|
Hypoxemia
Hypoxemia (also spelled hypoxaemia) is an abnormally low level of oxygen in the blood. More specifically, it is oxygen deficiency in arterial blood. Hypoxemia is usually caused by pulmonary disease. Sometimes the concentration of oxygen in the air is decreased leading to hypoxemia. Definition ''Hypoxemia'' refers to the low level of oxygen in arterial blood. Tissue hypoxia refers to low levels of oxygen in the tissues of the body and the term ''hypoxia'' is a general term for low levels of oxygen. Hypoxemia is usually caused by pulmonary disease whereas tissue oxygenation requires additionally adequate circulation of blood and perfusion of tissue to meet metabolic demands. Hypoxemia is usually defined in terms of reduced partial pressure of oxygen (mm Hg) in arterial blood, but also in terms of reduced content of oxygen (ml oxygen per dl blood) or percentage saturation of hemoglobin (the oxygen-binding protein within red blood cells) with oxygen, which is either found singly o ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] [Amazon] |
Alveolar–arterial Gradient
The Alveolar–arterial gradient (A-, or A–a gradient), is a measure of the difference between the alveolar concentration (A) of oxygen and the arterial (a) concentration of oxygen. It is a useful parameter for narrowing the differential diagnosis of hypoxemia. The A–a gradient helps to assess the integrity of the alveolar capillary unit. For example, in high altitude, the arterial oxygen is low but only because the alveolar oxygen () is also low. However, in states of ventilation perfusion mismatch, such as pulmonary embolism or right-to-left shunt, oxygen is not effectively transferred from the alveoli to the blood which results in an elevated A-a gradient. In a perfect system, no A-a gradient would exist: oxygen would diffuse and equalize across the capillary membrane, and the pressures in the arterial system and alveoli would be effectively equal (resulting in an A-a gradient of zero). However even though the partial pressure of oxygen is about equilibrated between the ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] [Amazon] |
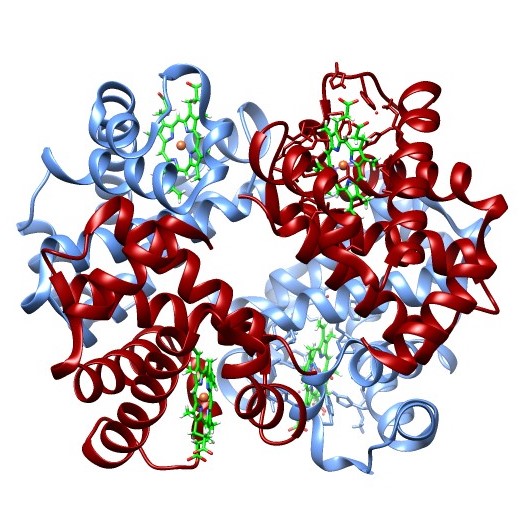
Hemoglobin
Hemoglobin (haemoglobin, Hb or Hgb) is a protein containing iron that facilitates the transportation of oxygen in red blood cells. Almost all vertebrates contain hemoglobin, with the sole exception of the fish family Channichthyidae. Hemoglobin in the blood carries oxygen from the respiratory organs (lungs or gills) to the other tissues of the body, where it releases the oxygen to enable aerobic respiration which powers an animal's metabolism. A healthy human has 12to 20grams of hemoglobin in every 100mL of blood. Hemoglobin is a metalloprotein, a chromoprotein, and a globulin. In mammals, hemoglobin makes up about 96% of a red blood cell's dry matter, dry weight (excluding water), and around 35% of the total weight (including water). Hemoglobin has an oxygen-binding capacity of 1.34mL of O2 per gram, which increases the total blood oxygen capacity seventy-fold compared to dissolved oxygen in blood plasma alone. The mammalian hemoglobin molecule can bind and transport up to four ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] [Amazon] |
Respiratory Failure
Respiratory failure results from inadequate gas exchange by the respiratory system, meaning that the arterial oxygen, carbon dioxide, or both cannot be kept at normal levels. A drop in the oxygen carried in the blood is known as hypoxemia; a rise in arterial carbon dioxide levels is called hypercapnia. Respiratory failure is classified as either Type 1 or Type 2, based on whether there is a high carbon dioxide level, and can be acute or chronic. In clinical trials, the definition of respiratory failure usually includes increased respiratory rate, abnormal blood gases (hypoxemia, hypercapnia, or both), and evidence of increased work of breathing. Respiratory failure causes an altered state of consciousness due to ischemia in the brain. The typical partial pressure reference values are oxygen Pa more than 80 mmHg (11 kPa) and carbon dioxide Pa less than 45 mmHg (6.0 kPa). Cause A variety of conditions that can potentially result in respiratory failure. The etiologie ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] [Amazon] |
