Prevalence of adverse events
 Millennia ago, Hippocrates recognized the potential for injuries that arise from the well-intentioned actions of healers. Greek healers in the 4th century BC drafted the Hippocratic Oath and pledged to "prescribe regimens for the good of my patients according to my ability and my judgment and never do harm to anyone."
Since then, the directive ''primum non nocere'' ("first do no harm") has become a central tenet for contemporary medicine. However, despite an increasing emphasis on the scientific basis of medical practice in Europe and the United States in the late 19th century, data on adverse outcomes were hard to come by and the various studies commissioned collected mostly anecdotal events.
In the United States, the public and the medical specialty of anesthesia were shocked in April 1982 by the ABC television program
Millennia ago, Hippocrates recognized the potential for injuries that arise from the well-intentioned actions of healers. Greek healers in the 4th century BC drafted the Hippocratic Oath and pledged to "prescribe regimens for the good of my patients according to my ability and my judgment and never do harm to anyone."
Since then, the directive ''primum non nocere'' ("first do no harm") has become a central tenet for contemporary medicine. However, despite an increasing emphasis on the scientific basis of medical practice in Europe and the United States in the late 19th century, data on adverse outcomes were hard to come by and the various studies commissioned collected mostly anecdotal events.
In the United States, the public and the medical specialty of anesthesia were shocked in April 1982 by the ABC television program ''To Err is Human''
In the United States, the full magnitude and impact of errors in health care was not appreciated until the 1990s, when several reports brought attention to this issue. In 1999, the Institute of Medicine (IOM) of the National Academy of Sciences released a report, '' To Err is Human: Building a Safer Health System''. The IOM called for a broad national effort to include establishment of a Center for Patient Safety, expanded reporting of adverse events, development of safety programs in health care organizations, and attention by regulators, health care purchasers, and professional societies. The majority of media attention, however, focused on the staggering statistics: from 44,000 to 98,000 preventable deaths annually due to medical error in hospitals, 7,000 preventable deaths related to medication errors alone. Within 2 weeks of the report's release, Congress began hearings and President Clinton ordered a government-wide study of the feasibility of implementing the report's recommendations. Initial criticisms of the methodology in the IOM estimates focused on the statistical methods of amplifying low numbers of incidents in the pilot studies to the general population. However, subsequent reports emphasized the striking prevalence and consequences of medical error. The experience has been similar in other countries. *Ten years after a groundbreaking Australian study revealed 18,000 annual deaths from medical errors, Professor Bill Runciman, one of the study's authors and president of the Australian Patient Safety Foundation since its inception in 1989, reported himself a victim of a medical dosing error. *The Department of Health Expert Group in June 2000 estimated that over 850,000 incidents harm10 facts on patient safety
Accessed 2008-05-19
Communication
Effective communication is essential for ensuring patient safety. Communicating starts with the provisioning of available information on any operational site especially in mobile professional services. Communicating continues with the reduction of administrative burden, releasing the operating staff and easing the operational demand by model driven orders, thus enabling adherence to a well executable procedure finalized with a qualified minimum of required feedback.Effective and ineffective communication
 The use of effective communication among patients and healthcare professionals is critical for achieving a patient's optimal health outcome. However, scientific patient safety research by Annegret Hannawa, among others, has shown that ineffective communication has the opposite effect as it can lead to severe patient harm. Communication with regards to patient safety can be classified into two categories: prevention of adverse events and responding to adverse events. Use of effective communication can aid in the prevention of adverse events, whereas ineffective communication can contribute to these incidences. If ineffective communication contributes to an adverse event, then better and more effective communication skills must be applied in response to achieve optimal outcomes for the patient's safety. There are different modes in which healthcare professionals can work to optimize the safety of patients which include both verbal and nonverbal communication, as well as the effective use of appropriate communication technologies.
Methods of effective verbal and nonverbal communication include treating patients with respect and showing empathy, clearly communicating with patients in a way that best fits their needs, practicing active listening skills, being sensitive with regards to cultural diversity and respecting the privacy and confidentiality rights of the patient. To use appropriate communication technology, healthcare professionals must choose which channel of communication is best suited to benefit the patient. Some channels are more likely to result in communication errors than others, such as communicating through telephone or email (missing nonverbal messages which are an important element of understanding the situation). It is also the responsibility of the provider to know the advantages and limitations of using electronic health records, as they do not convey all information necessary to understanding patient needs. If a health care professional is not practicing these skills, they are not being an effective communicator which may affect patient outcome.
The goal of a healthcare professional is to aid a patient in achieving their optimal health outcome, which entails that the patient's safety is not at risk. Practice of effective communication plays a large role in promoting and protecting patient safety.
The use of effective communication among patients and healthcare professionals is critical for achieving a patient's optimal health outcome. However, scientific patient safety research by Annegret Hannawa, among others, has shown that ineffective communication has the opposite effect as it can lead to severe patient harm. Communication with regards to patient safety can be classified into two categories: prevention of adverse events and responding to adverse events. Use of effective communication can aid in the prevention of adverse events, whereas ineffective communication can contribute to these incidences. If ineffective communication contributes to an adverse event, then better and more effective communication skills must be applied in response to achieve optimal outcomes for the patient's safety. There are different modes in which healthcare professionals can work to optimize the safety of patients which include both verbal and nonverbal communication, as well as the effective use of appropriate communication technologies.
