|
Cardiorenal Syndrome
Cardiorenal syndrome (CRS) refers to the spectrum of disorders in which acute or chronic dysfunction of the heart or kidneys leads to acute or chronic dysfunction of the other. The condition is classified into five subtypes based on the primary organ dysfunction and whether the disease process is acute or chronic. The heart and the kidneys maintain hemodynamic stability and organ perfusion through an intricate network. CRS results from a complex interplay of hemodynamic alterations, neurohormonal activation, inflammatory mediators, and endothelial dysfunction, all contributing to progressive organ injury. Cardiorenal syndrome is commonly associated with conditions such as heart failure, chronic kidney disease (CKD), acute kidney injury (AKI), and systemic hypertension. Management of CRS primarily focuses on addressing the underlying cause while mitigating the complications associated with the syndrome. Since volume overload is a predominant feature in most patients, treat ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |
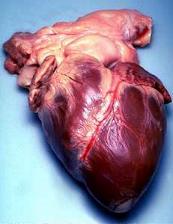
Heart
The heart is a muscular Organ (biology), organ found in humans and other animals. This organ pumps blood through the blood vessels. The heart and blood vessels together make the circulatory system. The pumped blood carries oxygen and nutrients to the tissue, while carrying metabolic waste such as carbon dioxide to the lungs. In humans, the heart is approximately the size of a closed fist and is located between the lungs, in the middle compartment of the thorax, chest, called the mediastinum. In humans, the heart is divided into four chambers: upper left and right Atrium (heart), atria and lower left and right Ventricle (heart), ventricles. Commonly, the right atrium and ventricle are referred together as the right heart and their left counterparts as the left heart. In a healthy heart, blood flows one way through the heart due to heart valves, which prevent cardiac regurgitation, backflow. The heart is enclosed in a protective sac, the pericardium, which also contains a sma ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |
Mineralocorticoid Receptor Antagonist
A mineralocorticoid receptor antagonist (MRA or MCRA) or aldosterone antagonist, is a diuretic drug which antagonizes the action of aldosterone at mineralocorticoid receptors. This group of drugs is often used as adjunctive therapy, in combination with other drugs, for the management of chronic heart failure. Spironolactone, the first member of the class, is also used in the management of hyperaldosteronism (including Conn's syndrome) and female hirsutism (due to additional antiandrogen actions). Most antimineralocorticoids, including spironolactone, are steroidal spirolactones. Finerenone is a nonsteroidal antimineralocorticoid. Medical uses Mineralocorticoid receptor antagonists are diuretic drugs that work primarily on the kidneys. They decrease sodium reabsorption, which leads to increased water excretion by the kidneys. By regulating water excretion, mineralocorticoid receptor antagonists lower blood pressure and reduce fluid around the heart which can be very benefici ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |
Diuretics
A diuretic () is any substance that promotes diuresis, the increased production of urine. This includes forced diuresis. A diuretic tablet is sometimes colloquially called a water tablet. There are several categories of diuretics. All diuretics increase the excretion of water from the body, through the kidneys. There exist several classes of diuretic, and each works in a distinct way. Alternatively, an antidiuretic, such as vasopressin (antidiuretic hormone), is an agent or drug which reduces the excretion of water in urine. Medical uses In medicine, diuretics are used to treat heart failure, liver cirrhosis, hypertension, influenza, water poisoning, and certain kidney diseases. Some diuretics, such as acetazolamide, help to make the urine more alkaline, and are helpful in increasing excretion of substances such as aspirin in cases of overdose or poisoning. Diuretics are sometimes abused by people with an eating disorder, especially people with bulimia nervosa, with the goal of ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |
Creatinine
Creatinine (; ) is a breakdown product of creatine phosphate from muscle and protein metabolism. It is released at a constant rate by the body (depending on muscle mass). Biological relevance Serum creatinine (a blood measurement) is an important indicator of kidney function, because it is an easily measured byproduct of muscle metabolism that is excreted unchanged by the kidneys. Creatinine itself is produced via a biological system involving creatine, phosphocreatine (also known as creatine phosphate), and adenosine triphosphate (ATP, the body's immediate energy supply). Creatine is synthesized primarily in the liver by methylation of glycocyamine (guanidino acetate, synthesized in the kidney from the amino acids arginine and glycine) by S-adenosyl methionine. It is then transported in the blood to other organs, muscles, and the brain, where it is phosphorylated to phosphocreatine, a high-energy compound. Creatine conversion to phosphocreatine is catalysed by creatine ki ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |
Jugular Venous Distension
The jugular venous pressure (JVP, sometimes referred to as ''jugular venous pulse'') is the indirectly observed pressure over the venous system via visualization of the internal jugular vein. It can be useful in the differentiation of different forms of heart and lung disease. Classically three upward deflections and two downward deflections have been described. * The upward deflections are the "a" (atrial contraction), "c" (ventricular contraction and resulting bulging of tricuspid into the right atrium during isovolumetric systole) and "v" (venous filling). * The downward deflections of the wave are the "x" descent (the atrium relaxes and the tricuspid valve moves downward) and the "y" descent (filling of ventricle after tricuspid opening). Method Visualization The patient is positioned at a 45° incline. The head is gently turned to the left, and the right external jugular vein should be identified which may be pulsatile and the filling level noted. If the external jugular ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |
Pulmonary Edema
Pulmonary edema (British English: oedema), also known as pulmonary congestion, is excessive fluid accumulation in the tissue or air spaces (usually alveoli) of the lungs. This leads to impaired gas exchange, most often leading to shortness of breath ( dyspnea) which can progress to hypoxemia and respiratory failure. Pulmonary edema has multiple causes and is traditionally classified as cardiogenic (caused by the heart) or noncardiogenic (all other types not caused by the heart). Various laboratory tests ( CBC, troponin, BNP, etc.) and imaging studies (chest x-ray, CT scan, ultrasound) are often used to diagnose and classify the cause of pulmonary edema. Treatment is focused on three aspects: * improving respiratory function, * treating the underlying cause, and * preventing further damage and allow full recovery to the lung. Pulmonary edema can cause permanent organ damage, and when sudden (acute), can lead to respiratory failure or cardiac arrest due to hypoxia ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |
Acute Decompensated Heart Failure
Acute decompensated heart failure (ADHF) is a sudden worsening of the signs and symptoms of heart failure, which typically includes difficulty breathing (dyspnea), leg or feet swelling, and fatigue. ADHF is a common and potentially serious cause of acute respiratory distress. The condition is caused by severe congestion of multiple organs by fluid that is inadequately circulated by the failing heart. An attack of decompensation can be caused by underlying medical illness, such as myocardial infarction, an abnormal heart rhythm, infection, or thyroid disease. Acute Heart Failure Heart failure or cardiovascular insufficiency can be acute without being decompensated from a chronic condition. In this case, the signs of congestion such as weight gain and edema will not yet have developed. This is commonly due to pump failure or cardiovascular insufficiency after myocardial infarction when a significant loss of cardiac function occurs. Such patients will, have shortness of breath ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |
Peripheral Edema
Peripheral edema is edema (accumulation of fluid causing swelling) in tissues perfused by the peripheral vascular system, usually in the lower limbs. In the most dependent parts of the body (those hanging distally), it may be called dependent edema. Cause The condition is commonly associated with vascular and cardiac changes associated with aging but can be caused by many other conditions, including congestive heart failure, kidney failure, liver cirrhosis, portal hypertension, trauma, alcoholism, altitude sickness, pregnancy, hypertension, sickle cell anemia, a compromised lymphatic system or merely long periods of time sitting or standing without moving. Some medicines (e.g. amlodipine, pregabalin) may also cause or worsen the condition. Prognosis Successful treatment depends on control of the underlying cause. Severe swelling can cause permanent damage to nerves, resulting in peripheral neuropathy Peripheral neuropathy, often shortened to neuropathy, refers to damage o ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |
Acute Kidney Injury
Acute kidney injury (AKI), previously called acute renal failure (ARF), is a sudden decrease in renal function, kidney function that develops within seven days, as shown by an increase in serum creatinine or a decrease in urine output, or both. Causes of AKI are classified as either prerenal (due to decreased blood flow to the kidney), intrinsic renal (due to damage to the kidney itself), or postrenal (due to blockage of urine flow). Prerenal causes of AKI include sepsis, dehydration, hemorrhage, excessive blood loss, cardiogenic shock, heart failure, cirrhosis, and certain medications like ACE inhibitors or NSAIDs. Intrinsic renal causes of AKI include glomerulonephritis, lupus nephritis, acute tubular necrosis, certain antibiotics, and chemotherapeutic agents. Postrenal causes of AKI include kidney stones, bladder cancer, neurogenic bladder, benign prostatic hyperplasia, enlargement of the prostate, urethral stricture, narrowing of the urethra, and certain medications like anti ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |
Cardiac Output
In cardiac physiology, cardiac output (CO), also known as heart output and often denoted by the symbols Q, \dot Q, or \dot Q_ , edited by Catherine E. Williamson, Phillip Bennett is the volumetric flow rate of the heart's pumping output: that is, the volume of blood being pumped by a single Ventricle (heart), ventricle of the heart, per unit time (usually measured per minute). Cardiac output (CO) is the product of the heart rate (HR), i.e. the number of heartbeats per minute (bpm), and the stroke volume (SV), which is the volume of blood pumped from the left ventricle per beat; thus giving the formula: :CO = HR \times SV Values for cardiac output are usually denoted as L/min. For a healthy individual weighing 70 kg, the cardiac output at rest averages about 5 L/min; assuming a heart rate of 70 beats/min, the stroke volume would be approximately 70 mL. Because cardiac output is related to the quantity of blood delivered to various parts of the body, it is an important com ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |
Hypervolemia
Hypervolemia, also known as fluid overload, is the medical condition where there is too much fluid in the blood. The opposite condition is hypovolemia, which is too little fluid volume in the blood. Fluid volume excess in the intravascular compartment occurs due to an increase in total body sodium content and a consequent increase in extracellular body water. The mechanism usually stems from compromised regulatory mechanisms for sodium handling as seen in congestive heart failure (CHF), kidney failure, and liver failure. It may also be caused by excessive intake of sodium from foods, intravenous (IV) solutions and blood transfusions, medications, or diagnostic contrast dyes. Treatment typically includes administration of diuretics and limit the intake of water, fluids, sodium, and salt. Signs and symptoms The excess fluid, primarily salt and water, builds up in various locations in the body and leads to an increase in weight, swelling in the legs and arms (peripheral edema), and/ ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |