Syphilis on:
[Wikipedia]
[Google]
[Amazon]
Syphilis () is a sexually transmitted infection caused by the bacterium ''Treponema pallidum'' subspecies ''pallidum''. The signs and symptoms of syphilis vary depending in which of the four stages it presents (primary, secondary, latent, and tertiary). The primary stage classically presents with a single chancre (a firm, painless, non-itchy skin ulceration usually between 1 cm and 2 cm in diameter) though there may be multiple sores. In secondary syphilis, a diffuse rash occurs, which frequently involves the palms of the hands and soles of the feet. There may also be sores in the mouth or vagina. In latent syphilis, which can last for years, there are few or no symptoms. In tertiary syphilis, there are gumma (pathology), gummas (soft, non-cancerous growths), neurological problems, or heart symptoms. Syphilis has been known as "the great imitator" as it may cause symptoms similar to many other diseases.
Syphilis is most commonly spread through human sexual activity, sexual activity. It may also be Vertical transmission, transmitted from mother to baby during pregnancy or at birth, resulting in congenital syphilis. Other diseases caused by ''Treponema'' bacteria include yaws (''Treponema pallidum, T. pallidum'' subspecies ''pertenue''), Pinta (disease), pinta (''Treponema carateum, T. carateum''), and nonvenereal endemic syphilis (''T. pallidum'' subspecies ''endemicum''). These three diseases are not typically sexually transmitted. Diagnosis is usually made by using serological testing, blood tests; the bacteria can also be detected using dark field microscopy. The Centers for Disease Control and Prevention (U.S.) recommend all pregnant women be tested.
The risk of sexual transmission of syphilis can be reduced by using a latex or polyurethane condom. Syphilis can be effectively treated with antibiotics. The preferred antibiotic for most cases is benzathine benzylpenicillin intramuscular, injected into a muscle. In those who have a severe penicillin allergy, doxycycline or tetracycline may be used. In those with neurosyphilis, intravenous benzylpenicillin or ceftriaxone is recommended. During treatment people may develop fever, headache, and myalgia, muscle pains, a reaction known as Jarisch–Herxheimer reaction, Jarisch–Herxheimer.
In 2015, about 45.4 million people had syphilis infections, of which six million were new cases. During 2015, it caused about 107,000 deaths, down from 202,000 in 1990. After decreasing dramatically with the availability of penicillin in the 1940s, rates of infection have increased since the turn of the millennium in many countries, often in combination with HIV, human immunodeficiency virus (HIV). This is believed to be partly due to increased sexual activity, prostitution, and decreasing use of condoms.
 Tertiary syphilis may occur approximately 3 to 15 years after the initial infection, and may be divided into three different forms: gummatous syphilis (15%), late neurosyphilis (6.5%), and cardiovascular syphilis (10%). Without treatment, a third of infected people develop tertiary disease. People with tertiary syphilis are not infectious.
Gummatous syphilis or late benignity, benign syphilis usually occurs 1 to 46 years after the initial infection, with an average of 15 years. This stage is characterized by the formation of chronic gumma (pathology), gummas, which are soft, tumor-like balls of inflammation which may vary considerably in size. They typically affect the skin, bone, and liver, but can occur anywhere.
Cardiovascular syphilis usually occurs 10–30 years after the initial infection. The most common complication is syphilitic aortitis, which may result in aortic aneurysm formation.
Neurosyphilis refers to an infection involving the central nervous system. Involvement of the central nervous system in syphilis (either asymptomatic or symptomatic) can occur at any stage of the infection. It may occur early, being either asymptomatic or in the form of syphilitic meningitis; or late as meningovascular syphilis, manifesting as general paresis or tabes dorsalis.
Meningovascular syphilis involves inflammation of the small and medium arteries of the central nervous system. It can present between 1–10 years after the initial infection. Meningovascular syphilis is characterized by stroke, cranial nerve palsies and myelopathy, spinal cord inflammation. Late symptomatic neurosyphilis can develop decades after the original infection and includes 2 types; general paresis and tabes dorsalis. General paresis presents with dementia, personality changes, delusions, seizures, psychosis and depression. Tabes dorsalis is characterized by gait instability, sharp pains in the trunk and limbs, impaired positional sensation of the limbs as well as having a positive Romberg's sign. Both tabes dorsalis and general paresis may present with Argyll Robertson pupil which are pupils that constrict when the person focuses on near objects (accommodation reflex) but do not constrict when exposed to bright light (Light reflex, pupillary reflex).
Tertiary syphilis may occur approximately 3 to 15 years after the initial infection, and may be divided into three different forms: gummatous syphilis (15%), late neurosyphilis (6.5%), and cardiovascular syphilis (10%). Without treatment, a third of infected people develop tertiary disease. People with tertiary syphilis are not infectious.
Gummatous syphilis or late benignity, benign syphilis usually occurs 1 to 46 years after the initial infection, with an average of 15 years. This stage is characterized by the formation of chronic gumma (pathology), gummas, which are soft, tumor-like balls of inflammation which may vary considerably in size. They typically affect the skin, bone, and liver, but can occur anywhere.
Cardiovascular syphilis usually occurs 10–30 years after the initial infection. The most common complication is syphilitic aortitis, which may result in aortic aneurysm formation.
Neurosyphilis refers to an infection involving the central nervous system. Involvement of the central nervous system in syphilis (either asymptomatic or symptomatic) can occur at any stage of the infection. It may occur early, being either asymptomatic or in the form of syphilitic meningitis; or late as meningovascular syphilis, manifesting as general paresis or tabes dorsalis.
Meningovascular syphilis involves inflammation of the small and medium arteries of the central nervous system. It can present between 1–10 years after the initial infection. Meningovascular syphilis is characterized by stroke, cranial nerve palsies and myelopathy, spinal cord inflammation. Late symptomatic neurosyphilis can develop decades after the original infection and includes 2 types; general paresis and tabes dorsalis. General paresis presents with dementia, personality changes, delusions, seizures, psychosis and depression. Tabes dorsalis is characterized by gait instability, sharp pains in the trunk and limbs, impaired positional sensation of the limbs as well as having a positive Romberg's sign. Both tabes dorsalis and general paresis may present with Argyll Robertson pupil which are pupils that constrict when the person focuses on near objects (accommodation reflex) but do not constrict when exposed to bright light (Light reflex, pupillary reflex).
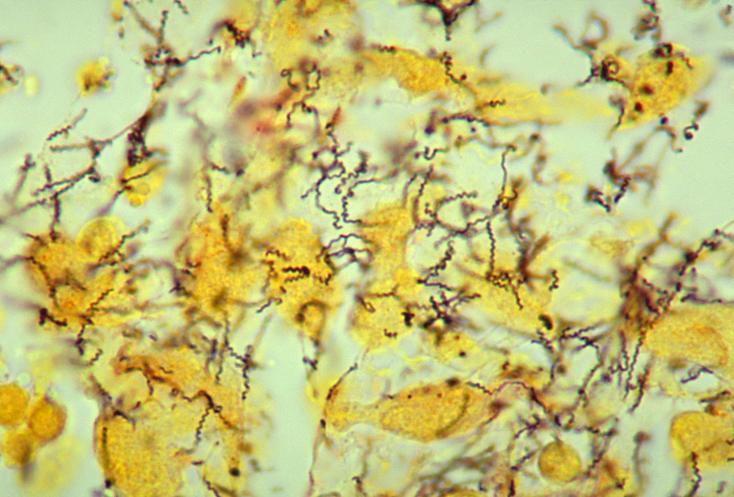 ''Treponema pallidum'' subspecies'' pallidum'' is a spiral-shaped, Gram-negative, highly mobile bacterium. Three other human diseases are caused by related ''Treponema pallidum'' subspecies, including yaws (subspecies ''pertenue''), Pinta (disease), pinta (subspecies ''carateum'') and nonvenereal endemic syphilis, bejel (subspecies ''endemicum''). Unlike subspecies ''pallidum'', they do not cause neurological disease. Humans are the only known natural reservoir for subspecies ''pallidum''. It is unable to survive more than a few days without a Host (biology), host. This is due to its small genome (1.14base pair, Mbp) failing to encode the metabolic pathways necessary to make most of its macronutrients. It has a slow doubling time of greater than 30 hours. The bacterium is known for its ability to evade the immune system and its invasiveness.
''Treponema pallidum'' subspecies'' pallidum'' is a spiral-shaped, Gram-negative, highly mobile bacterium. Three other human diseases are caused by related ''Treponema pallidum'' subspecies, including yaws (subspecies ''pertenue''), Pinta (disease), pinta (subspecies ''carateum'') and nonvenereal endemic syphilis, bejel (subspecies ''endemicum''). Unlike subspecies ''pallidum'', they do not cause neurological disease. Humans are the only known natural reservoir for subspecies ''pallidum''. It is unable to survive more than a few days without a Host (biology), host. This is due to its small genome (1.14base pair, Mbp) failing to encode the metabolic pathways necessary to make most of its macronutrients. It has a slow doubling time of greater than 30 hours. The bacterium is known for its ability to evade the immune system and its invasiveness.
 Syphilis is difficult to diagnose clinically during early infection. Confirmation is either via blood tests or direct visual inspection using Dark-field microscopy, dark field microscopy. Blood tests are more commonly used, as they are easier to perform. Diagnostic tests are unable to distinguish between the stages of the disease.
