Methylprednisolone on:
[Wikipedia]
[Google]
[Amazon]
Methylprednisolone (Depo-Medrol, Medrol, Solu-Medrol) is a synthetic glucocorticoid, primarily prescribed for its anti-inflammatory and immunosuppressive effects. It is either used at low doses for chronic illnesses or used concomitantly at high doses during acute flares. Methylprednisolone and its derivatives can be administered orally or parenterally.
Regardless of route of administration, methylprednisolone integrates systemically as exhibited by its effectiveness to quickly reduce inflammation during acute flares. It is associated with many adverse reactions that require tapering off the drug as soon as the disease is under control. Serious side effects include iatrogenic
 The activation of the hypothalamic-pituitary axis (HPA axis) stimulates the production of endogenous glucocorticoids within the adrenal cortex. The HPA axis interprets stimuli (stress, inflammation and circadian cues) and transduces a corresponding physiochemical response. Glucocorticoids released in the blood, serve as a messenger by binding to glucocorticoid receptors in a wide distribution across the body, including the HPA axis itself. Thus, the physiological range of GCs is monitored by the negative feedback loop GCs exert on any portion of the HPA axis. Methylprednisolone structurally and functionally mimics endogenous corticoids and will act upon the HPA axis in a similar fashion.
The activation of the hypothalamic-pituitary axis (HPA axis) stimulates the production of endogenous glucocorticoids within the adrenal cortex. The HPA axis interprets stimuli (stress, inflammation and circadian cues) and transduces a corresponding physiochemical response. Glucocorticoids released in the blood, serve as a messenger by binding to glucocorticoid receptors in a wide distribution across the body, including the HPA axis itself. Thus, the physiological range of GCs is monitored by the negative feedback loop GCs exert on any portion of the HPA axis. Methylprednisolone structurally and functionally mimics endogenous corticoids and will act upon the HPA axis in a similar fashion.
 Methylprednisolone is approved for oral and parenteral administration. Methylprednisolone (Medrol) for oral administration is available in a tablet formulation in 2 mg, 4 mg, 8 mg, 16 mg or 32 mg strengths. Both methylprednisolone acetate (Depo-Medrol) and methylprednisolone succinate (Solu-Medrol) are approved for intramuscular injection. Depo-Medrol is additionally approved for intralesional, intra-articular, and soft tissue injections. Depo-Medrol is available as sterile aqueous solution in 20 mg/mL, 40 mg/mL, or 80 mg/mL strengths. Solu-Medrol is the only derivative of methylprednisolone that is approved for intravenous infusion, as the sterile powder is soluble in water and can be mixed with a diluent. Strengths vary from 40 mg to 2g.
Synthetic glucocorticoids are similar to endogenous steroids in metabolism, but differ in affinity for glucocorticoid and mineralocorticoid receptors, affinity for protein-binding, rate of elimination, and metabolic products.
Oral methylprednisolone is readily absorbed from the gastrointestinal tract with a bioavailability of 89.9%. In contrast to endogenous GCs, methylprednisolone does not bind to the glycoprotein transcortin (corticosteroid binding globulin, CBG) but does have moderate protein binding to albumin. Thus, pharmacokinetics of methylprednisolone is linear and show no dose dependency. Patients exhibiting low albumin concentrations are at risk for adverse effects during glucocorticoid therapy. Oral methylprednisolone has a moderate distribution into tissue at 1.38L/kg.
Methylprednisolone is primarily eliminated by hepatic metabolism and renal excretion of metabolites; with renal excretion of unchanged methylprednisolone at only 1.3–9.2%. Methylprednisolone can be interconverted with methylprednisone. Hepatic metabolism is mediated by 11 beta-hydroxysteroid dehydrogenases (11
Methylprednisolone is approved for oral and parenteral administration. Methylprednisolone (Medrol) for oral administration is available in a tablet formulation in 2 mg, 4 mg, 8 mg, 16 mg or 32 mg strengths. Both methylprednisolone acetate (Depo-Medrol) and methylprednisolone succinate (Solu-Medrol) are approved for intramuscular injection. Depo-Medrol is additionally approved for intralesional, intra-articular, and soft tissue injections. Depo-Medrol is available as sterile aqueous solution in 20 mg/mL, 40 mg/mL, or 80 mg/mL strengths. Solu-Medrol is the only derivative of methylprednisolone that is approved for intravenous infusion, as the sterile powder is soluble in water and can be mixed with a diluent. Strengths vary from 40 mg to 2g.
Synthetic glucocorticoids are similar to endogenous steroids in metabolism, but differ in affinity for glucocorticoid and mineralocorticoid receptors, affinity for protein-binding, rate of elimination, and metabolic products.
Oral methylprednisolone is readily absorbed from the gastrointestinal tract with a bioavailability of 89.9%. In contrast to endogenous GCs, methylprednisolone does not bind to the glycoprotein transcortin (corticosteroid binding globulin, CBG) but does have moderate protein binding to albumin. Thus, pharmacokinetics of methylprednisolone is linear and show no dose dependency. Patients exhibiting low albumin concentrations are at risk for adverse effects during glucocorticoid therapy. Oral methylprednisolone has a moderate distribution into tissue at 1.38L/kg.
Methylprednisolone is primarily eliminated by hepatic metabolism and renal excretion of metabolites; with renal excretion of unchanged methylprednisolone at only 1.3–9.2%. Methylprednisolone can be interconverted with methylprednisone. Hepatic metabolism is mediated by 11 beta-hydroxysteroid dehydrogenases (11
 Adverse reactions may overshadow the therapeutic effects of methylprednisolone.
Adverse reactions may overshadow the therapeutic effects of methylprednisolone.


Cushing's Syndrome
Cushing's syndrome is a collection of signs and symptoms due to prolonged exposure to glucocorticoids such as cortisol. Signs and symptoms may include high blood pressure, abdominal obesity but with thin arms and legs, reddish stretch marks, a ...
, hypertension, osteoporosis, diabetes, infection, and skin atrophy.