Methods of effective verbal and nonverbal communication include treating patients with respect and showing empathy, clearly communicating with patients in a way that best fits their needs, practicing active listening skills, being sensitive with regards to cultural diversity and respecting the privacy and confidentiality rights of the patient. To use appropriate communication technology, healthcare professionals must choose which channel of communication is best suited to benefit the patient. Some channels are more likely to result in communication errors than others, such as communicating through telephone or email (missing nonverbal messages which are an important element of understanding the situation). It is also the responsibility of the provider to know the advantages and limitations of using electronic health records, as they do not convey all information necessary to understanding patient needs. If a health care professional is not practicing these skills, they are not being an effective communicator which may affect patient outcome.
The goal of a healthcare professional is to aid a patient in achieving their optimal health outcome, which entails that the patient's safety is not at risk. Practice of effective communication plays a large role in promoting and protecting patient safety.
Teamwork and communication
During complex situations, communication between health professionals must be at its best. There are several techniques, tools, and strategies used to improve communication. Any team should have a clear purpose and each member should be aware of their role and be involved accordingly. To increase the quality of communication between people involved, regular feedback should be provided. Strategies such as briefings allow the team to be set on their purpose and ensure that members not only share the goal but also the process they will follow to achieve it. Briefings reduce interruptions, prevent delays and build stronger relationships, resulting in a strong patient safety environment.Safety culture
As is the case in other industries, when there is a mistake or error made people look for someone to blame. This may seem natural, but it creates a blame culture where ''who'' is more important than ''why'' or ''how''. A ''just culture'', also sometimes known as ''no blame'' or ''no fault'', seeks to understand the root causes of an incident rather than just who was involved. In health care, there is a move towards a patient safety culture. This applies the lessons learned from other industries, such asDisclosure of an incident
After an adverse event occurs, each country has its own way of dealing with the incident. In Canada, a quality improvement review is primarily used. A quality improvement review is an evaluation that is completed after an adverse event occurs with the intention to both fix the problem, as well as preventing it from happening again. The individual provinces and territories have laws on whether it is required to disclose the quality improvement review to the patient. Healthcare providers have an obligation to disclose any adverse event to their patients because of ethical and professional guidelines. If more providers participate in the quality improvement review, it can increase interdisciplinary collaboration and can sustain relationships between departments and staff. In the US,Causes of healthcare error
The simplest definition of a health care error is a preventableSeminole County Patient Safety Summit
, April 22, 2006) ;Human Factors *Variations in healthcare provider training & experience, fatigue, depression and burnout. *Diverse patients, unfamiliar settings, time pressures. *Failure to acknowledge the prevalence and seriousness of medical errors. * Increasing working hours of healthcare personnel *mislabeling specimen or forgetting to label specimen *states of anxiety and stress ;Medical complexity *Complicated technologies, powerful drugs. *Intensive care, prolonged hospital stay. ;System failures *Unsafe communication *Unclear lines of authority of physicians, nurses, and other care providers. *Complications increase as patient to nurse staffing ratio increases. *Disconnected reporting systems within a hospital: fragmented systems in which numerous hand-offs of patients results in lack of coordination and errors. *Drug names that look alike or sound alike. *The impression that action is being taken by other groups within the institution. *Reliance on automated systems to prevent error. *Inadequate systems to share information about errors hamper analysis of contributory causes and improvement strategies. *Cost-cutting measures by hospitals in response to reimbursement cutbacks. *Environment and design factors. In emergencies, patient care may be rendered in areas poorly suited for safe monitoring. The American Institute of Architects has identified concerns for the safe design and construction of health care facilities. *Infrastructure failure. According to the WHO, 50% of medical equipment in developing countries is only partly usable due to lack of skilled operators or parts. As a result, diagnostic procedures or treatments cannot be performed, leading to substandard treatment. The Joint Commission's Annual Report on Quality and Safety 2007 found that inadequate communication between healthcare providers, or between providers and the patient and family members, was the root cause of over half the serious adverse events in accredited hospitals. Other leading causes included inadequate assessment of the patient's condition, and poor leadership or training. Common misconceptions about adverse events are: * "'Bad apples' or incompetent health care providers are a common cause." Many of the errors are normal human slips or lapses, and not the result of poor judgment or recklessness. * "High risk procedures or medical specialties are responsible for most ''avoidable'' adverse events". Although some mistakes, such as in surgery, are easier to notice, errors occur in all levels of care. Even though complex procedures entail more risk, adverse outcomes are not usually due to error, but to the severity of the condition being treated. However, USP has reported that medication errors during the course of a surgical procedure are three times more likely to cause harm to a patient than those occurring in other types of hospital care. * "If a patient experiences an adverse event during the process of care, an error has occurred". Most medical care entails some level of risk, and there can be complications or side effects, even unforeseen ones, from the underlying condition or from the treatment itself. Nursing Burnout and Patient Safety In the medical field there are many things that can lead to a decrease of patient safety. One big influence on this is nurse burnout, leading to hundreds of thousands of deaths a year, to billions of dollars spent when having to rectify a new problem, this is a real issue in the world. On