Syphilis is difficult to diagnose clinically during early infection. Confirmation is either via blood tests or direct visual inspection using Dark-field microscopy, dark field microscopy. Blood tests are more commonly used, as they are easier to perform. Diagnostic tests are unable to distinguish between the stages of the disease.
 One of the potential side effects of treatment is the Jarisch–Herxheimer reaction. It frequently starts within one hour and lasts for 24 hours, with symptoms of fever, muscle pains, headache, and a tachycardia, fast heart rate. It is caused by cytokines released by the immune system in response to lipoproteins released from rupturing syphilis bacteria.
One of the potential side effects of treatment is the Jarisch–Herxheimer reaction. It frequently starts within one hour and lasts for 24 hours, with symptoms of fever, muscle pains, headache, and a tachycardia, fast heart rate. It is caused by cytokines released by the immune system in response to lipoproteins released from rupturing syphilis bacteria.
 In 2012, about 0.5% of adults were infected with syphilis, with 6 million new cases. In 1999, it is believed to have infected 12 million additional people, with greater than 90% of cases in the developing world. It affects between 700,000 and 1.6 million pregnancies a year, resulting in spontaneous abortions, stillbirths, and congenital syphilis. During 2015, it caused about 107,000 deaths, down from 202,000 in 1990. In sub-Saharan Africa, syphilis contributes to approximately 20% of perinatal deaths. Rates are proportionally higher among Recreational drug use, intravenous drug users, those who are infected with HIV, and men who have sex with men. In the United States about 55,400 people are newly infected each year. In the United States as of 2020, rates of syphilis have increased by more than threefold; in 2018 approximately 86% of all cases of syphilis in the United States were in men. African Americans accounted for almost half of all cases in 2010. As of 2014, syphilis infections continue to increase in the United States.
Syphilis was very common in Europe during the 18th and 19th centuries. Gustave Flaubert, Flaubert found it universal among nineteenth-century Egyptian prostitutes. In the developed world during the early 20th century, infections declined rapidly with the widespread use of antibiotics, until the 1980s and 1990s. Since 2000, rates of syphilis have been increasing in the US, Canada, the UK, Australia and Europe, primarily among men who have sex with men. Rates of syphilis among US women have remained stable during this time, while rates among UK women have increased, but at a rate less than that of men. Increased rates among heterosexuals have occurred in China and Russia since the 1990s. This has been attributed to unsafe sexual practices, such as sexual promiscuity, prostitution, and decreasing use of barrier protection.
Left untreated, it has a mortality rate of 8% to 58%, with a greater death rate among males. The symptoms of syphilis have become less severe over the 19th and 20th centuries, in part due to widespread availability of effective treatment, and partly due to virulence of the bacteria. With early treatment, few complications result. Syphilis increases the risk of HIV transmission by two to five times, and coinfection is common (30–60% in some urban centers). In 2015, Cuba became the first country to eliminate mother-to-child transmission of syphilis.
In 2012, about 0.5% of adults were infected with syphilis, with 6 million new cases. In 1999, it is believed to have infected 12 million additional people, with greater than 90% of cases in the developing world. It affects between 700,000 and 1.6 million pregnancies a year, resulting in spontaneous abortions, stillbirths, and congenital syphilis. During 2015, it caused about 107,000 deaths, down from 202,000 in 1990. In sub-Saharan Africa, syphilis contributes to approximately 20% of perinatal deaths. Rates are proportionally higher among Recreational drug use, intravenous drug users, those who are infected with HIV, and men who have sex with men. In the United States about 55,400 people are newly infected each year. In the United States as of 2020, rates of syphilis have increased by more than threefold; in 2018 approximately 86% of all cases of syphilis in the United States were in men. African Americans accounted for almost half of all cases in 2010. As of 2014, syphilis infections continue to increase in the United States.
Syphilis was very common in Europe during the 18th and 19th centuries. Gustave Flaubert, Flaubert found it universal among nineteenth-century Egyptian prostitutes. In the developed world during the early 20th century, infections declined rapidly with the widespread use of antibiotics, until the 1980s and 1990s. Since 2000, rates of syphilis have been increasing in the US, Canada, the UK, Australia and Europe, primarily among men who have sex with men. Rates of syphilis among US women have remained stable during this time, while rates among UK women have increased, but at a rate less than that of men. Increased rates among heterosexuals have occurred in China and Russia since the 1990s. This has been attributed to unsafe sexual practices, such as sexual promiscuity, prostitution, and decreasing use of barrier protection.
Left untreated, it has a mortality rate of 8% to 58%, with a greater death rate among males. The symptoms of syphilis have become less severe over the 19th and 20th centuries, in part due to widespread availability of effective treatment, and partly due to virulence of the bacteria. With early treatment, few complications result. Syphilis increases the risk of HIV transmission by two to five times, and coinfection is common (30–60% in some urban centers). In 2015, Cuba became the first country to eliminate mother-to-child transmission of syphilis.

 There is an outstanding issue, however. Damaged teeth and bones may seem to hold proof of pre-Columbian syphilis, but there is a possibility that they point to an endemic form of the disease instead. As syphilis, bejel, and yaws vary considerably in mortality rates and the level of human disgust they elicit, it is important to know which one is under discussion in any given case, but it remains difficult for paleopathologists to distinguish among them. (The fourth of the treponemal diseases is Pinta (disease), Pinta, a skin disease and therefore unrecoverable through paleopathology.) Ancient DNA (aDNA) holds the answer, because just as only aDNA suffices to distinguish between syphilis and other diseases that produce similar symptoms in the body, it alone can differentiate spirochetes that are 99.8 percent identical with absolute accuracy. Progress on uncovering the historical extent of syndromes through aDNA remains slow, however, because the spirochete responsible for treponematosis is rare in skeletal remains and fragile, making it notoriously difficult to recover and analyze. Precise dating to the medieval period is not yet possible, but work by Kettu Majander et al. uncovering the presence of several different kinds of treponematosis at the beginning of the early modern period argues against its recent introduction from elsewhere. Therefore, they argue, treponematosis—including syphilis—almost certainly existed in medieval Europe.
Despite significant progress in tracing the presence of syphilis in past historic periods, definitive findings from paleopathology and aDNA studies are still lacking for the medieval period. Evidence from art is therefore helpful in settling the issue. Research by Marylynn Salmon has demonstrated that deformities in medieval subjects can be identified by comparing them to those of modern victims of syphilis in medical drawings and photographs. One of the most typical deformities, for example, is a collapsed nasal bridge called saddle nose. Salmon discovered that it appeared often in Illuminated manuscript, medieval illuminations, especially among the men tormenting Christ in scenes of the crucifixion. The association of saddle nose with men perceived to be so evil they would kill the son of God indicates the artists were thinking of syphilis, which is typically transmitted through sexual intercourse with promiscuous partners, a mortal sin in medieval times. One illuminator goes so far as to show a flagellant with an exposed penis, red at the tip as though infected with a syphilitic sore. Others show the deformed teeth associated with congenital syphilis—Hutchinson's teeth, Hutchinson's incisors—or the eye deformity Ptosis (eyelid), ptosis that often appears in victims of the disease.
It remains mysterious why the authors of medieval medical treatises so uniformly refrained from describing syphilis or commenting on its existence in the population. Probably many confused it with other diseases such as leprosy (Leprosy, Hansen's Disease) or elephantiasis. The great variety of symptoms of treponematosis, the different ages at which the various diseases appears, and its widely divergent outcomes depending on climate and culture, would have added greatly to the confusion of medical practitioners, as indeed they did right down to the middle of the twentieth century. In addition, evidence indicates that some writers on disease feared the political implications of discussing a condition more fatal to elites than to commoners. Historian Jon Arrizabalaga has investigated this question for Castile (historical region), Castile with startling results revealing an effort to hide its association with elites.
The first written records of an outbreak of syphilis in Europe occurred in 1495 in Naples, Naples, Italy, during a French invasion (Italian War of 1494–98). Since it was claimed to have been spread by French troops, it was initially called the "French disease" by the people of Naples. The disease reached London in 1497 and was recorded at St Batholomew's Hospital as infected 10 out of the 20 patients. In 1530, the pastoral name "syphilis" (the name of a character) was first used by the Italian physician and poet Girolamo Fracastoro as the title of his Latin poem in dactylic hexameter ''Syphilis sive morbus gallicus'' (''Syphilis or The French Disease'') describing the ravages of the disease in Italy. In Great Britain it was also called the "Great Pox".
In the 16th through 19th centuries, syphilis was one of the largest public health burdens in prevalence, symptoms, and disability, although records of its true prevalence were generally not kept because of the fearsome and sordid status of sexually transmitted infections in those centuries. According to a 2020 study, more than 20% of individuals in the age range 15–34 years in late 18th century London were treated for syphilis. At the time the causative agent was unknown but it was well known that it was spread sexually and also often from mother to child. Its association with sex, especially sexual promiscuity and prostitution, made it an object of fear and revulsion and a taboo. The magnitude of its morbidity and mortality in those centuries reflected that, unlike today, there was no adequate understanding of its pathogenesis and no truly effective treatments. Its damage was caused not so much by great sickness or death early in the course of the disease but rather by its gruesome effects decades after infection as it progressed to neurosyphilis with tabes dorsalis. Mercury (element), Mercury compounds and isolation were commonly used, with treatments often worse than the disease.
