of the cavity in which it normally resides. The term is also used for the normal Devel ...
repairs (ventral), lumbar fusion surgery, the Nuss procedure (pectus excavatum treatment), and kidney stone
Kidney stone disease (known as nephrolithiasis, renal calculus disease, or urolithiasis) is a crystallopathy and occurs when there are too many minerals in the urine and not enough liquid or hydration. This imbalance causes tiny pieces of cr ...
removal procedures.
References
{{Authority control Regional anesthesia