average in the medical field, 1 out of 20 prescriptions filled contains an error, considering the billions of prescriptions that get filled ever year there is an insane amount of error happening. And with these errors not only is there a likelihood of a prescription being wrong but there is a $3.5 billion price-tag that goes with that covering the amount that people pay each year for litigation costs and extra days that patients need to stay in hospital beds because of mistakes from the hospital. Out of these patients that end up sitting in beds because of medical malpractice or burnout related decreases in patent safety, around 250,000 of them die a year in the United States alone. This high mortality rate is the third leading cause of death in the country, because when workers are constantly stressed and overworked, mistakes are going to happen. These errors and other variables have caused a significant amount of death within hospitals due to a decrease in patient safety, which is brought on by workers being burnt out and overworked especially during the recent years during the pandemic. Burnout has been going on for years amongst nurses and other physicians, affecting nearly half of healthcare workers. Burnout has been going on for decades and the term was originally coined by Herbert Freudenberger who was working at a free clinic and overtime he mentioned some of the effects that he had seen, "emotional depletion and accompanying psychosomatic symptoms...excessive demands on energy, strength, or resources". These symptoms are commonly seen today in hospital settings as nurses feel like they are pushed to the edge. This situation is not ideal for people to feel, especially not people who have to look after patients and take care of others who can be in very severe states. Using what Freudenberger described, there was a scale created to measure the amount of burnout in the healthcare field. Known as Maslach's scale, this measures 1) Workload 2) Control 3) Reward 4) Community 5) Fairness and 6) Values. All of these core points work together and the less you have of them the more likely that burnout will occur and cause a major decrease in patient safety. Similarly to Maslach’s scale, there is the Conservation of Resources Theory which essentially states that if one of the four pillars are lost, so is safety and control, “Healthcare organizations and nursing administration should develop strategies to protect nurses from the threat of resource loss to decrease nurse burnout, which may improve nurse and patient safety.” The amount of nursing professionals that have experienced burnout is said to be around 50%, this number leads to an increased risk of adverse events that shouldn't happen, anywhere from 26% to 70% higher risk that something bad will happen to the patient.
Safety programs in industry
;Aviation safety :In the United States, two organizations contribute to one of the world's lowest aviation accident rates. Mandatory accident investigation is carried out by the National Transportation Safety Board, while theTeam Stepps
which was introduced by the Agency for Healthcare Research and Quality (AHRQ). The AHRQ calls this program "an evidence-based teamwork system to improve communication and teamwork skills among health care professionals." ;Near-miss reporting :A near miss is an unplanned event that did not result in injury, illness, or damage - but had the potential to do so. Reporting of near misses by observers is an established error reduction technique in aviation, and has been extended to private industry, traffic safety and fire-rescue services with reductions in accidents and injury. AORN, a US-based professional organization of perioperative registered nurses, has put in effect a voluntary near miss reporting system (SafetyNet), covering medication or transfusion reactions, communication or consent issues, wrong patient or procedures, communication breakdown or technology malfunctions. An analysis of incidents allows safety alerts to be issued to AORN members. AlmostME is another commercially offered solution for near-miss reporting in healthcare. ;Limits of the industrial safety model : Unintended consequences may occur as improvements in safety are undertaken. It may not be possible to attain maximum safety goals in healthcare without adversely affecting patient care in other ways. An example is blood transfusion; in recent years, to reduce the risk of transmissible infection in the blood supply, donors with only a small probability of infection have been excluded. The result has been a critical shortage of blood for other lifesaving purposes, with a broad impact on patient care. Application of high-reliability theory and normal accident theory can help predict the organizational consequences of implementing safety measures.
Technology in healthcare
;Overview According to a study by RAND Health, the U.S. healthcare system could save more than $81 billion annually, reduce adverse healthcare events, and improve the quality of care ifTypes of healthcare technology
Handwritten reports or notes, manual order entry, non-standard abbreviations and poor legibility lead to substantial errors and injuries, according to the IOM (2000) report. The follow-up IOM report, ''Crossing the Quality Chasm: A New Health System for the 21st Century'', advised rapid adoption of electronic patient records, electronic medication ordering, with computer- and internet-based information systems to support clinical decisions. This section contains only the patient safety related aspects of HIT.= Electronic health record (EHR)
= The electronic health record (EHR), previously known as the= Active RFID platform
= These systems' basic security measures are based on sound identifying electronic tags, in order that the patient details provided in different situations are always reliable. These systems offer three differently qualified options: * Identification upon request of health care personnel, using scanners (similar to readers for passive RFID tags or scanners for barcode labels) to identify patient semi-automatically upon presentation of patient with tag to staff * Automatic identification upon entry of patient. An automatic identification check is carried out on each person with tags (primarily patients) entering the area to determine the presented patient in contrast to other patient earlier entered into reach of the used reader. * Automatic identification and range estimation upon approach to most proximate patient, excluding reads from more distant tags of other patients in the same area Any of these options may be applied whenever and wherever patient details are required in electronic form Such identifying is essential when the information concerned is critical. There are increasing numbers of hospitals that have an RFID system to identify patients, for instanceHospital La Fe in Valencia(Spain)
Wayne Memorial Hospital (US); Royal Alexandria Hospital (UK).