The causative organism, ''Treponema pallidum'', was first identified by Fritz Schaudinn and Erich Hoffmann, in 1905. The first effective treatment for syphilis was arsphenamine, discovered by Sahachiro Hata in 1909, during a survey of hundreds of newly synthesized organic arsenical compounds led by Paul Ehrlich. It was manufactured and marketed from 1910 under the trade name Salvarsan by Hoechst AG. This Organoarsenic chemistry, organoarsenic compound was the first modern Antimicrobial chemotherapy, chemotherapeutic agent.
During the 20th century, as both microbiology and pharmacology advanced greatly, syphilis, like many other infectious diseases, became more of a manageable burden than a scary and disfiguring mystery, at least in developed countries among those people who could afford to pay for timely diagnosis and treatment. Penicillin was discovered in 1928, and effectiveness of treatment with penicillin was confirmed in trials in 1943, at which time it became the main treatment.
Many famous historical figures, including Franz Schubert, Arthur Schopenhauer, Édouard Manet, Charles Baudelaire, and Guy de Maupassant are believed to have had the disease. Friedrich Nietzsche was long believed to have gone mad as a result of tertiary syphilis, but that diagnosis has recently come into question.
There is an outstanding issue, however. Damaged teeth and bones may seem to hold proof of pre-Columbian syphilis, but there is a possibility that they point to an endemic form of the disease instead. As syphilis, bejel, and yaws vary considerably in mortality rates and the level of human disgust they elicit, it is important to know which one is under discussion in any given case, but it remains difficult for paleopathologists to distinguish among them. (The fourth of the treponemal diseases is Pinta (disease), Pinta, a skin disease and therefore unrecoverable through paleopathology.) Ancient DNA (aDNA) holds the answer, because just as only aDNA suffices to distinguish between syphilis and other diseases that produce similar symptoms in the body, it alone can differentiate spirochetes that are 99.8 percent identical with absolute accuracy. Progress on uncovering the historical extent of syndromes through aDNA remains slow, however, because the spirochete responsible for treponematosis is rare in skeletal remains and fragile, making it notoriously difficult to recover and analyze. Precise dating to the medieval period is not yet possible, but work by Kettu Majander et al. uncovering the presence of several different kinds of treponematosis at the beginning of the early modern period argues against its recent introduction from elsewhere. Therefore, they argue, treponematosis—including syphilis—almost certainly existed in medieval Europe.
Despite significant progress in tracing the presence of syphilis in past historic periods, definitive findings from paleopathology and aDNA studies are still lacking for the medieval period. Evidence from art is therefore helpful in settling the issue. Research by Marylynn Salmon has demonstrated that deformities in medieval subjects can be identified by comparing them to those of modern victims of syphilis in medical drawings and photographs. One of the most typical deformities, for example, is a collapsed nasal bridge called saddle nose. Salmon discovered that it appeared often in Illuminated manuscript, medieval illuminations, especially among the men tormenting Christ in scenes of the crucifixion. The association of saddle nose with men perceived to be so evil they would kill the son of God indicates the artists were thinking of syphilis, which is typically transmitted through sexual intercourse with promiscuous partners, a mortal sin in medieval times. One illuminator goes so far as to show a flagellant with an exposed penis, red at the tip as though infected with a syphilitic sore. Others show the deformed teeth associated with congenital syphilis—Hutchinson's teeth, Hutchinson's incisors—or the eye deformity Ptosis (eyelid), ptosis that often appears in victims of the disease.
It remains mysterious why the authors of medieval medical treatises so uniformly refrained from describing syphilis or commenting on its existence in the population. Probably many confused it with other diseases such as leprosy (Leprosy, Hansen's Disease) or elephantiasis. The great variety of symptoms of treponematosis, the different ages at which the various diseases appears, and its widely divergent outcomes depending on climate and culture, would have added greatly to the confusion of medical practitioners, as indeed they did right down to the middle of the twentieth century. In addition, evidence indicates that some writers on disease feared the political implications of discussing a condition more fatal to elites than to commoners. Historian Jon Arrizabalaga has investigated this question for Castile (historical region), Castile with startling results revealing an effort to hide its association with elites.
The first written records of an outbreak of syphilis in Europe occurred in 1495 in Naples, Naples, Italy, during a French invasion (Italian War of 1494–98). Since it was claimed to have been spread by French troops, it was initially called the "French disease" by the people of Naples. The disease reached London in 1497 and was recorded at St Batholomew's Hospital as infected 10 out of the 20 patients. In 1530, the pastoral name "syphilis" (the name of a character) was first used by the Italian physician and poet Girolamo Fracastoro as the title of his Latin poem in dactylic hexameter ''Syphilis sive morbus gallicus'' (''Syphilis or The French Disease'') describing the ravages of the disease in Italy. In Great Britain it was also called the "Great Pox".
In the 16th through 19th centuries, syphilis was one of the largest public health burdens in prevalence, symptoms, and disability, although records of its true prevalence were generally not kept because of the fearsome and sordid status of sexually transmitted infections in those centuries. According to a 2020 study, more than 20% of individuals in the age range 15–34 years in late 18th century London were treated for syphilis. At the time the causative agent was unknown but it was well known that it was spread sexually and also often from mother to child. Its association with sex, especially sexual promiscuity and prostitution, made it an object of fear and revulsion and a taboo. The magnitude of its morbidity and mortality in those centuries reflected that, unlike today, there was no adequate understanding of its pathogenesis and no truly effective treatments. Its damage was caused not so much by great sickness or death early in the course of the disease but rather by its gruesome effects decades after infection as it progressed to neurosyphilis with tabes dorsalis. Mercury (element), Mercury compounds and isolation were commonly used, with treatments often worse than the disease.
The causative organism, ''Treponema pallidum'', was first identified by Fritz Schaudinn and Erich Hoffmann, in 1905. The first effective treatment for syphilis was arsphenamine, discovered by Sahachiro Hata in 1909, during a survey of hundreds of newly synthesized organic arsenical compounds led by Paul Ehrlich. It was manufactured and marketed from 1910 under the trade name Salvarsan by Hoechst AG. This Organoarsenic chemistry, organoarsenic compound was the first modern Antimicrobial chemotherapy, chemotherapeutic agent.
During the 20th century, as both microbiology and pharmacology advanced greatly, syphilis, like many other infectious diseases, became more of a manageable burden than a scary and disfiguring mystery, at least in developed countries among those people who could afford to pay for timely diagnosis and treatment. Penicillin was discovered in 1928, and effectiveness of treatment with penicillin was confirmed in trials in 1943, at which time it became the main treatment.
Many famous historical figures, including Franz Schubert, Arthur Schopenhauer, Édouard Manet, Charles Baudelaire, and Guy de Maupassant are believed to have had the disease. Friedrich Nietzsche was long believed to have gone mad as a result of tertiary syphilis, but that diagnosis has recently come into question.
 The earliest known depiction of an individual with syphilis is Albrecht Dürer's ''Syphilitic Man'', a woodcut believed to represent a Landsknecht, a Northern European mercenary. The myth of the ''femme fatale'' or "poison women" of the 19th century is believed to be partly derived from the devastation of syphilis, with classic examples in literature including John Keats' "La Belle Dame sans Merci".
The Flemish artist Stradanus designed a print called ''Preparation and Use of Guayaco for Treating Syphilis'', a scene of a wealthy man receiving treatment for syphilis with the tropical wood guaiacum sometime around 1590.
The earliest known depiction of an individual with syphilis is Albrecht Dürer's ''Syphilitic Man'', a woodcut believed to represent a Landsknecht, a Northern European mercenary. The myth of the ''femme fatale'' or "poison women" of the 19th century is believed to be partly derived from the devastation of syphilis, with classic examples in literature including John Keats' "La Belle Dame sans Merci".
The Flemish artist Stradanus designed a print called ''Preparation and Use of Guayaco for Treating Syphilis'', a scene of a wealthy man receiving treatment for syphilis with the tropical wood guaiacum sometime around 1590.
 The "Tuskegee Study of Untreated Syphilis in the Negro Male" was an infamous, unethical and racist clinical trial, clinical study conducted between 1932 and 1972 by the U.S. Public Health Service. Whereas the purpose of this study was to observe the Natural history of disease, natural history of untreated syphilis; the African-American men in the study were told they were receiving free treatment for "bad blood" from the United States government.
The Public Health Service started working on this study in 1932 in collaboration with Tuskegee University, a historically black college in Alabama. Researchers enrolled 600 poor, African-American sharecroppers from Macon County, Alabama, Macon County, Alabama in the study. Of these men, 399 had contracted syphilis before the study began, and 201 did not have the disease. Medical care, hot meals and free burial insurance were given to those who participated. The men were told that the study would last six months, but in the end it continued for 40 years. After funding for treatment was lost, the study was continued without informing the men that they were only being studied and would not be treated. Facing insufficient participation, the Macon County Health Department nevertheless wrote to subjects to offer them a "last chance" to get a special "treatment", which was not a treatment at all, but a spinal tap administered exclusively for diagnostic purposes. None of the men infected were ever told that they had the disease, and none were treated with penicillin even after the antibiotic had been proven to successfully treat syphilis. According to the Centers for Disease Control, the men were told they were being treated for "bad blood"—a colloquialism describing various conditions such as fatigue, anemia and syphilis—which was a leading cause of death among southern African-American men.
The 40-year study became a textbook example of poor medical ethics because researchers had knowingly withheld treatment with penicillin and because the subjects had been misled concerning the purposes of the study. The revelation in 1972 of these study failures by a whistleblower, Peter Buxtun, led to major changes in U.S. law and regulation on the protection of participants in clinical studies. Now studies require informed consent, communication of diagnosis, and accurate reporting of test results.
Similar experiments were carried out in Guatemala from 1946 to 1948. It was done during the administration of American President Harry S. Truman and Guatemalan President Juan José Arévalo with the cooperation of some Guatemalan health ministries and officials. Doctors infected soldiers, prostitutes, prisoners and mental patients with syphilis and other sexually transmitted infections, without the informed consent of the subjects, and treated most subjects with antibiotics. The experiment resulted in at least 83 deaths. In October 2010, the U.S. formally apologized to Guatemala for the ethical violations that took place. Secretary of State Hillary Clinton and Health and Human Services Secretary Kathleen Sebelius stated "Although these events occurred more than 64 years ago, we are outraged that such reprehensible research could have occurred under the guise of public health. We deeply regret that it happened, and we apologize to all the individuals who were affected by such abhorrent research practices." The experiments were led by physician John Charles Cutler who also participated in the late stages of the Tuskegee syphilis experiment.
The "Tuskegee Study of Untreated Syphilis in the Negro Male" was an infamous, unethical and racist clinical trial, clinical study conducted between 1932 and 1972 by the U.S. Public Health Service. Whereas the purpose of this study was to observe the Natural history of disease, natural history of untreated syphilis; the African-American men in the study were told they were receiving free treatment for "bad blood" from the United States government.
The Public Health Service started working on this study in 1932 in collaboration with Tuskegee University, a historically black college in Alabama. Researchers enrolled 600 poor, African-American sharecroppers from Macon County, Alabama, Macon County, Alabama in the study. Of these men, 399 had contracted syphilis before the study began, and 201 did not have the disease. Medical care, hot meals and free burial insurance were given to those who participated. The men were told that the study would last six months, but in the end it continued for 40 years. After funding for treatment was lost, the study was continued without informing the men that they were only being studied and would not be treated. Facing insufficient participation, the Macon County Health Department nevertheless wrote to subjects to offer them a "last chance" to get a special "treatment", which was not a treatment at all, but a spinal tap administered exclusively for diagnostic purposes. None of the men infected were ever told that they had the disease, and none were treated with penicillin even after the antibiotic had been proven to successfully treat syphilis. According to the Centers for Disease Control, the men were told they were being treated for "bad blood"—a colloquialism describing various conditions such as fatigue, anemia and syphilis—which was a leading cause of death among southern African-American men.
The 40-year study became a textbook example of poor medical ethics because researchers had knowingly withheld treatment with penicillin and because the subjects had been misled concerning the purposes of the study. The revelation in 1972 of these study failures by a whistleblower, Peter Buxtun, led to major changes in U.S. law and regulation on the protection of participants in clinical studies. Now studies require informed consent, communication of diagnosis, and accurate reporting of test results.
Similar experiments were carried out in Guatemala from 1946 to 1948. It was done during the administration of American President Harry S. Truman and Guatemalan President Juan José Arévalo with the cooperation of some Guatemalan health ministries and officials. Doctors infected soldiers, prostitutes, prisoners and mental patients with syphilis and other sexually transmitted infections, without the informed consent of the subjects, and treated most subjects with antibiotics. The experiment resulted in at least 83 deaths. In October 2010, the U.S. formally apologized to Guatemala for the ethical violations that took place. Secretary of State Hillary Clinton and Health and Human Services Secretary Kathleen Sebelius stated "Although these events occurred more than 64 years ago, we are outraged that such reprehensible research could have occurred under the guise of public health. We deeply regret that it happened, and we apologize to all the individuals who were affected by such abhorrent research practices." The experiments were led by physician John Charles Cutler who also participated in the late stages of the Tuskegee syphilis experiment.
"Syphilis - CDC Fact Sheet"
Centers for Disease Control and Prevention (CDC)
UCSF HIV InSite Knowledge Base Chapter: Syphilis and HIV
Recommendations for Public Health Surveillance of Syphilis in the United States
* {{Authority control Syphilis, Bacterial diseases Bacterium-related cutaneous conditions Infectious diseases Infectious diseases with eradication efforts Infections with a predominantly sexual mode of transmission Sexually transmitted diseases and infections Spirochaetes Wikipedia medicine articles ready to translate (full) Wikipedia infectious disease articles ready to translate
Signs and symptoms
Syphilis can Presentation (medical), present in one of four different stages: primary, secondary, latent, and tertiary, and may also occur congenitally. It was referred to as "the great imitator" by Sir William Osler due to its varied presentations.Primary
Primary syphilis is typically acquired by direct sexual contact with the infectious lesions of another person. Approximately 2–6 weeks after contact (with a range of 10–90 days) a skin lesion, called a chancre, appears at the site and this contains infectious spirochetes. This is classically (40% of the time) a single, firm, painless, non-itchy skin ulceration with a clean base and sharp borders approximately 0.3–3.0 cm in size. The lesion may take on almost any form. In the classic form, it evolves from a macule to a papule and finally to an erosion (dermatopathology)#Primary lesions, erosion or ulcer (dermatology), ulcer. Occasionally, multiple lesions may be present (~40%), with multiple lesions being more common when coinfected with HIV. Lesions may be painful or tender (30%), and they may occur in places other than the genitals (2–7%). The most common location in women is the cervix (44%), the Human penis, penis in heterosexual men (99%), and Human anus, anally and rectally in men who have sex with men (34%). Lymphadenopathy, Lymph node enlargement frequently (80%) occurs around the area of infection, occurring seven to 10 days after chancre formation. The lesion may persist for three to six weeks if left untreated.Secondary
image:2ndsyphil2.jpg, upright=1.4, Reddish papules and nodule (dermatology)#Primary lesions, nodules over much of the body due to secondary syphilis Secondary syphilis occurs approximately four to ten weeks after the primary infection. While secondary disease is known for the many different ways it can manifest, symptoms most commonly involve the skin, mucous membranes, and lymph nodes. There may be a symmetrical, reddish-pink, non-itchy rash on the trunk and extremities, including the palms and soles. The rash may become maculopapular or abscess, pustular. It may form flat, broad, whitish, wart-like lesions on mucous membranes, known as condyloma latum. All of these lesions harbor bacteria and are infectious. Other symptoms may include fever, sore throat, malaise, weight loss, hair loss, and headache. Rare manifestations include hepatitis, liver inflammation, kidney disease, arthritis, joint inflammation, periostitis, optic neuritis, inflammation of the optic nerve, uveitis, and interstitial keratitis. The acute symptoms usually resolve after three to six weeks; about 25% of people may present with a recurrence of secondary symptoms. Many people who present with secondary syphilis (40–85% of women, 20–65% of men) do not report previously having had the classical chancre of primary syphilis.Latent
Latent syphilis is defined as having serology, serologic proof of infection without symptoms of disease. It develops after secondary syphilis and is divided into early latent and late latent stages. Early latent syphilis is defined by the World Health Organization as less than 2 years after original infection. Early latent syphilis is infectious as up to 25% of people can develop a recurrent secondary infection (during which spirochetes are actively replicating and are infectious). Two years after the original infection the person will enter late latent syphilis and is not as infectious as the early phase. The latent phase of syphilis can last many years after which, without treatment, approximately 15-40% of people can develop tertiary syphilis.Tertiary
Congenital
Congenital syphilis is that which is transmitted during pregnancy or during birth. Two-thirds of syphilitic infants are born without symptoms. Common symptoms that develop over the first couple of years of life include hepatosplenomegaly, enlargement of the liver and spleen (70%), rash (70%), fever (40%), neurosyphilis (20%), and pneumonitis, lung inflammation (20%). If untreated, late congenital syphilis may occur in 40%, including saddle nose deformation, Higouménakis' sign, saber shin, or Clutton's joints among others. Infection during pregnancy is also associated with miscarriage. The three main dental defects in congenital syphilis are Hutchinson's incisors (screwdriver shaped incisors), Moon's molars or bud molars, and Fournier's molars or mulberry molars (molars with abnormal occlusal anatomy resembling a mulberry).Cause
Bacteriology
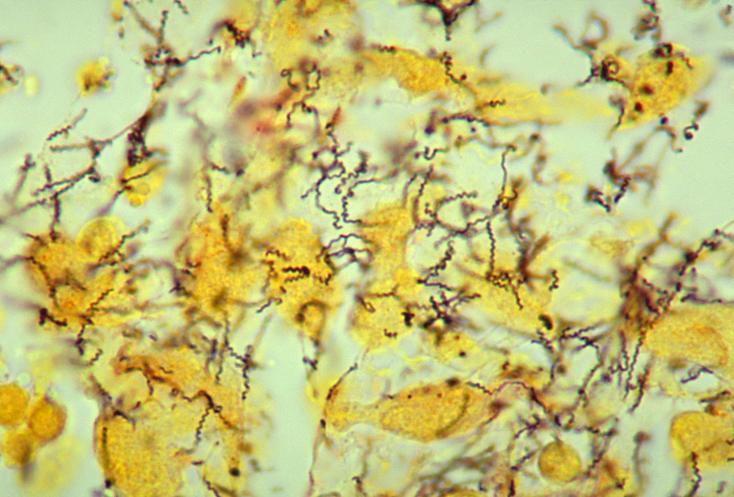 ''Treponema pallidum'' subspecies'' pallidum'' is a spiral-shaped, Gram-negative, highly mobile bacterium. Three other human diseases are caused by related ''Treponema pallidum'' subspecies, including yaws (subspecies ''pertenue''), Pinta (disease), pinta (subspecies ''carateum'') and nonvenereal endemic syphilis, bejel (subspecies ''endemicum''). Unlike subspecies ''pallidum'', they do not cause neurological disease. Humans are the only known natural reservoir for subspecies ''pallidum''. It is unable to survive more than a few days without a Host (biology), host. This is due to its small genome (1.14base pair, Mbp) failing to encode the metabolic pathways necessary to make most of its macronutrients. It has a slow doubling time of greater than 30 hours. The bacterium is known for its ability to evade the immune system and its invasiveness.
''Treponema pallidum'' subspecies'' pallidum'' is a spiral-shaped, Gram-negative, highly mobile bacterium. Three other human diseases are caused by related ''Treponema pallidum'' subspecies, including yaws (subspecies ''pertenue''), Pinta (disease), pinta (subspecies ''carateum'') and nonvenereal endemic syphilis, bejel (subspecies ''endemicum''). Unlike subspecies ''pallidum'', they do not cause neurological disease. Humans are the only known natural reservoir for subspecies ''pallidum''. It is unable to survive more than a few days without a Host (biology), host. This is due to its small genome (1.14base pair, Mbp) failing to encode the metabolic pathways necessary to make most of its macronutrients. It has a slow doubling time of greater than 30 hours. The bacterium is known for its ability to evade the immune system and its invasiveness.
Transmission
Syphilis is transmitted primarily by sexual contact or during pregnancy from a mother to her baby; the spirochete is able to pass through intact mucous membranes or compromised skin. It is thus transmissible by kissing near a lesion, as well as Oral sex, oral, Vaginal sex, vaginal, and anal sex. Approximately 30% to 60% of those exposed to primary or secondary syphilis will get the disease. Its infectivity is exemplified by the fact that an individual Inoculation, inoculated with only 57 organisms has a 50% chance of being infected. Most new cases in the United States (60%) occur in men who have sex with men; and in this population 20% of syphilis cases were due to oral sex alone. Syphilis can be transmitted by blood products, but the risk is low due to screening of Blood donation, donated blood in many countries. The risk of transmission from sharing needles appears to be limited. It is not generally possible to contract syphilis through toilet seats, daily activities, hot tubs, or sharing eating utensils or clothing. This is mainly because the bacteria die very quickly outside of the body, making transmission by fomite, objects extremely difficult.Diagnosis
 Syphilis is difficult to diagnose clinically during early infection. Confirmation is either via blood tests or direct visual inspection using Dark-field microscopy, dark field microscopy. Blood tests are more commonly used, as they are easier to perform. Diagnostic tests are unable to distinguish between the stages of the disease.
Syphilis is difficult to diagnose clinically during early infection. Confirmation is either via blood tests or direct visual inspection using Dark-field microscopy, dark field microscopy. Blood tests are more commonly used, as they are easier to perform. Diagnostic tests are unable to distinguish between the stages of the disease.
Blood tests
Blood tests are divided into Nontreponemal tests for syphilis, nontreponemal and treponemal tests. Nontreponemal tests are used initially, and include venereal disease research laboratory (VDRL) and rapid plasma reagin (RPR) tests. False positive#Type I error, False positives on the nontreponemal tests can occur with some viral infections, such as varicella (chickenpox) and measles. False positives can also occur with lymphoma, tuberculosis, malaria, endocarditis, connective tissue disease, and pregnancy. Because of the possibility of false positives with nontreponemal tests, confirmation is required with a treponemal test, such as treponemal pallidum particle agglutination (TPHA) or fluorescent treponemal antibody absorption test (FTA-Abs). Treponemal antibody tests usually become positive two to five weeks after the initial infection. Neurosyphilis is diagnosed by finding high numbers of leukocytes (predominately lymphocytes) and high protein levels in the cerebrospinal fluid in the setting of a known syphilis infection.Direct testing
Dark field microscopy of serous fluid from a chancre may be used to make an immediate diagnosis. Hospitals do not always have equipment or experienced staff members, and testing must be done within 10 minutes of acquiring the sample. Two other tests can be carried out on a sample from the chancre: direct fluorescent antibody (DFA) and polymerase chain reaction (PCR) tests. DFA uses antibodies tagged with fluorescein, which attach to specific syphilis proteins, while PCR uses techniques to detect the presence of specific syphilis genes. These tests are not as time-sensitive, as they do not require living bacteria to make the diagnosis.Prevention
Vaccine
, there is no vaccine effective for prevention. Several vaccines based on treponemal proteins reduce lesion development in an animal model but research continues.Sex
Condom use reduces the likelihood of transmission during sex, but does not eliminate the risk. The Centers for Disease Control and Prevention (CDC) states, "Correct and consistent use of latex condoms can reduce the risk of syphilis only when the infected area or site of potential exposure is protected. However, a syphilis sore outside of the area covered by a latex condom can still allow transmission, so caution should be exercised even when using a condom." Abstinence from intimate physical contact with an infected person is effective at reducing the transmission of syphilis. The CDC states, "The surest way to avoid transmission of sexually transmitted diseases, including syphilis, is to abstain from sexual contact or to be in a long-term mutually monogamous relationship with a partner who has been tested and is known to be uninfected."Congenital disease
Congenital syphilis in the newborn can be prevented by screening mothers during early pregnancy and treating those who are infected. The United States Preventive Services Task Force (USPSTF) strongly recommends universal screening of all pregnant women, while the World Health Organization (WHO) recommends all women be tested at their first antenatal visit and again in the third trimester. If they are positive, it is recommended their partners also be treated. Congenital syphilis is still common in the developing world, as many women do not receive antenatal care at all, and the antenatal care others receive does not include screening. It still occasionally occurs in the developed world, as those most likely to acquire syphilis are least likely to receive care during pregnancy. Several measures to increase access to testing appear effective at reducing rates of congenital syphilis in low- to middle-income countries. Point-of-care testing to detect syphilis appeared to be reliable although more research is needed to assess its effectiveness and into improving outcomes in mothers and babies.Screening
The CDC recommends that sexually active men who have sex with men be tested at least yearly. The USPSTF also recommends screening among those at high risk. Syphilis is a notifiable disease in many countries, including Canada, the European Union, and the United States. This means health care providers are required to notify public health authorities, which will then ideally provide partner notification to the person's partners. Physicians may also encourage patients to send their partners to seek care. Several strategies have been found to improve follow-up for STI testing, including email and text messaging of reminders for appointments.Treatment
As a form of chemotherapy, elemental mercury was frequently used to treat syphilis in Europe very early on in the epidemic, and in this respect was rather effective. Mercury is highly anti-microbial, and in the early stages of infection was sometimes sufficient in halting development of the disease when applied to cankers or other wounds. Once the bacterium gained a strong foothold, however, the amounts and forms of mercury necessary to control its development exceeded the human ability to endure this extremely toxic metal, and the treatment became worse and more lethal than the disease. Medically directed mercury poisoning also became widespread, and thousands died in desperate attempts to rid themselves of the excruciating, disfiguring, and humiliating illness.Early infections
The first-line treatment for uncomplicated syphilis (primary or secondary stages) remains a single dose of Intramuscular injection, intramuscular benzathine benzylpenicillin. Doxycycline and tetracycline are alternative choices for those allergic to penicillin; due to the risk of birth defects, these are not recommended for pregnant women. Antibiotic resistance, Resistance to macrolides, rifampicin, and clindamycin is often present. Ceftriaxone, a third-generation cephalosporin antibiotic, may be as effective as penicillin-based treatment. It is recommended that a treated person avoid sex until the sores are healed.Late infections
For neurosyphilis, due to the poor penetration of benzathine penicillin into the central nervous system, those affected are given large doses of Intravenous therapy, intravenous penicillin G for a minimum of 10 days. If a person is allergic to penicillin, ceftriaxone may be used or penicillin desensitization attempted. Other late presentations may be treated with once-weekly intramuscular benzathine penicillin for three weeks. Treatment at this stage solely limits further progression of the disease and has a limited effect on damage which has already occurred. Serologic cure can be measured when the non-treponemal titers decline by a factor of 4 or more in 6–12 months in early syphilis or 12–24 months in late syphilis.Jarisch–Herxheimer reaction
 One of the potential side effects of treatment is the Jarisch–Herxheimer reaction. It frequently starts within one hour and lasts for 24 hours, with symptoms of fever, muscle pains, headache, and a tachycardia, fast heart rate. It is caused by cytokines released by the immune system in response to lipoproteins released from rupturing syphilis bacteria.
One of the potential side effects of treatment is the Jarisch–Herxheimer reaction. It frequently starts within one hour and lasts for 24 hours, with symptoms of fever, muscle pains, headache, and a tachycardia, fast heart rate. It is caused by cytokines released by the immune system in response to lipoproteins released from rupturing syphilis bacteria.