Pulmonary Hypertension
Pulmonary hypertension (PH or PHTN) is a condition of increased blood pressure in the pulmonary artery, arteries of the lungs. Symptoms include dypsnea, shortness of breath, Syncope (medicine), fainting, tiredness, chest pain, pedal edema, swelling of the legs, and a fast heartbeat. The condition may make it difficult to exercise. Onset is typically gradual. According to the definition at the 6th World Symposium of Pulmonary Hypertension in 2018, a patient is deemed to have pulmonary hypertension if the pulmonary mean arterial pressure is greater than 20mmHg at rest, revised down from a purely arbitrary 25mmHg, and pulmonary vascular resistance (PVR) greater than 3 Wood units. The cause is often unknown. Risk factors include a family history, prior pulmonary embolism (blood clots in the lungs), HIV/AIDS, sickle cell disease, cocaine use, chronic obstructive pulmonary disease, sleep apnea, living at high altitudes, and problems with the mitral valve. The underlying mechanism typ ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] [Amazon] |
Right Sided Heart Failure
Heart failure (HF), also known as congestive heart failure (CHF), is a syndrome caused by an impairment in the heart's ability to fill with and pump blood. Although symptoms vary based on which side of the heart is affected, HF typically presents with shortness of breath, excessive fatigue, and bilateral leg swelling. The severity of the heart failure is mainly decided based on ejection fraction and also measured by the severity of symptoms. Other conditions that have symptoms similar to heart failure include obesity, kidney failure, liver disease, anemia, and thyroid disease. Common causes of heart failure include coronary artery disease, heart attack, high blood pressure, atrial fibrillation, valvular heart disease, excessive alcohol consumption, infection, and cardiomyopathy. These cause heart failure by altering the structure or the function of the heart or in some cases both. There are different types of heart failure: right-sided heart failure, which affects the righ ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] [Amazon] |
Right-to-left Shunt
A right-to-left shunt is a cardiac shunt which allows blood to flow from the right heart to the left heart. This terminology is used both for the abnormal state in humans and for normal physiological shunts in reptiles. Clinical Significance A right-to-left shunt occurs when: #there is an opening or passage between the atria, ventricles, and/or great vessels; ''and'', #right heart pressure is higher than left heart pressure and/or the shunt has a one-way valvular opening. Small physiological, or "normal", shunts are seen due to the return of bronchial artery blood and coronary blood through the Thebesian veins, which are deoxygenated, to the left side of the heart. Causes Congenital defects can lead to right-to-left shunting immediately after birth: * Persistent truncus arteriosus (minimal cyanosis) * Transposition of great vessels * Tricuspid atresia * Tetralogy of Fallot * Total anomalous pulmonary venous return A mnemonic to remember the conditions associated with rig ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] [Amazon] |
Arterial Blood Gas
An arterial blood gas (ABG) test, or arterial blood gas analysis (ABGA) measures the amounts of arterial gases, such as oxygen and carbon dioxide. An ABG test requires that a small volume of blood be drawn from the radial artery with a syringe and a thin needle, but sometimes the femoral artery in the groin or another site is used. The blood can also be drawn from an arterial catheter. An ABG test measures the blood gas tension values of the arterial partial pressure of oxygen (PaO2), and the arterial partial pressure of carbon dioxide (PaCO2), and the blood's pH. In addition, the arterial oxygen saturation (SaO2) can be determined. Such information is vital when caring for patients with critical illnesses or respiratory disease. Therefore, the ABG test is one of the most common tests performed on patients in intensive-care units. In other levels of care, pulse oximetry plus transcutaneous carbon-dioxide measurement is a less invasive, alternative method of obtaining simila ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] [Amazon] |