=Computerized Provider Order Entry (CPOE)
= Prescribing errors are the largest identified source of preventable errors in hospitals (IOM, 2000; 2007). The IOM (2006) estimates that each hospitalized patient, on average, is exposed to one medication error each day. Computerized provider order entry (CPOE), formerly called computerized physician order entry, can reduce medication errors by 80% overall but more importantly decrease harm to patients by 55%. A Leapfrog (2004) survey found that 16% of US clinics, hospitals, and medical practices are expected to utilize CPOE within 2 years. ;Complete Safety Medication System A standardized= Specific Patient Safety Software
= A standardized, modular technology system that allows a hospital, clinic, or health system record their Incidents that include falls, medication errors, pressure ulcers, near misses, etc. These systems can be configured to specific workflows and the analytics behind it will allow for reporting and dashboards to help learn from things that have gone wrong (and right). Some vendors include Datix, RL Solutions, Verge, Midas, and Quantros.Technological Iatrogenesis
Technology induced errors are significant and increasingly more evident in care delivery systems. This idiosyncratic and potentially serious problems associated with HIT implementation has recently become a tangible concern for healthcare and information technology professionals. As such, the term technological iatrogenesis describes this new category of adverse events that are an emergent property resulting from technological innovation creating system and microsystem disturbances. Healthcare systems are complex and adaptive, meaning there are many networks and connections working simultaneously to produce certain outcomes. When these systems are under the increased stresses caused by the diffusion of new technology, unfamiliar and new process errors often result. If not recognized, over time these new errors can collectively lead to catastrophic system failures. The term "e-iatrogenesis" can be used to describe the local error manifestation. The sources for these errors include: *Prescriber and staff inexperience may lead to a false sense of security; that when technology suggests a course of action, errors are avoided. *Shortcut or default selections can override non-standard medication regimens for elderly or underweight patients, resulting in toxic doses. *CPOE and automated drug dispensing was identified as a cause of error by 84% of over 500 health care facilities participating in a surveillance system by theEvidence-based medicine
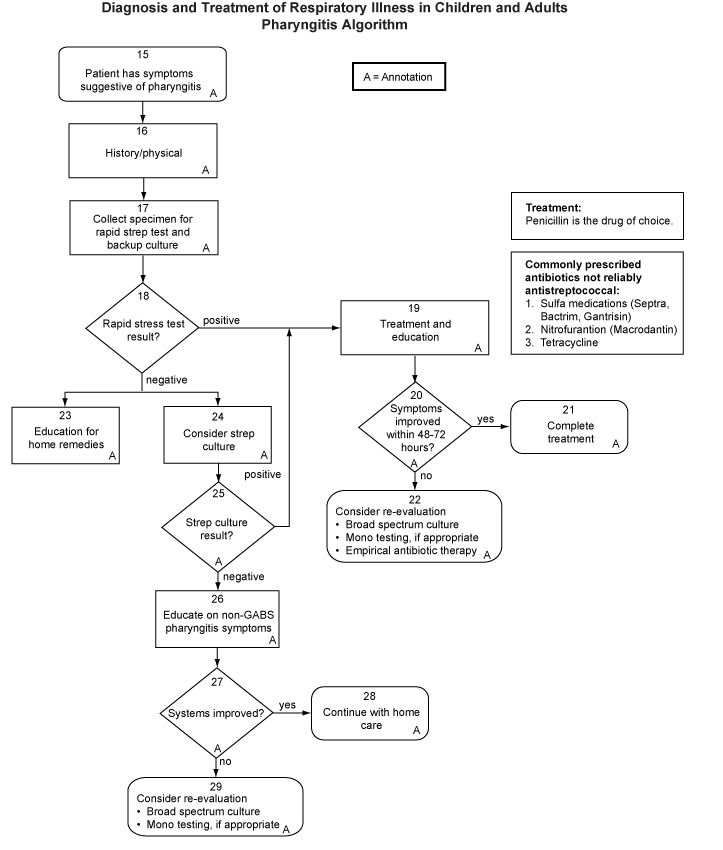 ]
Evidence-based medicine integrates an individual doctor's exam and diagnostic skills for a specific patient, with the best available evidence from medical research. The doctor's expertise includes both diagnostic skills and consideration of individual patient's rights and preferences in making decisions about his or her care. The clinician uses pertinent clinical research on the accuracy of diagnostic tests and the efficacy and safety of therapy, rehabilitation, and prevention to develop an individual plan of care. The development of evidence-based recommendations for specific medical conditions, termed clinical practice guidelines or "best practices", has accelerated in the past few years. In the United States, over 1,700 guidelines (see example image, right) have been developed as a resource for physicians to apply to specific patient presentations.Agency for Healthcare Research and Quality
]
Evidence-based medicine integrates an individual doctor's exam and diagnostic skills for a specific patient, with the best available evidence from medical research. The doctor's expertise includes both diagnostic skills and consideration of individual patient's rights and preferences in making decisions about his or her care. The clinician uses pertinent clinical research on the accuracy of diagnostic tests and the efficacy and safety of therapy, rehabilitation, and prevention to develop an individual plan of care. The development of evidence-based recommendations for specific medical conditions, termed clinical practice guidelines or "best practices", has accelerated in the past few years. In the United States, over 1,700 guidelines (see example image, right) have been developed as a resource for physicians to apply to specific patient presentations.Agency for Healthcare Research and QualityThe National Guideline Clearinghouse
The National Institute for Health and Clinical Excellence (NICE) in the United Kingdom provides detailed "clinical guidance" for both health care professionals and the public about specific medical conditions.The National Institute for Health and Clinical Excellence (NICE
Providing national guidance on promoting good health
National Guideline Agencies from all continents collaborate in the Guidelines International Network, which entertains the largest guideline library worldwide. The International Standard ISO 15189:2007 for Accreditation of Medical Laboratory requires laboratories to continuously monitor and improve the quality of their facilities. Advantages:Institute of Medicine
Guidelines for Clinical Practice: From Development to Use
(1992) #Evidence-based medicine may reduce adverse events, especially those involving incorrect diagnosis, outdated or risky tests or procedures, or medication overuse. #Clinical guidelines provide a common framework for improving communication among clinicians, patients and non-medical purchasers of health care. #Errors related to changing shifts or multiple specialists are reduced by a consistent plan of care. #Information on the clinical effectiveness of treatments and services can help providers, consumers and purchasers of health care make better use of limited resources. #As medical advances become available, doctors and nurses can keep up with new tests and treatments as guidelines are improved. Drawbacks:American College of Surgeons Bulletin