Pregnancy
Penicillin is an effective treatment for syphilis in pregnancy but there is no agreement on which dose or route of delivery is most effective.Epidemiology
History
Paleopathology, Paleopatholgists have known for decades that syphilis was present in the Americas before European contact. The situation in Europe and Afro-Eurasia has been murkier and caused considerable debate. According to the Columbian theory, syphilis was brought to Spain by the men who sailed with Christopher Columbus in 1492 and spread from there, with a serious epidemic in Naples beginning as early as 1495. Contemporaries believed the disease sprang from American roots, and in the sixteenth century physicians wrote extensively about the new disease inflicted on them by the returning explorers. Most historians and paleopathologists initially accepted the Columbian theory, but over several decades beginning in the 1960s examples of probable treponematosis—the parent disease of syphilis, Nonvenereal endemic syphilis, bejel, and yaws—in skeletal remains have shifted opinion. As a result the pre-Columbian hypothesis is now more widely accepted. It argues that treponemal disease in the form of bejel and yaws was a common childhood ailment in Europe and Afro-Eurasia beginning in ancient times. Largely benign if still unpleasant, infections occurred among the young, transmitted via shared drinking vessels or bedding with only a small viral load. In adulthood, people infected as children had a certain degree of immunity that prevented serious symptoms upon reinfection. Once living conditions began to change with urbanization, however, and certain more elite social groups separated themselves from their inferiors and regularly practiced better hygiene, treponematosis was driven out of the age group in which it had become endemic. It then began to appear in adults as syphilis. Because they had never been exposed as children, they were not able to fend off serious illness. Spreading the disease via sexual contact also led to victims being infected with a massive viral load from open sores on the genitalia. Adults in higher socioeconomic groups then became very sick with painful and debilitating symptoms lasting for decades. Often they died of the disease, as did their children who were infected with congenital syphilis. The difference between rural and urban populations was first noted by Ellis Herndon Hudson, a clinician who published extensively about the prevalence of treponematosis, including syphilis, in times past. The importance of viral load was first noted by the physician Ernest Grin in 1952 in his study of syphilis in Bosnia. The most compelling evidence for the validity of the pre-Columbian hypothesis is the presence of syphilitic-like damage to bones and teeth in medieval skeletal remains. While the absolute number of cases is not large, they keep turning up, most recently in 2015. In 2020, a group of leading paleopathologists concluded that enough evidence had been collected to prove that treponemal disease, almost certainly including syphilis, had existed in Europe prior to the voyages of Columbus. At least fifteen cases of acquired treponematosis based on evidence from bones, and six examples of congenital treponematosis based on evidence from teeth, are now widely accepted. In several of the twenty-one cases the evidence may also indicate syphilis.
 There is an outstanding issue, however. Damaged teeth and bones may seem to hold proof of pre-Columbian syphilis, but there is a possibility that they point to an endemic form of the disease instead. As syphilis, bejel, and yaws vary considerably in mortality rates and the level of human disgust they elicit, it is important to know which one is under discussion in any given case, but it remains difficult for paleopathologists to distinguish among them. (The fourth of the treponemal diseases is Pinta (disease), Pinta, a skin disease and therefore unrecoverable through paleopathology.) Ancient DNA (aDNA) holds the answer, because just as only aDNA suffices to distinguish between syphilis and other diseases that produce similar symptoms in the body, it alone can differentiate spirochetes that are 99.8 percent identical with absolute accuracy. Progress on uncovering the historical extent of syndromes through aDNA remains slow, however, because the spirochete responsible for treponematosis is rare in skeletal remains and fragile, making it notoriously difficult to recover and analyze. Precise dating to the medieval period is not yet possible, but work by Kettu Majander et al. uncovering the presence of several different kinds of treponematosis at the beginning of the early modern period argues against its recent introduction from elsewhere. Therefore, they argue, treponematosis—including syphilis—almost certainly existed in medieval Europe.
Despite significant progress in tracing the presence of syphilis in past historic periods, definitive findings from paleopathology and aDNA studies are still lacking for the medieval period. Evidence from art is therefore helpful in settling the issue. Research by Marylynn Salmon has demonstrated that deformities in medieval subjects can be identified by comparing them to those of modern victims of syphilis in medical drawings and photographs. One of the most typical deformities, for example, is a collapsed nasal bridge called saddle nose. Salmon discovered that it appeared often in Illuminated manuscript, medieval illuminations, especially among the men tormenting Christ in scenes of the crucifixion. The association of saddle nose with men perceived to be so evil they would kill the son of God indicates the artists were thinking of syphilis, which is typically transmitted through sexual intercourse with promiscuous partners, a mortal sin in medieval times. One illuminator goes so far as to show a flagellant with an exposed penis, red at the tip as though infected with a syphilitic sore. Others show the deformed teeth associated with congenital syphilis—Hutchinson's teeth, Hutchinson's incisors—or the eye deformity Ptosis (eyelid), ptosis that often appears in victims of the disease.
It remains mysterious why the authors of medieval medical treatises so uniformly refrained from describing syphilis or commenting on its existence in the population. Probably many confused it with other diseases such as leprosy (Leprosy, Hansen's Disease) or elephantiasis. The great variety of symptoms of treponematosis, the different ages at which the various diseases appears, and its widely divergent outcomes depending on climate and culture, would have added greatly to the confusion of medical practitioners, as indeed they did right down to the middle of the twentieth century. In addition, evidence indicates that some writers on disease feared the political implications of discussing a condition more fatal to elites than to commoners. Historian Jon Arrizabalaga has investigated this question for Castile (historical region), Castile with startling results revealing an effort to hide its association with elites.
The first written records of an outbreak of syphilis in Europe occurred in 1495 in Naples, Naples, Italy, during a French invasion (Italian War of 1494–98). Since it was claimed to have been spread by French troops, it was initially called the "French disease" by the people of Naples. The disease reached London in 1497 and was recorded at St Batholomew's Hospital as infected 10 out of the 20 patients. In 1530, the pastoral name "syphilis" (the name of a character) was first used by the Italian physician and poet Girolamo Fracastoro as the title of his Latin poem in dactylic hexameter ''Syphilis sive morbus gallicus'' (''Syphilis or The French Disease'') describing the ravages of the disease in Italy. In Great Britain it was also called the "Great Pox".
In the 16th through 19th centuries, syphilis was one of the largest public health burdens in prevalence, symptoms, and disability, although records of its true prevalence were generally not kept because of the fearsome and sordid status of sexually transmitted infections in those centuries. According to a 2020 study, more than 20% of individuals in the age range 15–34 years in late 18th century London were treated for syphilis. At the time the causative agent was unknown but it was well known that it was spread sexually and also often from mother to child. Its association with sex, especially sexual promiscuity and prostitution, made it an object of fear and revulsion and a taboo. The magnitude of its morbidity and mortality in those centuries reflected that, unlike today, there was no adequate understanding of its pathogenesis and no truly effective treatments. Its damage was caused not so much by great sickness or death early in the course of the disease but rather by its gruesome effects decades after infection as it progressed to neurosyphilis with tabes dorsalis. Mercury (element), Mercury compounds and isolation were commonly used, with treatments often worse than the disease.
The causative organism, ''Treponema pallidum'', was first identified by Fritz Schaudinn and Erich Hoffmann, in 1905. The first effective treatment for syphilis was arsphenamine, discovered by Sahachiro Hata in 1909, during a survey of hundreds of newly synthesized organic arsenical compounds led by Paul Ehrlich. It was manufactured and marketed from 1910 under the trade name Salvarsan by Hoechst AG. This Organoarsenic chemistry, organoarsenic compound was the first modern Antimicrobial chemotherapy, chemotherapeutic agent.
During the 20th century, as both microbiology and pharmacology advanced greatly, syphilis, like many other infectious diseases, became more of a manageable burden than a scary and disfiguring mystery, at least in developed countries among those people who could afford to pay for timely diagnosis and treatment. Penicillin was discovered in 1928, and effectiveness of treatment with penicillin was confirmed in trials in 1943, at which time it became the main treatment.
Many famous historical figures, including Franz Schubert, Arthur Schopenhauer, Édouard Manet, Charles Baudelaire, and Guy de Maupassant are believed to have had the disease. Friedrich Nietzsche was long believed to have gone mad as a result of tertiary syphilis, but that diagnosis has recently come into question.
There is an outstanding issue, however. Damaged teeth and bones may seem to hold proof of pre-Columbian syphilis, but there is a possibility that they point to an endemic form of the disease instead. As syphilis, bejel, and yaws vary considerably in mortality rates and the level of human disgust they elicit, it is important to know which one is under discussion in any given case, but it remains difficult for paleopathologists to distinguish among them. (The fourth of the treponemal diseases is Pinta (disease), Pinta, a skin disease and therefore unrecoverable through paleopathology.) Ancient DNA (aDNA) holds the answer, because just as only aDNA suffices to distinguish between syphilis and other diseases that produce similar symptoms in the body, it alone can differentiate spirochetes that are 99.8 percent identical with absolute accuracy. Progress on uncovering the historical extent of syndromes through aDNA remains slow, however, because the spirochete responsible for treponematosis is rare in skeletal remains and fragile, making it notoriously difficult to recover and analyze. Precise dating to the medieval period is not yet possible, but work by Kettu Majander et al. uncovering the presence of several different kinds of treponematosis at the beginning of the early modern period argues against its recent introduction from elsewhere. Therefore, they argue, treponematosis—including syphilis—almost certainly existed in medieval Europe.