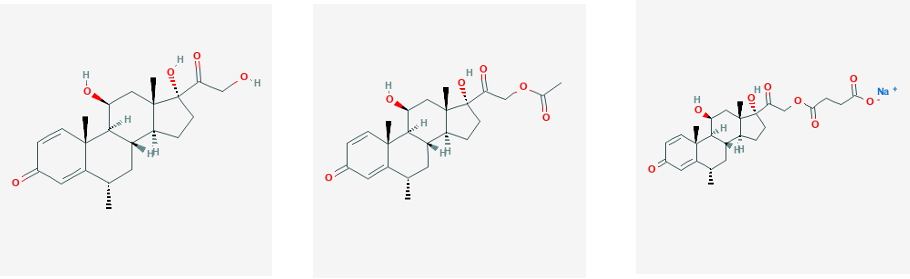
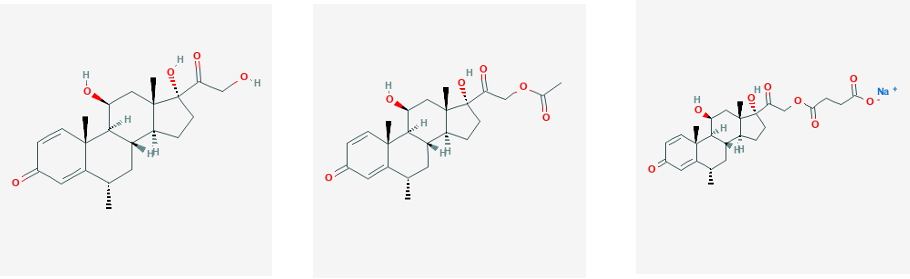
Chemically, methylprednisolone is a synthetic pregnane steroid hormone derived from hydrocortisone and prednisolone
Prednisolone is a steroid medication used to treat certain types of allergies, inflammatory conditions, autoimmune disorders, and cancers. Some of these conditions include adrenocortical insufficiency, high blood calcium, rheumatoid arth ...
. It belongs to a class of synthetic glucocorticoids and more generally, corticosteroid
Corticosteroids are a class of steroid hormones that are produced in the adrenal cortex of vertebrates, as well as the synthetic analogues of these hormones. Two main classes of corticosteroids, glucocorticoids and mineralocorticoids, are inv ...
s. It acts as a mineralocorticoid and glucocorticoid receptor agonist. In comparison to other exogenous glucocorticoids, methylprednisolone has a higher affinity to glucocorticoid receptors than to mineralocorticoid receptors.
Glucocorticoid's name was derived after the discovery of their involvement in regulating carbohydrate metabolism. The cellular functions of glucocorticoids, such as methylprednisolone, are now understood to regulate homeostasis, metabolism, development, cognition, and inflammation. They play a critical role in adapting and responding to environmental, physical and emotional stress.
Methylprednisolone was first synthesized and manufactured by The Upjohn Company (now Pfizer) and FDA approved in the United States in October 1957. In 2020, it was the 161st most commonly prescribed medication in the United States, with more than 3million prescriptions. Methylprednisolone is also on the World Health Organization's List of Essential Medicines for its effects against lymphoid leukemia.
Pharmacodynamics
Methylprednisolone is a synthetic glucocorticoid (GCs) that exhibits pleiotropic effects on a variety of physiological mechanisms. However, they have been prescribed extensively for their effects on inflammation and immunity. The effects of synthetic glucocorticoids, such as methylprednisolone, is dependent on its association with intracellular glucocorticoid receptors (GRs), and to a lesser extent, mineralocorticoid receptors (MRs). GRs are widely distributed in contrast to MRs that show a restricted tissue distribution. By this mechanism, the ligand-bound receptor translocate to the nucleus and modulate gene expression.Signal transduction
In the absence of endogenous or synthetic GCs, monomeric GRs are located in the cytoplasm and form multiprotein complexes withheat shock protein
Heat shock proteins (HSP) are a family of proteins produced by cells in response to exposure to stressful conditions. They were first described in relation to heat shock, but are now known to also be expressed during other stresses including expo ...
s (HSPs), immunophilins, and other chaperones such as src, and p23. The GR acts in a ligand-dependent manner, with the complex holding the GR in an inactive form with high specificity for the ligand. When methylprednisolone from the plasma or interstitial fluid diffuses passively across the cell membrane, it binds to the GR inducing a conformational change and GC-GR dimerization. It was previously thought that this conformational change was necessary to dissociate the multiprotein complex to allow the ligand bound receptor to translocate to the nucleus. However, recent studies have indicated that chaperones play a role in nuclear import. The now active methylprednisolone-GR complex can either transduce non-genomic changes in the cytoplasm or translocate to the nucleus and regulate transcriptional activity of target genes by direct, tethering or composite mechanisms.
Genomic signaling
Genomic mechanisms, regardless of which type, elicit responses with a slow onset and a slow dissipation. This is attributed to the duration of mRNA transcription and translation. Glucocorticoids have the ability to regulate roughly 100 to 1000 genes with specificity to cell-type. Three major mechanisms have described how the MP-GR complex alter gene expression by either binding to DNA or transcription modulators. One mechanism of genomic signaling occurs when the MP-GR complex directly binds to DNA sequences called glucocorticoid response elements (GREs). GREs are located in regulatory regions of target genes and mediate their transactivation or transrepression. For example, the activation of lipocortin 1 (ANAX1) negatively interferes with the production ofprostaglandin
The prostaglandins (PG) are a group of physiologically active lipid compounds called eicosanoids having diverse hormone-like effects in animals. Prostaglandins have been found in almost every tissue in humans and other animals. They are deriv ...
s and leukotriene
Leukotrienes are a family of eicosanoid inflammatory mediators produced in leukocytes by the oxidation of arachidonic acid (AA) and the essential fatty acid eicosapentaenoic acid (EPA) by the enzyme arachidonate 5-lipoxygenase.
Leukotrienes ...
s, known pro-inflammatory signals. Likewise, negative GREs (nGREs) are responsible for repressing genes involved in immune cell activation.
Post transcriptional modifications
Post translational modifications (PTMs) also contribute to methylprednisolone signaling and can produce genomic and non-genomic effects. The GR has contains several sites for phosphorylation, sumoylation, ubiquitination, and acetylation that primarily occurs after intracellular methylprednisolone binding to the GR.Kino T, Chrousos GP. Acetylation-mediated epigenetic regulation of glucocorticoid receptor activity: circadian rhythm-associated alterations of glucocorticoid actions in target tissues. ''Mol Cell Endocrinol''. 2011;336(1-2):23-30. PTMs modulate many functions including nuclear translocation, strength and duration of receptor signaling and cofactor interaction. A specific example is the deacetylation by histone deacetylase 2 (HDACe) was necessary for transrepression of NF-κB.Non-genomic signaling
The mechanisms of non-genomic signaling are distinct from genomic signaling, yet mediate similar pathways and provide therapeutic relevance. These mechanisms are characterized as having a rapid onset (less than 15 minutes), because they do not rely on time-consuming transcription or translation and are not modified by inhibitors of transcription. Methylprednisolone induced non-genomic signaling is classified by three mechanisms: (1) cytoplasmic glucocorticoid receptor (cGR)-mediated non-genomic effects, (2) membrane-bound glucocorticoid receptor (mGR) non-genomic effects, and (3) physiochemical interactions with cellular membranes (non-specific non-genomic effects). Proteins that dissociate from the activated GC-cGR complex, initiate intracellular transcription-independent mechanisms. It is evidence that dissociated SRC is responsible for inhibiting the release of arachidonic acid (AA) from cell membrane phospholipids. AA is required for the synthesis of inflammatory mediators (prostaglandins and leukotrienes) and thus AA inhibition mediates several important pathways such as cellular growth, metabolism and inflammation. Previous studies identified mGRs in lymphoma cells, but it wasn't until 2004 that mGRs were identified in human peripheral mononuclear cells. The prevalence of mGRs ranges per cell type, with the highest concentration in B lymphocytes at up to 12.3%, up to 9.2% in monocytes, and absent from T lymphocytes. Studies have shown a positive correlation between the mGR-positive cells and disease related activity. There are no proven signaling pathways associated with mGR at this time. Some researchers hypothesize that high disease activity activates mGR expression and upon administering methylprednisolone, creates a negative feedback loop by inducing apoptosis. High concentrations of methylprednisolone intercalate in plasma and mitochondrial cellular membranes. This association changes physiochemical properties of the membrane; activating membrane proteins, altering cellular functions and ultimately influencing cation transport through the plasma membrane and stimulating the proton leak across the inner mitochondrial membrane. Hindered oxidative phosphorylation compromises ATP production, a major energy source for cellular energy metabolism and immune function. In vivo studies of Con-A stimulated thymocytes (in rats) and human immune cells that were administered high doses of methylprednisolone has been shown to inhibit respiration in a dose-dependent manner, inhibit plasma calcium and sodium uptake, and increase cytoplasmic calcium concentration. The summative process is as follows: Methylprednisolone intercalates in the plasma membrane, causes physiochemical changes, activates membrane proteins that inhibit plasma calcium and sodium uptake (mimicking an energy deficit state). ATP consumption drops (resembled by inhibited respiration), resulting in protein permeability at the inner mitochondrial membrane and uncoupling of oxidative phosphorylation. Of notable importance, DNA/RNA synthesis was not hindered. The dependency of house keeping cells and immune cells on ATP, results in immunosuppression during ATP deficit. Specific immune functions effected by this process are cytokinesis, migration, phagocytosis, antigen processing and presenting, antibody synthesis, cytotoxicity and regulation.The HPA axis
 The activation of the hypothalamic-pituitary axis (HPA axis) stimulates the production of endogenous glucocorticoids within the adrenal cortex. The HPA axis interprets stimuli (stress, inflammation and circadian cues) and transduces a corresponding physiochemical response. Glucocorticoids released in the blood, serve as a messenger by binding to glucocorticoid receptors in a wide distribution across the body, including the HPA axis itself. Thus, the physiological range of GCs is monitored by the negative feedback loop GCs exert on any portion of the HPA axis. Methylprednisolone structurally and functionally mimics endogenous corticoids and will act upon the HPA axis in a similar fashion.
The activation of the hypothalamic-pituitary axis (HPA axis) stimulates the production of endogenous glucocorticoids within the adrenal cortex. The HPA axis interprets stimuli (stress, inflammation and circadian cues) and transduces a corresponding physiochemical response. Glucocorticoids released in the blood, serve as a messenger by binding to glucocorticoid receptors in a wide distribution across the body, including the HPA axis itself. Thus, the physiological range of GCs is monitored by the negative feedback loop GCs exert on any portion of the HPA axis. Methylprednisolone structurally and functionally mimics endogenous corticoids and will act upon the HPA axis in a similar fashion.
Pharmacokinetics
 Methylprednisolone is approved for oral and parenteral administration. Methylprednisolone (Medrol) for oral administration is available in a tablet formulation in 2 mg, 4 mg, 8 mg, 16 mg or 32 mg strengths. Both methylprednisolone acetate (Depo-Medrol) and methylprednisolone succinate (Solu-Medrol) are approved for intramuscular injection. Depo-Medrol is additionally approved for intralesional, intra-articular, and soft tissue injections. Depo-Medrol is available as sterile aqueous solution in 20 mg/mL, 40 mg/mL, or 80 mg/mL strengths. Solu-Medrol is the only derivative of methylprednisolone that is approved for intravenous infusion, as the sterile powder is soluble in water and can be mixed with a diluent. Strengths vary from 40 mg to 2g.
Synthetic glucocorticoids are similar to endogenous steroids in metabolism, but differ in affinity for glucocorticoid and mineralocorticoid receptors, affinity for protein-binding, rate of elimination, and metabolic products.
Oral methylprednisolone is readily absorbed from the gastrointestinal tract with a bioavailability of 89.9%. In contrast to endogenous GCs, methylprednisolone does not bind to the glycoprotein transcortin (corticosteroid binding globulin, CBG) but does have moderate protein binding to albumin. Thus, pharmacokinetics of methylprednisolone is linear and show no dose dependency. Patients exhibiting low albumin concentrations are at risk for adverse effects during glucocorticoid therapy. Oral methylprednisolone has a moderate distribution into tissue at 1.38L/kg.
Methylprednisolone is primarily eliminated by hepatic metabolism and renal excretion of metabolites; with renal excretion of unchanged methylprednisolone at only 1.3–9.2%. Methylprednisolone can be interconverted with methylprednisone. Hepatic metabolism is mediated by 11 beta-hydroxysteroid dehydrogenases (11
Methylprednisolone is approved for oral and parenteral administration. Methylprednisolone (Medrol) for oral administration is available in a tablet formulation in 2 mg, 4 mg, 8 mg, 16 mg or 32 mg strengths. Both methylprednisolone acetate (Depo-Medrol) and methylprednisolone succinate (Solu-Medrol) are approved for intramuscular injection. Depo-Medrol is additionally approved for intralesional, intra-articular, and soft tissue injections. Depo-Medrol is available as sterile aqueous solution in 20 mg/mL, 40 mg/mL, or 80 mg/mL strengths. Solu-Medrol is the only derivative of methylprednisolone that is approved for intravenous infusion, as the sterile powder is soluble in water and can be mixed with a diluent. Strengths vary from 40 mg to 2g.
Synthetic glucocorticoids are similar to endogenous steroids in metabolism, but differ in affinity for glucocorticoid and mineralocorticoid receptors, affinity for protein-binding, rate of elimination, and metabolic products.
Oral methylprednisolone is readily absorbed from the gastrointestinal tract with a bioavailability of 89.9%. In contrast to endogenous GCs, methylprednisolone does not bind to the glycoprotein transcortin (corticosteroid binding globulin, CBG) but does have moderate protein binding to albumin. Thus, pharmacokinetics of methylprednisolone is linear and show no dose dependency. Patients exhibiting low albumin concentrations are at risk for adverse effects during glucocorticoid therapy. Oral methylprednisolone has a moderate distribution into tissue at 1.38L/kg.
Methylprednisolone is primarily eliminated by hepatic metabolism and renal excretion of metabolites; with renal excretion of unchanged methylprednisolone at only 1.3–9.2%. Methylprednisolone can be interconverted with methylprednisone. Hepatic metabolism is mediated by 11 beta-hydroxysteroid dehydrogenases (11eta
Eta (uppercase , lowercase ; grc, ἦτα ''ē̂ta'' or ell, ήτα ''ita'' ) is the seventh letter of the Greek alphabet, representing the close front unrounded vowel . Originally denoting the voiceless glottal fricative in most dialects, ...
HSD) and 20-ketosteroid reductases. Methylprednisolone undergoes renal excretion of hydrophilic inactive metabolites, including 20-carboxymelthylprednisolone and 6eta
Eta (uppercase , lowercase ; grc, ἦτα ''ē̂ta'' or ell, ήτα ''ita'' ) is the seventh letter of the Greek alphabet, representing the close front unrounded vowel . Originally denoting the voiceless glottal fricative in most dialects, ...
hydroxy-20 lphahydroxymethylprednisolone.
Medical uses
As stated previously, the primary use of methylprednisolone is to suppress inflammatory and immune responses. Methylprednisolone achieves this primarily by regulating the number and function of leukocytes, cytokines and chemokines. Its widespread inflammatory control is conducive in use across multiple disorders regardless of pathology. Methylprednisolone is commonly prescribed as short-term therapy for acute flares, as seen with acute gouty arthritis. It can be prescribed during on-going therapy in lower doses contingent upon monitorization of adverse effects. Dosage strength and formulation are optimized per medical use.Asthma
In 2001–2002, 11.4% of patients diagnosed with asthma and seen at an outpatient visit were prescribed oral corticosteroids as a long-term control therapy. The National Asthma Education and Prevention Program (NAEPP) indicates systemic methylprednisolone in both short and long term therapies to quickly control and to suppress persistent asthma, respectively. For exacerbations that result in a visit to the Emergency Department (ED), oral methylprednisolone is preferred over intravenous administration, unless there are issues with adherence or vomiting. Oral methylprednisolone is less invasive and studies have shown that equivalent efficacy compared to intravenous methylprednisolone. Dosage above 60–80 mg/day or 2 mg/kg/day is not recommended as it has not been shown to alter pulmonary function, rate of admission, or length of stay in the hospital compared to lower doses. Following ED discharge, it is advised to prescribed a five-day course of methylprednisolone to decrease the probability of relapse or withdrawal symptoms.Rheumatic diseases
Methylprednisolone is used to treat several rheumatic diseases, such as Systemic Lupus Erythematosus (SLE) and Rheumatoid Arthritis (RA). Methylprednisolone dosage and administration for these diseases is highly variable due to varied pathophysiology between the diseases and within patients diagnosed with a given disease. In Lupus Nephritis, a common manifestation of SLE, patients are often prescribed methylprednisolone concomitantly with immunosuppressants. Severe manifestations are often treated withCyclophosphamide
Cyclophosphamide (CP), also known as cytophosphane among other names, is a medication used as chemotherapy and to suppress the immune system. As chemotherapy it is used to treat lymphoma, multiple myeloma, leukemia, ovarian cancer, breast cancer ...
or Rituximab and three doses of methylprednisolone IV-pulse treatment (as recommended by ACR guidelines) prior to switching to oral prednisolone and azathioprine for maintenance.
Intra-articular corticosteroid injections (IACI) are a second line therapy to relieve joint pain resulting from rheumatoid arthritis.Habib, G.S. Systemic effects of intra-articular corticosteroids. Clin. Rheumatol. 2009, 28, 749–756. It is most commonly injected into the joints of the knees and shoulders. Although the injection is local, studies have shown systemic absorption as evidenced by beneficial effects on distant joints. In an attempt to minimize HPA suppression, FDA guidelines have restricted IACIs to three per year, with a minimum of 30 days in between injections.
Primary or secondary adrenocortical insufficiency
Methylprednisolone is not typically recommended for primary or secondary adrenocortical insufficiency compared to other corticosteroids which have a higher affinity for mineralocorticoid receptor and salt retaining properties.Labeled indications
The labeled indications below are categorized by route of administration then by medical discipline.Oral methylprednisolone
* Allergy and Immunology: angioneurotic edema,asthma
Asthma is a long-term inflammatory disease of the airways of the lungs. It is characterized by variable and recurring symptoms, reversible airflow obstruction, and easily triggered bronchospasms. Symptoms include episodes of wheezing, co ...
, urticaria
Hives, also known as urticaria, is a kind of skin rash with red, raised, itchy bumps. Hives may burn or sting. The patches of rash may appear on different body parts, with variable duration from minutes to days, and does not leave any long-last ...
, seasonal or perennial allergic rhinitis, drug hypersensitivity reactions, and serum sickness.
* Dermatology: toxic epidermal necrolysis, atopic dermatitis
Atopic dermatitis (AD), also known as atopic eczema, is a long-term type of inflammation of the skin ( dermatitis). It results in itchy, red, swollen, and cracked skin. Clear fluid may come from the affected areas, which often thickens over tim ...
, contact dermatitis
Contact dermatitis is a type of acute or chronic inflammation of the skin caused by exposure to chemical or physical agents. Symptoms of contact dermatitis can include itchy or dry skin, a red rash, bumps, blisters, or swelling. These rashes are ...
, pemphigus
Pemphigus ( or ) is a rare group of blistering autoimmune diseases that affect the skin and mucous membranes.
The name is derived from the Greek root ''pemphix'', meaning "pustule".
In pemphigus, autoantibodies form against desmoglein, whic ...
, erythema multiforme
Erythema multiforme (EM) is a skin condition that appears with red patches evolving into target lesions, typically on both hands.
It is a type of erythema possibly mediated by deposition of immune complexes (mostly IgM-bound complexes) in the ...
, Steven-Johnson syndrome, bullous dermatitis herpetiformis, severe seborrheic dermatitis, exfoliative dermatitis, mycosis fungoides
Mycosis fungoides, also known as Alibert-Bazin syndrome or granuloma fungoides, is the most common form of cutaneous T-cell lymphoma. It generally affects the skin, but may progress internally over time. Symptoms include rash, tumors, skin lesions ...
, and severe psoriasis
Psoriasis is a long-lasting, noncontagious autoimmune disease characterized by raised areas of abnormal skin. These areas are red, pink, or purple, dry, itchy, and scaly. Psoriasis varies in severity from small, localized patches to comple ...
.
* Endocrinology: congenital adrenal hyperplasia
Congenital adrenal hyperplasia (CAH) is a group of autosomal recessive disorders characterized by impaired cortisol synthesis. It results from the deficiency of one of the five enzymes required for the synthesis of cortisol in the adrenal cortex ...
, hypercalcemia associated with cancer, nonsuppurative thyroiditis, and primary or secondary adrenocortical insufficiency.
* Gastroenterology: inflammatory bowel disease
Inflammatory bowel disease (IBD) is a group of inflammatory conditions of the colon and small intestine, Crohn's disease and ulcerative colitis being the principal types. Crohn's disease affects the small intestine and large intestine, as well ...
and ulcerative colitis
Ulcerative colitis (UC) is a long-term condition that results in inflammation and ulcers of the colon and rectum. The primary symptoms of active disease are abdominal pain and diarrhea mixed with blood (hematochezia). Weight loss, fever, and ...
.
* Hematology: acquired (autoimmune) hemolytic anemia, idiopathic thrombocytopenic purpura
Immune thrombocytopenic purpura (ITP), also known as idiopathic thrombocytopenic purpura or immune thrombocytopenia, is a type of thrombocytopenic purpura defined as an isolated low platelet count with a normal bone marrow in the absence of oth ...
, secondary thrombocytopenia, erythroblastopenia, leukemia
Leukemia ( also spelled leukaemia and pronounced ) is a group of blood cancers that usually begin in the bone marrow and result in high numbers of abnormal blood cells. These blood cells are not fully developed and are called ''blasts'' or ...
, lymphoma
Lymphoma is a group of blood and lymph tumors that develop from lymphocytes (a type of white blood cell). In current usage the name usually refers to just the cancerous versions rather than all such tumours. Signs and symptoms may include en ...
and congenital (erythroid) hypoplastic anemia.
* Pulmonary: aspiration pneumonitis, chronic beryllium disease, eosinophilic pneumonia
Eosinophilic pneumonia is a disease in which an eosinophil, a type of white blood cell, accumulates in the lungs. These cells cause disruption of the normal air spaces (alveoli) where oxygen is extracted from the atmosphere. Several different kin ...
, symptomatic sarcoidosis
Sarcoidosis (also known as ''Besnier-Boeck-Schaumann disease'') is a disease involving abnormal collections of inflammatory cells that form lumps known as granulomata. The disease usually begins in the lungs, skin, or lymph nodes. Less commonly af ...
, and pulmonary tuberculosis
Tuberculosis (TB) is an infectious disease usually caused by ''Mycobacterium tuberculosis'' (MTB) bacteria. Tuberculosis generally affects the lungs, but it can also affect other parts of the body. Most infections show no symptoms, i ...
in conjunction with antituberculosis chemotherapy.
* Nephrology: nephrotic syndrome
Nephrotic syndrome is a collection of symptoms due to kidney damage. This includes protein in the urine, low blood albumin levels, high blood lipids, and significant swelling. Other symptoms may include weight gain, feeling tired, and foamy ...
, idiopathic type or secondary to lupus nephritis.
* Neurology: multiple sclerosis
Multiple (cerebral) sclerosis (MS), also known as encephalomyelitis disseminata or disseminated sclerosis, is the most common demyelinating disease, in which the insulating covers of nerve cells in the brain and spinal cord are damaged. This ...
.
* Ophthalmology: scleritis
Scleritis is a serious inflammatory disease that affects the white outer coating of the eye, known as the sclera. The disease is often contracted through association with other diseases of the body, such as granulomatosis with polyangiitis or ...
, retinal vasculitis, uveitis
Uveitis () is inflammation of the uvea, the pigmented layer of the eye between the inner retina and the outer fibrous layer composed of the sclera and cornea. The uvea consists of the middle layer of pigmented vascular structures of the eye and in ...
, choroiditis, iritis, iridocyclitis, keratitis
Keratitis is a condition in which the eye's cornea, the clear dome on the front surface of the eye, becomes inflamed. The condition is often marked by moderate to intense pain and usually involves any of the following symptoms: pain, impaired e ...
, optic neuritis
Optic neuritis describes any condition that causes inflammation of the optic nerve; it may be associated with demyelinating diseases, or infectious or inflammatory processes.
It is also known as optic papillitis (when the head of the optic nerv ...
, allergic conjunctivitis, allergic corneal marginal ulcers, herpes zoster ophthalmicus, sympathetic ophthalmia, and chorioretinitis.
* Rheumatology: rheumatoid arthritis
Rheumatoid arthritis (RA) is a long-term autoimmune disorder that primarily affects joints. It typically results in warm, swollen, and painful joints. Pain and stiffness often worsen following rest. Most commonly, the wrist and hands are inv ...
, rheumatic carditis, acute gouty arthritis, ankylosing spondylitis
Ankylosing spondylitis (AS) is a type of arthritis characterized by long-term inflammation of the joints of the spine typically where the spine joins the pelvis. Occasionally areas affected may include other joints such as the shoulders or hi ...
, dermatomyositis
Dermatomyositis (DM) is a long-term inflammatory disorder which affects skin and the muscles. Its symptoms are generally a skin rash and worsening muscle weakness over time. These may occur suddenly or develop over months. Other symptoms may inc ...
and polymyositis
Polymyositis (PM) is a type of chronic inflammation of the muscles (inflammatory myopathy) related to dermatomyositis and inclusion body myositis. Its name means "inflammation of many muscles" ('' poly-'' + '' myos-'' + '' -itis''). The inflam ...
, psoriatic arthritis
Psoriatic arthritis is a long-term inflammatory arthritis that occurs in people affected by the autoimmune disease psoriasis. The classic feature of psoriatic arthritis is swelling of entire fingers and toes with a sausage-like appearance. T ...
, systemic lupus erythematosus
Lupus, technically known as systemic lupus erythematosus (SLE), is an autoimmune disease in which the body's immune system mistakenly attacks healthy tissue in many parts of the body. Symptoms vary among people and may be mild to severe. Commo ...
, acute and subacute bursitis
Bursitis is the inflammation of one or more bursae (fluid filled sacs) of synovial fluid in the body. They are lined with a synovial membrane that secretes a lubricating synovial fluid. There are more than 150 bursae in the human body. The bursae ...
, synovitis of osteoarthritis, post-traumatic osteoarthritis, and epicondylitis Epicondylitis is a type of musculoskeletal disorder that refers to an inflammation of an epicondyle. It is caused by repetitive motion. In athletes, it is linked to poor technique. Nonsurgical treatment is effective in approximately 95% of cases.
T ...
.
* Miscellaneous: trichinosis with neurologic or myocardial involvement.
Parenteral methylprednisolone
* Intra-articular or soft tissue injections: acute gouty arthritis, acute and subacute bursitis, acute tenosynovitis, epicondylitis, and synovitis of osteoarthritis. * Intralesional injections:alopecia areata
Alopecia areata, also known as spot baldness, is a condition in which hair is lost from some or all areas of the body. Often, it results in a few bald spots on the scalp, each about the size of a coin. Psychological stress and illness are pos ...
, discoid lupus erythematosus
Discoid lupus erythematosus is the most common type of chronic cutaneous lupus (CCLE), an autoimmune skin condition on the lupus erythematosus spectrum of illnesses. It presents with red, painful, inflamed and coin-shaped patches of skin with a sc ...
, keloid
Keloid, also known as keloid disorder and keloidal scar,
is the formation of a type of scar which, depending on its maturity, is composed mainly of either type III (early) or type I (late) collagen. It is a result of an overgrowth of granulation ...
s, granuloma annulare, lichen planus, lichen simplex chronicus
Lichen simplex chronicus (LSC) is thick leathery skin with exaggerated skin markings caused by sudden itching and excessive rubbing and scratching. It generally results in small bumps, patches, scratch marks and scale. It typically affects the ...
, psoriatic plaques, necrobiosis lipoidica diabeticorum.
* Intramuscular injections are prescribed treat many of the same conditions indicated for oral administration. Intramuscular injections are administered as an alternative to oral therapy.
Off-label indications
Some of the off-label indications of methylprednisolone include acutespinal cord injury
A spinal cord injury (SCI) is damage to the spinal cord that causes temporary or permanent changes in its function. Symptoms may include loss of muscle function, sensation, or autonomic function in the parts of the body served by the spinal cor ...
, acute respiratory distress syndrome
Acute respiratory distress syndrome (ARDS) is a type of respiratory failure characterized by rapid onset of widespread inflammation in the lungs. Symptoms include shortness of breath (dyspnea), rapid breathing (tachypnea), and bluish skin colo ...
, alcoholic hepatitis
Alcoholic hepatitis is hepatitis (inflammation of the liver) due to excessive intake of alcohol. Patients typically have a history of at least 10 years of heavy alcohol intake, typically 8-10 drinks per day. It is usually found in association with ...
, hormonal resuscitation in cadaveric organ recovery, and chronic obstructive pulmonary disease
Chronic obstructive pulmonary disease (COPD) is a type of progressive lung disease characterized by long-term respiratory symptoms and airflow limitation. The main symptoms include shortness of breath and a cough, which may or may not produce ...
.
Available forms
Footnotes: 1Signifies varying strengths of available forms. Is not indicative of frequency nor daily cumulative dose; varies per patient and condition. 2Benzyl alcohol should not to be used on neonates 3Preservative free formulationContraindications
Methylprednisolone should not be taken orally by people who have systemic fungal infections, with the exception of Depo-Medrol when administered as an intra-articular injection for localized joint conditions. Methylprednisolone is contraindicated in those with known hypersensitivity to methylprednisolone or its components Steroids should be used with caution in patients with ulcerative colitis, heart disease or hypertension, peptic ulcer, renal insufficiency, osteoporosis, myasthenia gravis, glaucoma, and diabetes. Psychic manifestations may appear while taking methylprednisolone, ranging from euphoria, insomnia, personality changes to depression. Caution is required for patients with predisposed psychoses, as psychotic tendencies may be exacerbated while taking corticosteroids. Solu-Medrol 40 mg dosage contains lactose monohydrate produced from cow's milk; It should not be taken by anyone with known hypersensitivity to dairy products or its components. Severe medical events have been associated with epidural administration of Solu-Medrol and Depo-Medrol, including spinal cord infarction, paraplegia, quadriplegia, cortical blindness and stroke. Intramuscular injections should not be administered to those with idiopathic thrombocytopenic purpura. Formulations of Solu-Medrol and Depo-Medrol containing benzyl alcohol are contraindicated for use in premature infants. Exposure of neural tissue to excessive amounts of benzyl alcohol has been associated with toxicity and in rare events has resulted in death.Adverse reactions
 Adverse reactions may overshadow the therapeutic effects of methylprednisolone.
Adverse reactions may overshadow the therapeutic effects of methylprednisolone.
Central nervous system
There is minimal clinical diagnostic criteria to define the psychic adverse effects (PAE) associated with methylprednisolone use in patients with systemic lupus erythematosus (SLE). The prevalence varies from 1.3 to 62% of adult treated patients. The type and severity of neuropsychiatric symptoms also varies significantly between patients, with 33% of patients reporting mild to moderate PAE and 5-10% reporting severe PAE. Methylprednisolone dose and duration have been implicated in PAE development. 20 mg/day of prednisone (16 mg/day of methylprednisolone) is the threshold dosage for PAE development agreed upon by many studies. Short-term pulse IV therapy at high doses is associated with rapid onset of manic and hypomanic symptoms, whereas long term therapy gives rise to depressive symptoms (suicide attempts infrequent). PAE are reversible with treatment reduction or discontinuation.Metabolic and endocrine
Iatrogenic Cushing's Syndrome is a direct complication of glucocorticoid therapy, and the most common cause of exogenous Cushing's Syndrome. Clinical features of Cushing's Syndrome is inclusive of many adverse effects in glucocorticoid therapy. Traditional symptoms include weight gain, myopathy, osteoporosis, increased risk of infection, hypertension and psychological effect. Fat deposition is centralized on the trunk, in between shoulders ("buffalo hump"), and on the face ("moon face"). Patient education and provider monitoring is the first step in recognizing and diagnosing Iatrogenic Cushing's Syndrome. Exogenous glucocorticoids suppressadrenocorticotropic hormone
Adrenocorticotropic hormone (ACTH; also adrenocorticotropin, corticotropin) is a polypeptide tropic hormone produced by and secreted by the anterior pituitary gland. It is also used as a medication and diagnostic agent. ACTH is an important c ...
(ATCH) production, which can be verified by AM biochemical analysis. The onset of side effects varies; neuropsychiatric symptoms can arise within a few hours, while osteoporosis would take months to develop.
The metabolic effects of taking methylprednisolone involve the continuous breakdown of proteins for gluconeogenesis increase necessity for insulin. This results in hyperlipidemia, weight gain, myopathy that may prompt a patient to cease treatment.
Infections
: ''See: Glucocorticoids § Immunodeficiency'' The Immunodeficiency section tabulates known pathogens of concern in glucocorticoid induced immunodeficiency.Musculoskeletal
Osteoporosis is a type of bone disease characterized by a loss of bone density, mass and architecture that leaves a patient susceptible to fractures. The World Health Organization (WHO) defines osteoporosis in caucasian postmenopausal women as a bone mineral density (BMD) and a T-score of -2.5 or less. The prevalence of osteoporosis in patients with SLE varies geographically and some attribute it to BMD and T-score diagnostic appropriateness. British 10.3%, Chinese 21.7%The Canadian Clinical Practice Guidelines and The American College of Rheumatology have switched to using a Z-score as a diagnostic marker for osteoporosis but have failed to find a clinical diagnostic threshold. Additionally, a UK-based study showed that BMD may underrepresent a patient with SLE, as their risk for fractures is 22% higher than the healthy individual. Exogenous corticosteroids induce osteoporosis by increasing bone resorption and reducing bone formation. Bone loss can be pronounced within the first few months of initiating methylprednisolone with a steady decrease with chronic use. Trabecular bone loss in the lumbar spine precedes cortical bone loss in the femoral neck.Exhaustive list
Allergic: allergic or hypersensitivity reactions, anaphylactoid reaction, anaphylaxis, and urticaria. Cardiovascular: hypertension, congestive heart failure in susceptible patients, premature atherosclerotic disease, arrhythmias, and possible hyperlipidemia. Dermatologic: impaired wound healing, petechiae and ecchymoses, thinning of the skin, facial erythema, and increased sweating. Endocrine: Cushingoid features, growth suppression in children, secondary adrenocortical and pituitary unresponsiveness, menstrual irregularities, decreased carbohydrate intolerance, and latent diabetes mellitus. In patients with diabetes, increased requirements of insulin or oral hypoglycemic agents. Fluid and electrolyte disturbances: sodium retention, fluid retention, potassium loss, hypokalemic alkalosis, or congestive heart failure in susceptible patients. Gastrointestinal: peptic ulcer, pancreatitis, abdominal distention, and ulcerative esophagitis. Metabolic: protein catabolism which causes negative nitrogen balance. Musculoskeletal: muscle weakness, loss of muscle mass, steroid myopathy, osteoporosis, tendon rupture (especially Achilles), vertebral compression fractures, aseptic necrosis of femoral and humeral heads, and pathologic fracture of long bones. Neurological: increased intracranial pressure with papilledema, convulsions, vertigo, and headache. Ophthalmic: posterior sub-capsular cataracts, increased intraocular pressure, glaucoma, and exophthalmos.Withdrawal
Feedback of the exogenous glucocorticoids at the hypothalamic–pituitary–adrenal (HPA) axis inhibits the secretion of the corticotropin-releasing hormone (CRH) and theadrenocorticotropic hormone
Adrenocorticotropic hormone (ACTH; also adrenocorticotropin, corticotropin) is a polypeptide tropic hormone produced by and secreted by the anterior pituitary gland. It is also used as a medication and diagnostic agent. ACTH is an important c ...
(ATCH) at the hypothalamus and pituitary glands, respectively. Prolonged suppression leads to inadequate responses to physical and emotional stresses, such as illness and trauma. Suppression of ATCH may result in adrenal hypoplasia or secondary adrenal gland atrophy within 6 weeks of methylprednisolone therapy, leaving a patient at risk for developing life-threatening adrenal insufficiency crisis. Factors that contribute to the extent of HPA axis suppression include steroid hormone potency (type of compound and route of administration), cumulative dose, duration of treatment and concomitant drug use. Any individual who has taken steroid hormones for 2+ weeks is at risk for developing HPA axis suppression. t Systemic methylprednisolone risk has been marked as moderate within the class of synthetic glucocorticoids.
Consult with your physician prior to discontinuing methylprednisolone for any reason. Abrupt termination of the drug commonly causes transient non-specific symptoms such as loss of appetite, upset stomach, vomiting, drowsiness, confusion, headache, fever, joint and muscle pain, peeling skin, and weight loss. These symptoms can be attributed to steroid withdrawal syndrome, adrenal insufficiency or disease relapse. Those who have been taking methylprednisolone as a long-term treatment may be gradually be tapered off to minimize withdrawal symptoms and potential for relapse. If symptoms are exacerbated, temporarily increasing methylprednisolone dosage has shown clinical relevancy. Studies retesting patients upon methylprednisolone withdrawal, showed persistent adrenal insufficiency, with one study showing 15% after 3 years. However, there was a wide range of prevalence and lack of uniformity in the follow-up timeline.
Drug interactions
Caution is advised when taking methylprednisolone concurrently with the medications described below. Enzyme inducers All drugs that fall within the class of enzyme inducers increase the clearance and decrease the half-life of methylprednisolone when co-administered.Phenobarbital
Phenobarbital, also known as phenobarbitone or phenobarb, sold under the brand name Luminal among others, is a medication of the barbiturate type. It is recommended by the World Health Organization (WHO) for the treatment of certain types of ep ...
, phenytoin
Phenytoin (PHT), sold under the brand name Dilantin among others, is an anti-seizure medication. It is useful for the prevention of tonic-clonic seizures (also known as grand mal seizures) and focal seizures, but not absence seizures. The in ...