#Managed care plans may attempt limit "unnecessary" services to cut the costs of health care, despite evidence that guidelines are not designed for general screening, rather as decision-making tools when an individual practitioner evaluates a specific patient. #The medical literature is evolving and often controversial; development of guidelines requires consensus. #Implementing guidelines and educating the entire health care team within a facility costs time and resources (which may be recovered by future efficiency and error reduction). #Clinicians may resist evidence-based medicine as a threat to traditional relationships between patients, doctors and other health professionals, since any participant can influence decisions. #Failing to follow guidelines might increase the risk of liability or disciplinary action by regulators.
Quality and safety initiatives in community pharmacy practice
Community pharmacy practice is making important advances in the quality and safety movement despite the limited number of federal and state regulations that exist and in the absence of national accreditation organizations such as the Joint Commission - a driving force for performance improvement in health care systems. Community pharmacies are using automated drug dispensing devices (robots), computerized drug utilization review tools, and most recently, the ability to receive electronic prescriptions from prescribers to decrease the risk for error and increase the likelihood of delivering high quality of care. Quality Assurance (QA) in community practice is a relatively new concept. , only 16 states have some form of legislation that regulates QA in community pharmacy practice. While most state QA legislation focuses on error reduction, North Carolina has recently approved legislation that requires the pharmacy QA program to include error reduction strategies and assessments of the quality of their pharmaceutical care outcomes and pharmacy services. New technologies facilitate the traceability tools of patients and medications. This is particularly relevant for drugs that are considered high risk and cost.Quality Improvement and Safety Initiatives in Pediatrics
Quality improvement and patient safety is a major concern in the pediatric world of health care. This next section will focus on quality improvement and patient safety initiatives in inpatient settings. Over the last several years, pediatric groups have partnered to improve general understanding, reporting, process improvement methodologies, and quality of pediatric inpatient care. These collaborations have created a robust program of projects, benchmarking efforts, and research. Much of the research and focus on adverse events has been on medication errors–the most frequently reported adverse event for both adult and pediatric patients. It is also of interest to note that medication errors are also the most preventable type of harm that can occur within the pediatric population. It has been reported that when pediatric medication errors occur, these patients have a higher rate of death associated with the error than adult patients. A more recent review of potential pediatric safety issues conducted by Miller, Elixhauser, and Zhan found that hospitalized children who experienced a patient safety incident, compared with those who did not, had * 1) Length of stay 2- to 6-fold longer * 2) Hospital mortality 2- to 18-fold greater * 3) Hospital charges 2- to 20-fold higher In order to reduce these errors the attention on safety needs to revolve around designing safe systems and processes. Slonim and Pollack point out that safety is critical to reduce medical errors and adverse events. These problems can range from diagnostic and treatment errors to hospital-acquired infections, procedural complications, and failure to prevent problems such as pressure ulcers. In addition to addressing quality and safety issues found in adult patients there are a few characteristics that are unique to the pediatric population. * Development: As children mature both cognitively and physically, their needs as consumers of health care goods and services change. Therefore, planning a unified approach to pediatric safety and quality is affected by the fluid nature of childhood development. * * Dependency: Hospitalized children, especially those who are very young and/or nonverbal, are dependent on caregivers, parents, or other surrogates to convey key information associated with patient encounters. Even when children can accurately express their needs, they are unlikely to receive the same acknowledgment accorded adult patients. In addition, because children are dependent on their caregivers, their care must be approved by parents or surrogates during all encounters. * * Different epidemiology: Most hospitalized children require acute episodic care, not care for chronic conditions as with adult patients. Planning safety and quality initiatives within a framework of "wellness, interrupted by acute conditions or exacerbations," presents distinct challenges and requires a new way of thinking. * * Demographics: Children are more likely than other groups to live in poverty and experience racial and ethnic disparities in health care. Children are more dependent on public insurance, such as State Children's Health Insurance Program (SCHIP) and Medicaid. One of the main challenges faced by pediatric safety and quality efforts is that most of the work on patient safety to date has focused on adult patients. In addition, there is no standard nomenclature for pediatric patient safety that is widely used. However, a standard framework for classifying pediatric adverse events that offers flexibility has been introduced. Standardization provides consistency between interdisciplinary teams and can facilitate multisite studies. If these large-scale studies are conducted, the findings could generate large-scale intervention studies conducted with a faster life cycle. Leaders in Pediatric Safety and Quality The Agency for Healthcare Research and Quality (AHRQ) is the Federal authority for patient safety and quality of care and has been a leader in pediatric quality and safety. AHRQ has developed Pediatric Quality Indicators (PedQIs) with the goal to highlight areas of quality concern and to target areas for further analysis. Eighteen pediatric quality indicators are included in