Despite significant progress in tracing the presence of syphilis in past historic periods, definitive findings from paleopathology and aDNA studies are still lacking for the medieval period. Evidence from art is therefore helpful in settling the issue. Research by Marylynn Salmon has demonstrated that deformities in medieval subjects can be identified by comparing them to those of modern victims of syphilis in medical drawings and photographs. One of the most typical deformities, for example, is a collapsed nasal bridge called saddle nose. Salmon discovered that it appeared often in Illuminated manuscript, medieval illuminations, especially among the men tormenting Christ in scenes of the crucifixion. The association of saddle nose with men perceived to be so evil they would kill the son of God indicates the artists were thinking of syphilis, which is typically transmitted through sexual intercourse with promiscuous partners, a mortal sin in medieval times. One illuminator goes so far as to show a flagellant with an exposed penis, red at the tip as though infected with a syphilitic sore. Others show the deformed teeth associated with congenital syphilis—Hutchinson's teeth, Hutchinson's incisors—or the eye deformity Ptosis (eyelid), ptosis that often appears in victims of the disease.
It remains mysterious why the authors of medieval medical treatises so uniformly refrained from describing syphilis or commenting on its existence in the population. Probably many confused it with other diseases such as leprosy (Leprosy, Hansen's Disease) or elephantiasis. The great variety of symptoms of treponematosis, the different ages at which the various diseases appears, and its widely divergent outcomes depending on climate and culture, would have added greatly to the confusion of medical practitioners, as indeed they did right down to the middle of the twentieth century. In addition, evidence indicates that some writers on disease feared the political implications of discussing a condition more fatal to elites than to commoners. Historian Jon Arrizabalaga has investigated this question for Castile (historical region), Castile with startling results revealing an effort to hide its association with elites.
The first written records of an outbreak of syphilis in Europe occurred in 1495 in Naples, Naples, Italy, during a French invasion (Italian War of 1494–98). Since it was claimed to have been spread by French troops, it was initially called the "French disease" by the people of Naples. The disease reached London in 1497 and was recorded at St Batholomew's Hospital as infected 10 out of the 20 patients. In 1530, the pastoral name "syphilis" (the name of a character) was first used by the Italian physician and poet Girolamo Fracastoro as the title of his Latin poem in dactylic hexameter ''Syphilis sive morbus gallicus'' (''Syphilis or The French Disease'') describing the ravages of the disease in Italy. In Great Britain it was also called the "Great Pox".
In the 16th through 19th centuries, syphilis was one of the largest public health burdens in prevalence, symptoms, and disability, although records of its true prevalence were generally not kept because of the fearsome and sordid status of sexually transmitted infections in those centuries. According to a 2020 study, more than 20% of individuals in the age range 15–34 years in late 18th century London were treated for syphilis. At the time the causative agent was unknown but it was well known that it was spread sexually and also often from mother to child. Its association with sex, especially sexual promiscuity and prostitution, made it an object of fear and revulsion and a taboo. The magnitude of its morbidity and mortality in those centuries reflected that, unlike today, there was no adequate understanding of its pathogenesis and no truly effective treatments. Its damage was caused not so much by great sickness or death early in the course of the disease but rather by its gruesome effects decades after infection as it progressed to neurosyphilis with tabes dorsalis. Mercury (element), Mercury compounds and isolation were commonly used, with treatments often worse than the disease.
The causative organism, ''Treponema pallidum'', was first identified by Fritz Schaudinn and Erich Hoffmann, in 1905. The first effective treatment for syphilis was arsphenamine, discovered by Sahachiro Hata in 1909, during a survey of hundreds of newly synthesized organic arsenical compounds led by Paul Ehrlich. It was manufactured and marketed from 1910 under the trade name Salvarsan by Hoechst AG. This Organoarsenic chemistry, organoarsenic compound was the first modern Antimicrobial chemotherapy, chemotherapeutic agent.
During the 20th century, as both microbiology and pharmacology advanced greatly, syphilis, like many other infectious diseases, became more of a manageable burden than a scary and disfiguring mystery, at least in developed countries among those people who could afford to pay for timely diagnosis and treatment. Penicillin was discovered in 1928, and effectiveness of treatment with penicillin was confirmed in trials in 1943, at which time it became the main treatment.
Many famous historical figures, including Franz Schubert, Arthur Schopenhauer, Édouard Manet, Charles Baudelaire, and Guy de Maupassant are believed to have had the disease. Friedrich Nietzsche was long believed to have gone mad as a result of tertiary syphilis, but that diagnosis has recently come into question.
Arts and literature
 The earliest known depiction of an individual with syphilis is Albrecht Dürer's ''Syphilitic Man'', a woodcut believed to represent a Landsknecht, a Northern European mercenary. The myth of the ''femme fatale'' or "poison women" of the 19th century is believed to be partly derived from the devastation of syphilis, with classic examples in literature including John Keats' "La Belle Dame sans Merci".
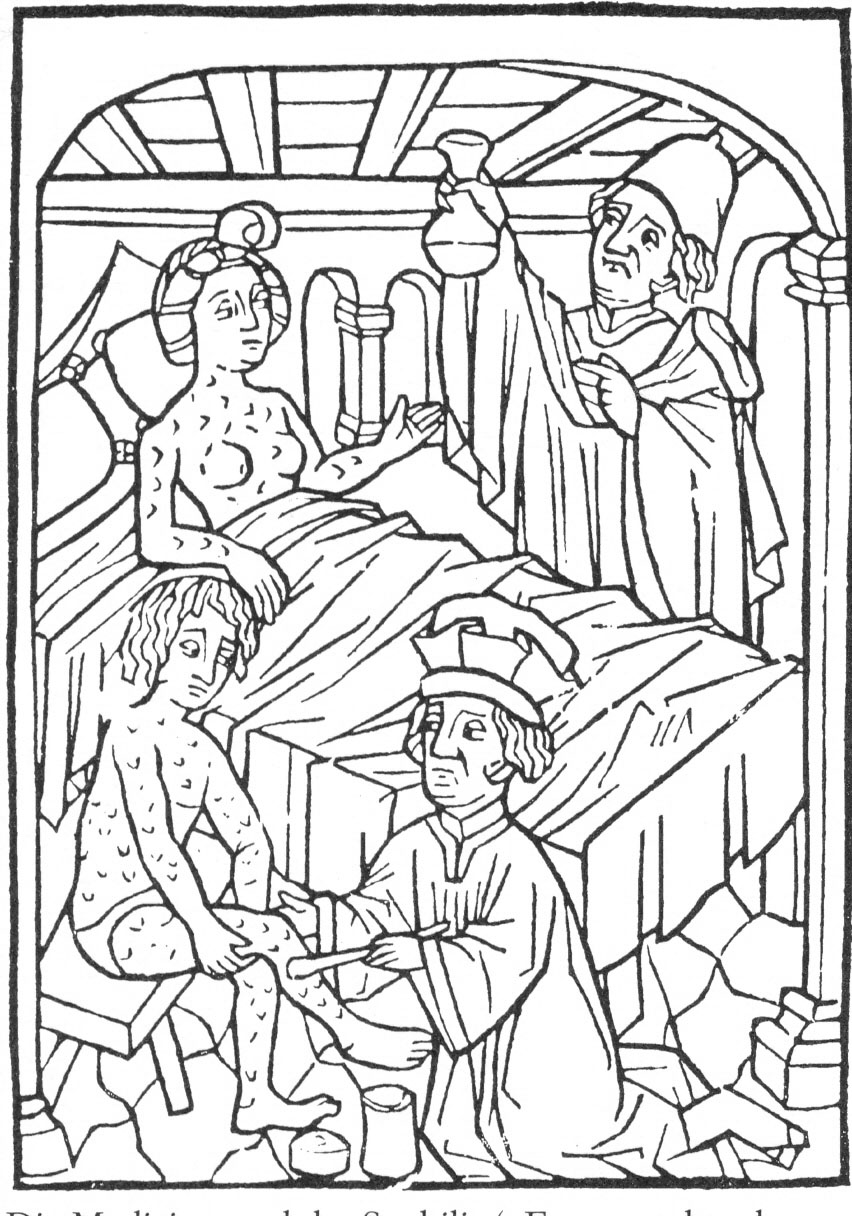
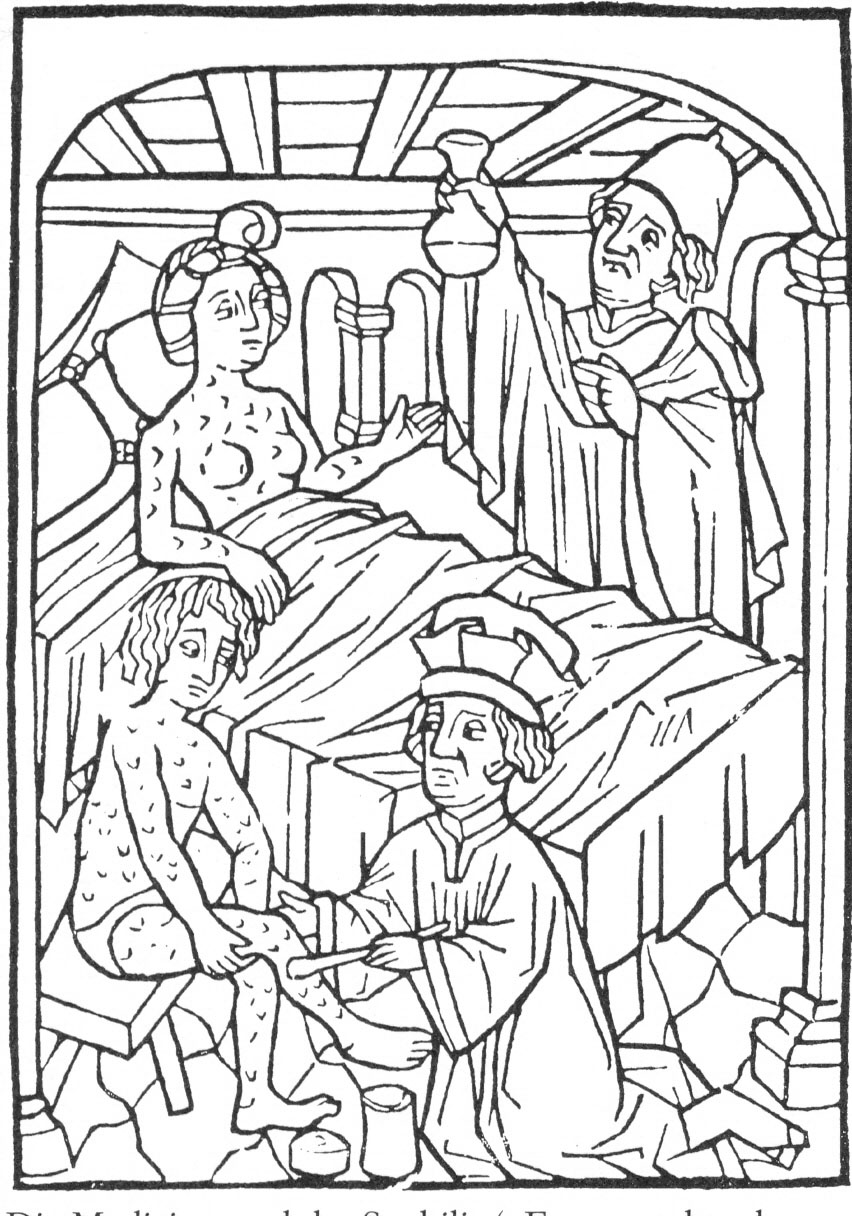
The Flemish artist Stradanus designed a print called ''Preparation and Use of Guayaco for Treating Syphilis'', a scene of a wealthy man receiving treatment for syphilis with the tropical wood guaiacum sometime around 1590.