Respiratory Distress
Shortness of breath (SOB), known as dyspnea (in AmE) or dyspnoea (in BrE), is an uncomfortable feeling of not being able to breathe well enough. The American Thoracic Society defines it as "a subjective experience of breathing discomfort that consists of qualitatively distinct sensations that vary in intensity", and recommends evaluating dyspnea by assessing the intensity of its distinct sensations, the degree of distress and discomfort involved, and its burden or impact on the patient's activities of daily living. Distinct sensations include effort/work to breathe, chest tightness or pain, and "air hunger" (the feeling of not enough oxygen). The tripod position is often assumed to be a sign. Dyspnea is a normal symptom of heavy physical exertion but becomes pathological if it occurs in unexpected situations, when resting or during light exertion. In 85% of cases it is due to asthma, pneumonia, reflux/LPR, cardiac ischemia, COVID-19, interstitial lung disease, congestive hea ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] [Amazon] |
Oxygen–hemoglobin Dissociation Curve
The oxygen–hemoglobin dissociation curve, also called the oxyhemoglobin dissociation curve or oxygen dissociation curve (ODC), is a curve that plots the proportion of hemoglobin in its saturated (oxygen-laden) form on the vertical axis against the prevailing oxygen tension on the horizontal axis. This curve is an important tool for understanding how our blood carries and releases oxygen. Specifically, the oxyhemoglobin dissociation curve relates oxygen saturation (SO2) and partial pressure of oxygen in the blood (PO2), and is determined by what is called "hemoglobin affinity for oxygen"; that is, how readily hemoglobin acquires and releases oxygen molecules into the fluid that surrounds it. Background Hemoglobin (Hb) is the primary vehicle for transporting oxygen in the blood. Each hemoglobin molecule has the capacity to carry four oxygen molecules. These molecules of oxygen bind to the globin chain of the heme prosthetic group. When hemoglobin has no bound oxygen, nor bound ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] [Amazon] |
Cyanosis
Cyanosis is the change of Tissue (biology), tissue color to a bluish-purple hue, as a result of decrease in the amount of oxygen bound to the hemoglobin in the red blood cells of the capillary bed. Cyanosis is apparent usually in the Tissue (biology), body tissues covered with thin skin, including the mucous membranes, lips, nail beds, and ear lobes. Some medications may cause discoloration such as medications containing amiodarone or silver. Furthermore, mongolian spots, large birthmarks, and the consumption of food products with blue or purple dyes can also result in the bluish skin tissue discoloration and may be mistaken for cyanosis. Appropriate physical examination and history taking is a crucial part to diagnose cyanosis. Management of cyanosis involves treating the main cause, as cyanosis is not a disease, but rather a symptom. Cyanosis is further classified into central cyanosis and peripheral cyanosis. Pathophysiology The mechanism behind cyanosis is different dep ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] [Amazon] |
Ventilation Perfusion Mismatch
Ventilation may refer to: * Ventilation (physiology), the movement of air between the environment and the lungs via inhalation and exhalation ** Mechanical ventilation, in medicine, using artificial methods to assist breathing *** Respirator, a machine designed to move breathable air into and out of the lungs * Ventilation (architecture), the process of "changing" or replacing air in any space to provide high indoor air quality * Ventilation (firefighting), the expulsion of heat and smoke from a fire building * Ventilation (mining), flow of air to the underground workings of a mine of sufficient volume to dilute and remove noxious gases See also * Heat recovery ventilation * Heating, ventilation, and air conditioning, the technology of indoor and vehicular environmental comfort * Mechanical fan * Reebok Ventilator, a shoe * Vent (other) Vent or vents may refer to: Science and technology Biology *Vent, the cloaca region of an animal * Vent DNA polymerase, a thermostabl ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] [Amazon] |