the AHRQ quality measure modules; based on expert input, risk adjustment, and other considerations. Thirteen inpatient indicators are recommended for use at the hospital level, and five are designated area indicators. Inpatient indicators are treatments or conditions with the greatest potential of an adverse event for hospitalized children. Possible additions to the dataset will address the patient's condition on admission and increase the understanding of how laboratory and pharmacy utilization impact patient outcomes. The goal of AHRQ is to refine the area-level indicators to improve outcomes for children receiving outpatient care and reduce the incidence of hospitalization for those defined conditions. Collaborations for Pediatric Safety and Quality Numerous groups are engaged in improving pediatric care, quality and safety. Each of these groups has a unique mission and membership. The following table details these groups' missions and websites. Nurse Staffing and Pediatric Outcomes While the number of nurses providing patient care is recognized as an inadequate measure of nursing care quality, there is hard evidence that nurse staffing is directly related to patient outcomes. Studies by Aiken and Needleman have demonstrated that patient death, nosocomial infections, cardiac arrest, and pressure ulcers are linked to inadequate nurse-to-patient ratios. The presence or absence of registered nurses (RNs) impacts the outcome for pediatric patients requiring pain management and/or peripheral administration of intravenous fluids and/or medications. These two indicators of pediatric nursing care quality are sensitive measures of nursing care. Professional nurses play a key role in successful pain management, especially among pediatric patients unable to verbally describe pain. Astute assessment skills are required to intervene successfully and relieve discomfort.33 Maintenance of a patient's intravenous access is a clear nursing responsibility. Pediatric patients are at increased risk for intravenous infiltration and for significant complications of infiltration, should it occur. The characteristics of effective indicators of pediatric nursing care quality include the following: * Scalable: The indicators are applicable to pediatric patients across a broad range of units and hospitals, in both intensive care and general care settings. * Feasible: Data collection does not pose undue burden on staff of participating units as the data is available from existing sources, such as the medical record or a quality improvement database, and can be collected in real time. * Valid and reliable: Indicator measurement within and across participating sites is accurate and consistent over time. Conclusions Pediatric care is complex due to developmental and dependency issues associated with children. How these factors impact the specific processes of care is an area of science in which little is known. Throughout health care providing safe and high quality patient care continues to provide significant challenges. Efforts to improve the safety and quality of care are resource intensive and take continued commitment not only by those who deliver care, but also by agencies and foundations that fund this work. Advocates for children's health care must be at the table when key policy and regulatory issues are discussed. Only then will the voice of our most vulnerable groups of health care consumers be heard. Working Hours of Nurses and Patient Safety A recent increase in work hours and overtime shifts of nurses has been used to compensate for the decrease of registered nurses (RNs). Logbooks completed by nearly 400 RNs have revealed that about "40 percent of the 5,317 work shifts they logged exceeded twelve hours." Errors by hospital staff nurses are more likely to occur when work shifts extend beyond 12 hours, or they work over 40 hours in one week. Studies have shown that overtime shifts have harmful effects on the quality of care provided to patients, but some researchers "who evaluated the safety of 12-hour shifts did not find increases in medication errors." The errors which these researchers found were "lapses of attention to detail, errors of omission, compromised problem solving, reduced motivation" due to fatigue as well as "errors in grammatical reasoning and chart reviewing." Overworked nurses are a serious safety concern to their patients wellbeing. Working back to back shifts, or night shifts, are a common cause of fatigue in hospital staff nurses. "Less sleep, or fatigue, may lead to increased likelihood of making an error, or even the decreased likelihood of catching someone else's error." Limiting working hours and shift rotations could "reduce the adverse effects of fatigue" and increase the quality of care of patients.Health literacy
Health literacy is a common and serious safety concern. A study of 2,600 patients at two hospitals determined that between 26 and 60% of patients could not understand medication directions, a standard informed consent, or basic health care materials. This mismatch between a clinician's level of communication and a patient's ability to understand can lead to medication errors and adverse outcomes. The Institute of Medicine (2004) report found low health literacy levels negatively affects healthcare outcomes. In particular, these patients have a higher risk of hospitalization and longer hospital stays, are less likely to comply with treatment, are more likely to make errors with medication, and are more ill when they seek medical care.Pay for performance (P4P)
Pay for performance systems link compensation to measures of work quality or goals. , 75 percent of all U.S. companies connect at least part of an employee's pay to measures of performance, and in healthcare, over 100 private and federal pilot programs are underway. Current methods of healthcare payment may actually reward less-safe care, since some insurance companies will not pay for new practices to reduce errors, while physicians and hospitals can bill for additional services that are needed when patients are injured by mistakes.The Commonwealth FundFive Years After "To Err Is Human": What Have We Learned?