The earliest known depiction of an individual with syphilis is Albrecht Dürer's ''Syphilitic Man'', a woodcut believed to represent a Landsknecht, a Northern European mercenary. The myth of the ''femme fatale'' or "poison women" of the 19th century is believed to be partly derived from the devastation of syphilis, with classic examples in literature including John Keats' "La Belle Dame sans Merci".
The Flemish artist Stradanus designed a print called ''Preparation and Use of Guayaco for Treating Syphilis'', a scene of a wealthy man receiving treatment for syphilis with the tropical wood guaiacum sometime around 1590.
Tuskegee and Guatemala studies
 The "Tuskegee Study of Untreated Syphilis in the Negro Male" was an infamous, unethical and racist clinical trial, clinical study conducted between 1932 and 1972 by the U.S. Public Health Service. Whereas the purpose of this study was to observe the Natural history of disease, natural history of untreated syphilis; the African-American men in the study were told they were receiving free treatment for "bad blood" from the United States government.
The Public Health Service started working on this study in 1932 in collaboration with Tuskegee University, a historically black college in Alabama. Researchers enrolled 600 poor, African-American sharecroppers from Macon County, Alabama, Macon County, Alabama in the study. Of these men, 399 had contracted syphilis before the study began, and 201 did not have the disease. Medical care, hot meals and free burial insurance were given to those who participated. The men were told that the study would last six months, but in the end it continued for 40 years. After funding for treatment was lost, the study was continued without informing the men that they were only being studied and would not be treated. Facing insufficient participation, the Macon County Health Department nevertheless wrote to subjects to offer them a "last chance" to get a special "treatment", which was not a treatment at all, but a spinal tap administered exclusively for diagnostic purposes. None of the men infected were ever told that they had the disease, and none were treated with penicillin even after the antibiotic had been proven to successfully treat syphilis. According to the Centers for Disease Control, the men were told they were being treated for "bad blood"—a colloquialism describing various conditions such as fatigue, anemia and syphilis—which was a leading cause of death among southern African-American men.
The 40-year study became a textbook example of poor medical ethics because researchers had knowingly withheld treatment with penicillin and because the subjects had been misled concerning the purposes of the study. The revelation in 1972 of these study failures by a whistleblower, Peter Buxtun, led to major changes in U.S. law and regulation on the protection of participants in clinical studies. Now studies require informed consent, communication of diagnosis, and accurate reporting of test results.
Similar experiments were carried out in Guatemala from 1946 to 1948. It was done during the administration of American President Harry S. Truman and Guatemalan President Juan José Arévalo with the cooperation of some Guatemalan health ministries and officials. Doctors infected soldiers, prostitutes, prisoners and mental patients with syphilis and other sexually transmitted infections, without the informed consent of the subjects, and treated most subjects with antibiotics. The experiment resulted in at least 83 deaths. In October 2010, the U.S. formally apologized to Guatemala for the ethical violations that took place. Secretary of State Hillary Clinton and Health and Human Services Secretary Kathleen Sebelius stated "Although these events occurred more than 64 years ago, we are outraged that such reprehensible research could have occurred under the guise of public health. We deeply regret that it happened, and we apologize to all the individuals who were affected by such abhorrent research practices." The experiments were led by physician John Charles Cutler who also participated in the late stages of the Tuskegee syphilis experiment.
The "Tuskegee Study of Untreated Syphilis in the Negro Male" was an infamous, unethical and racist clinical trial, clinical study conducted between 1932 and 1972 by the U.S. Public Health Service. Whereas the purpose of this study was to observe the Natural history of disease, natural history of untreated syphilis; the African-American men in the study were told they were receiving free treatment for "bad blood" from the United States government.
The Public Health Service started working on this study in 1932 in collaboration with Tuskegee University, a historically black college in Alabama. Researchers enrolled 600 poor, African-American sharecroppers from Macon County, Alabama, Macon County, Alabama in the study. Of these men, 399 had contracted syphilis before the study began, and 201 did not have the disease. Medical care, hot meals and free burial insurance were given to those who participated. The men were told that the study would last six months, but in the end it continued for 40 years. After funding for treatment was lost, the study was continued without informing the men that they were only being studied and would not be treated. Facing insufficient participation, the Macon County Health Department nevertheless wrote to subjects to offer them a "last chance" to get a special "treatment", which was not a treatment at all, but a spinal tap administered exclusively for diagnostic purposes. None of the men infected were ever told that they had the disease, and none were treated with penicillin even after the antibiotic had been proven to successfully treat syphilis. According to the Centers for Disease Control, the men were told they were being treated for "bad blood"—a colloquialism describing various conditions such as fatigue, anemia and syphilis—which was a leading cause of death among southern African-American men.
The 40-year study became a textbook example of poor medical ethics because researchers had knowingly withheld treatment with penicillin and because the subjects had been misled concerning the purposes of the study. The revelation in 1972 of these study failures by a whistleblower, Peter Buxtun, led to major changes in U.S. law and regulation on the protection of participants in clinical studies. Now studies require informed consent, communication of diagnosis, and accurate reporting of test results.
Similar experiments were carried out in Guatemala from 1946 to 1948. It was done during the administration of American President Harry S. Truman and Guatemalan President Juan José Arévalo with the cooperation of some Guatemalan health ministries and officials. Doctors infected soldiers, prostitutes, prisoners and mental patients with syphilis and other sexually transmitted infections, without the informed consent of the subjects, and treated most subjects with antibiotics. The experiment resulted in at least 83 deaths. In October 2010, the U.S. formally apologized to Guatemala for the ethical violations that took place. Secretary of State Hillary Clinton and Health and Human Services Secretary Kathleen Sebelius stated "Although these events occurred more than 64 years ago, we are outraged that such reprehensible research could have occurred under the guise of public health. We deeply regret that it happened, and we apologize to all the individuals who were affected by such abhorrent research practices." The experiments were led by physician John Charles Cutler who also participated in the late stages of the Tuskegee syphilis experiment.
Names
It was first called ''grande verole'' or the "great pox" by the French. Other historical names have included "button scurvy", sibbens, frenga and dichuchwa, among others. Since it was a disgraceful disease, the disease was known in several countries by the name of their neighbouring country. The English, the Germans, and the Italians called it "the French disease", while the French referred to it as the "Neapolitan disease". The Dutch called it the "Spanish/Castilian disease". To the Turks it was known as the "Christian disease", whilst in India, the Hindus and Muslims named the disease after each other.References
Further reading
* *External links
"Syphilis - CDC Fact Sheet"
Centers for Disease Control and Prevention (CDC)
UCSF HIV InSite Knowledge Base Chapter: Syphilis and HIV
Recommendations for Public Health Surveillance of Syphilis in the United States
* {{Authority control Syphilis, Bacterial diseases Bacterium-related cutaneous conditions Infectious diseases Infectious diseases with eradication efforts Infections with a predominantly sexual mode of transmission Sexually transmitted diseases and infections Spirochaetes Wikipedia medicine articles ready to translate (full) Wikipedia infectious disease articles ready to translate