, rifampin, carbamazepine and barbiturates, increase hepatic enzymes and rate of elimination, thus reducing the immunosuppressive effect of methylprednisolone. Increased dosages may be required to achieve desired effect of methylprednisolone.
Cytochrome P450 (CYP) 3A4 inhibitors
Troleandomycin
Troleandomycin (TAO for short) is a macrolide antibiotic. It was sold in Italy (branded Triocetin) and Turkey (branded Tekmisin). It is no longer sold in Italy as of 2018.
The drug's mode of action is to bind to the ribosome, specifically in ...
, ketoconazole
Ketoconazole, sold under the brand name Nizoral among others, is an antiandrogen and antifungal medication used to treat a number of fungal infections. Applied to the skin it is used for fungal skin infections such as tinea, cutaneous ca ...
, and Clarithromycin inhibit metabolism; and may decrease rate of elimination and increase half-life of methylprednisolone. Dosages should be decreased accordingly to avoid side effects. Another CYP 3A4 inhibitor, grapefruit juice, prolongs half-life of oral methylprednisolone.
Oral contraceptives
Oral contraceptives inhibit oxidative processes, as highlighted by its ability to decrease methylprednisolone clearance.
P-glycoprotein inhibitors
Methylprednisolone is shown to be a substrate of P-glycoprotein; its inhibition is thought to increase methylprednisone absorption and distribution. No clinical relevance has been linked.
Ciclosporin, tacrolimus, sirolimus (Rapamycin)
Methylprednisolone and cyclosporin
Ciclosporin, also spelled cyclosporine and cyclosporin, is a calcineurin inhibitor, used as an immunosuppressant medication. It is a natural product. It is taken orally or intravenously for rheumatoid arthritis, psoriasis, Crohn's disea ...
inhibit metabolism and therefore increase the likelihood of experiencing side effects associated with either of the individual drugs. In addition to known individual side effects, convulsions have been reported.
Cox1 inhibitors
Methylprednisolone may increase rate of elimination with chronic high dose aspirin
Aspirin, also known as acetylsalicylic acid (ASA), is a nonsteroidal anti-inflammatory drug (NSAID) used to reduce pain, fever, and/or inflammation, and as an antithrombotic. Specific inflammatory conditions which aspirin is used to treat inc ...
. Patient's are susceptible to increased salicylate serum levels or salicylate toxicity upon termination of methylprednisolone. Excessive caution should be taken when prescribing methylprednisolone and aspirin to patients with hypoprothrombinemia.
Anticoagulants
Anticoagulant
Anticoagulants, commonly known as blood thinners, are chemical substances that prevent or reduce coagulation of blood, prolonging the clotting time. Some of them occur naturally in blood-eating animals such as leeches and mosquitoes, where t ...
s exhibit variable interactions; monitoring coagulation indices is recommended to achieve the desired effect.
Physical properties
Oral methylprednisolone (Medrol) and its derivatives are a white, odorless crystalline powder. Its solubility ranges from practically insoluble in water, very slightly soluble in ether, sightly soluble in acetone and chloroform to sparingly soluble in alcohol, dioxane and methanol. Methylprednisolone acetate suspension (Depo-Medrol) is a 6-methyl derivative of prednisolone that melts at 215 degrees Celsius with some decomposition. Methylprednisolone sodium succinate (Solu-Medrol) is the sodium succinate ester of methylprednisolone. Contrary to the solubilities above, methylprednisolone sodium succinate is soluble in water and alcohol, slightly soluble in acetone and insoluble in chloroformChemical properties
Methylprednisolone, or 6α-methylprednisolone, also known as 11β,17,21-trihydroxy-6α-methylpregna-1,4-diene-3,20-dione, is asynthetic Synthetic things are composed of multiple parts, often with the implication that they are artificial. In particular, 'synthetic' may refer to:
Science
* Synthetic chemical or compound, produced by the process of chemical synthesis
* Synthetic ...
pregnane steroid
A steroid is a biologically active organic compound with four rings arranged in a specific molecular configuration. Steroids have two principal biological functions: as important components of cell membranes that alter membrane fluidity; and ...
and a derivative
In mathematics, the derivative of a function of a real variable measures the sensitivity to change of the function value (output value) with respect to a change in its argument (input value). Derivatives are a fundamental tool of calculus. ...
of hydrocortisone (11β,17α,21-trihydroxypregn-4-ene-3,20-dione) and prednisolone
Prednisolone is a steroid medication used to treat certain types of allergies, inflammatory conditions, autoimmune disorders, and cancers. Some of these conditions include adrenocortical insufficiency, high blood calcium, rheumatoid arth ...
(11β,17α,21-trihydroxypregn-1,4-diene-3,20-dione). A variety of methylprednisolone esters with differing characteristics exist and have been marketed for medical use. They include methylprednisolone aceponate (Advantan), methylprednisolone acetate (Depo-Medrol), methylprednisolone succinate (Solu-Medrol), and methylprednisolone suleptanate (Medrosol, Promedrol).
Synthesis
Synthetic steroids are synthesized from cholic acid and sapogenins obtained from cattle and plants, respectively.History, society and culture
Methylprednisolone was first synthesized and manufactured by The Upjohn Company (now Pfizer) andFood and Drug Administration
The United States Food and Drug Administration (FDA or US FDA) is a federal agency of the Department of Health and Human Services. The FDA is responsible for protecting and promoting public health through the control and supervision of food ...
(FDA) approved in the United States on 2 October 1957. The patent has since expired, and generics are now available. In 2020, it was the 161st most commonly prescribed medication in the United States, with more than 3million prescriptions. Methylprednisolone has been a prescribed therapy amidst the COVID-19 pandemic
The COVID-19 pandemic, also known as the coronavirus pandemic, is an ongoing global pandemic of coronavirus disease 2019 (COVID-19) caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). The novel virus was first identi ...
, but there is no evidence it is either safe or effective for this purpose.
Research
Methylprednisolone has been a prescribed therapy amidst theCOVID-19 pandemic
The COVID-19 pandemic, also known as the coronavirus pandemic, is an ongoing global pandemic of coronavirus disease 2019 (COVID-19) caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). The novel virus was first identi ...
, but there is no evidence it is either safe or effective for this purpose.
References
External links
* * {{Portal bar, Medicine Alcohols Chemical substances for emergency medicine CYP3A4 inducers Glucocorticoids Ketones Pfizer brands Pregnanes Wikipedia medicine articles ready to translate World Health Organization essential medicines