However, early studies showed little gain in quality for the money spent, as well as evidence suggesting unintended consequences, like the avoidance of high-risk patients, when payment was linked to outcome improvements. The 2006 Institute of Medicine report ''Preventing Medication Errors'' recommended "incentives...so that profitability of hospitals, clinics, pharmacies, insurance companies, and manufacturers (are) aligned with patient safety goals;...(to) strengthen the business case for quality and safety." There is widespread international interest in health care pay-for-performance programs in a range of countries, including the United Kingdom,National Health Service
Quality and Outcomes Framework data
Retrieved July 8, 2006 United States, Australia, Canada,, Retrieved 2008-07-18 Germany, the Netherlands, and New Zealand.
United Kingdom
In the United Kingdom, theUnited States
In the United States, Medicare has various pay-for-performance ("P4P") initiatives in offices, clinics and hospitals, seeking to improving quality and avoid unnecessary health care costs. The Centers for Medicare and Medicaid Services (CMS) has several demonstration projects underway offering compensation for improvements: *Payments for better care coordination between home, hospital and offices for patients with chronic illnesses. In April 2005, CMS launched its first value-based purchasing pilot or "demonstration" project- the three-year Medicare Physician Group Practice (PGP) Demonstration. The project involves ten large, multi-specialty physician practices caring for more than 200,000 Medicare fee-for-service beneficiaries. Participating practices will phase in quality standards for preventive care and the management of common chronic illnesses such as diabetes. Practices meeting these standards will be eligible for rewards from savings due to resulting improvements in patient management. The ''First Evaluation Report to Congress'' in 2006 showed that the model rewarded high quality, efficient provision of health care, but the lack of up-front payment for the investment in new systems of case management "have made for an uncertain future with respect for any payments under the demonstration." *A set of 10 hospital quality measures which, if reported to CMS, will increase the payments that hospitals receive for each discharge. By the third year of the demonstration, those hospitals that do not meet a threshold on quality will be subject to reductions in payment. Preliminary data from the second year of the study indicates that pay for performance was associated with a roughly 2.5% to 4.0% improvement in compliance with quality measures, compared with the control hospitals. Dr. Arnold Epstein of the Harvard School of Public Health commented in an accompanying editorial that pay-for-performance "is fundamentally a social experiment likely to have only modest incremental value." Unintended consequences of some publicly reported hospital quality measures have adversely affected patient care. The requirement to give the first antibiotic dose in the emergency department within 4 hours, if the patient has pneumonia, has caused an increase in pneumonia misdiagnosis. *Rewards to physicians for improving health outcomes by the use ofComplex illness
Pay for performance programs often target patients with serious and complex illnesses; such patients commonly interact with multiple healthcare providers and facilities. However, pilot programs now underway focus on simple indicators such as improvement in lab values or use of emergency services, avoiding areas of complexity such as multiple complications or several treating specialists. A 2007 study analyzing Medicare beneficiaries' healthcare visits showed that a median of two primary care physicians and five specialists provide care for a single patient. The authors doubt that pay-for-performance systems can accurately attribute responsibility for the outcome of care for such patients. The American College of Physicians Ethics has stated concerns about using a limited set of clinical practice parameters to assess quality, "especially if payment for good performance is grafted onto the current payment system, which does not reward robust comprehensive care...The elderly patient with multiple chronic conditions is especially vulnerable to this unwanted effect of powerful incentives." Present pay-for-performance systems measure good performance based on specified clinical measurements, such asPublic reporting
Mandatory reporting
;Denmark :The Danish Act on Patient Safety passed Parliament in June 2003, and on January 1, 2004, Denmark became the first country to introduce nationwide mandatory reporting. The Act obligates frontline personnel to report adverse events to a national reporting system. Hospital owners are obligated to act on the reports and the National Board of Health is obligated to communicate the learning nationally. The reporting system is intended purely for learning and frontline personnel cannot experience sanctions for reporting. This is stated in Section 6 of the Danish Act on Patient Safety (as of January 1, 2007: Section 201 of the Danish Health Act): "A frontline person who reports an adverse event cannot as a result of that report be subjected to investigation or disciplinary action from the employer, the Board of Health or the Court of Justice." The reporting system and the Danish Patient Safety Database is described in further detail in a National Board of Health publication. ;United Kingdom :The National Patient Safety Agency encourages voluntary reporting of health care errors, but has several specific instances, known as "Confidential Enquiries", for which investigation is routinely initiated: maternal or infant deaths, childhood deaths to age 16, deaths in persons with mental illness, and perioperative and unexpected medical deaths. Medical records and questionnaires are requested from the involved clinician, and participation has been high, since individual details are confidential. ;United States :The 1999 Institute of Medicine (IOM) report recommended "a nationwide mandatory reporting system … that provides for … collection of standardized information by state governments about adverse events that result in death or serious harm." Professional organizations, such as theIndividual patient disclosures
For a health care institution, disclosing an unanticipated event should be made as soon as possible. Some health care organizations may have a policy regarding the disclosure of unanticipated events. The amount of information presented to those affected is dependent on the family's readiness and the organization's culture. The employee disclosing the event to family requires support from risk management, patient safety officers and senior leadership. Disclosures are objectively documented in the medical record.Voluntary disclosure
In public surveys, a significant majority of those surveyed believe that health care providers should be required to report all serious medical errors publicly. However, reviews of the medical literature show little effect of publicly reported performance data on patient safety or the quality of care. Public reporting on the quality of individual providers or hospitals does not seem to affect selection of hospitals and individual providers. Some studies have shown that reporting performance data stimulates quality improvement activity in hospitals. As of 2012, only one in seven errors or accidents are reported, showing that most errors that happen are not reported.=United States
=Medical error Ethical standards of the Joint Commission on Accreditation of Healthcare Organizations (JCAHO), the
Performance In April 2008, consumer, employer and labor organizations announced an agreement with major physician organizations and health insurers on principles to measure and report doctors' performance on quality and cost.
=United Kingdom
= In the United Kingdom, whistleblowing is well recognised and is government sanctioned, as a way to protect patients by encouraging employees to call attention to deficient services. Health authorities are encouraged to put local policies in place to protect whistleblowers.Studies of patient safety
Numerous organizations, government branches, and private companies conduct research studies to investigate the overall health of patient safety in America and across the globe. Despite the shocking and widely publicized statistics on preventable deaths due to medical errors in America's hospitals, the 2006 National Healthcare Quality Report assembled by the Agency for Healthcare Research and Quality (AHRQ) had the following sobering assessment: A 2011 study of more than 1,000 patients with advanced colon cancer found that one in eight was treated with at least one drug regimen with specific recommendations against their use in the National Comprehensive Cancer Network guidelines. The study focused on three chemotherapy regimens that were not supported by evidence from prior clinical studies or clinical practice guidelines. One treatment was rated "insufficient data to support," one had been "shown to be ineffective," and one was supported by "no data, nor is there a compelling rationale." Many of the patients received multiple cycles of non-beneficial chemotherapy and some received two or more unproven treatments. Potential side effects for the treatments include hypertension, heightened risk of bleeding and bowel perforation.Organizations advocating patient safety
Several authors of the 1999 Institute of Medicine report revisited the status of their recommendations and the state of patient safety, five years after "To Err is Human". Discovering that patient safety had become a frequent topic for journalists, health care experts, and the public, it was harder to see overall improvements on a national level. What was noteworthy was the impact on attitudes and organizations. Few health care professionals now doubted that preventable medical injuries were a serious problem. The central concept of the report—that bad systems and not bad people lead to most errors—became established in patient safety efforts. A broad array of organizations now advance the cause of patient safety. For instance, in 2010 the principal European anaesthesiology organisations launched The Helsinki Declaration for Patient Safety in Anaesthesiology, which incorporates many of the principles described above.See also
* * * * * * * * * * * * * * * * * * * * * * of 2005 * *-Time 100 (2008) Most Influential People in the World; authored over 800 articles/chapters on patient safety; advisor to the World Health Organization's World Alliance for Patient Safety * * * * * * of accident causation in human systems * ''(SCID)'' *References
External links
CIMIT Center for Integration of Medicine and Innovative Technology - Nonprofit organizations together advocating for Patient safety
Institute for safety in Office Based Surgery
for the prevention of healthcare-induced harm
Patient Safety in the EU
Academic Center for Evidence-Based Practice (ACE)
Improvement Science Research Network (ISRN)
Beyond The Checklist: What Else Healthcare Can Learn From Aviation Teamwork and Safety
Institute of Medicine & Law
{{DEFAULTSORT:Patient Safety Evidence-based practices Health care quality