Glycogen storage disease type I on:
[Wikipedia]
[Google]
[Amazon]
Glycogen storage disease type I (GSD I) is an
 The hypoglycemia of GSD I is termed "fasting", or "post-absorptive", usually about 4 hours after the complete digestion of a meal. This inability to maintain adequate blood glucose levels during fasting results from the combined impairment of both glycogenolysis and gluconeogenesis. Fasting hypoglycemia is often the most significant problem in GSD I, and typically the problem that leads to the diagnosis. Chronic hypoglycemia produces secondary metabolic adaptations, including chronically low
The hypoglycemia of GSD I is termed "fasting", or "post-absorptive", usually about 4 hours after the complete digestion of a meal. This inability to maintain adequate blood glucose levels during fasting results from the combined impairment of both glycogenolysis and gluconeogenesis. Fasting hypoglycemia is often the most significant problem in GSD I, and typically the problem that leads to the diagnosis. Chronic hypoglycemia produces secondary metabolic adaptations, including chronically low
 Impairment in the liver's ability to perform gluconeogenesis leads to clinically apparent
Impairment in the liver's ability to perform gluconeogenesis leads to clinically apparent
GeneReview/NIH/UW entry on Glycogen Storage Disease Type I
inherited disease
A genetic disorder is a health problem caused by one or more abnormalities in the genome. It can be caused by a mutation in a single gene (monogenic) or multiple genes (polygenic) or by a chromosomal abnormality. Although polygenic disorders ...
that results in the liver being unable to properly break down stored glycogen
Glycogen is a multibranched polysaccharide of glucose that serves as a form of energy storage in animals, fungi, and bacteria. The polysaccharide structure represents the main storage form of glucose in the body.
Glycogen functions as one of ...
. This impairment disrupts the liver
The liver is a major organ only found in vertebrates which performs many essential biological functions such as detoxification of the organism, and the synthesis of proteins and biochemicals necessary for digestion and growth. In humans, it i ...
's ability to break down stored glycogen
Glycogen is a multibranched polysaccharide of glucose that serves as a form of energy storage in animals, fungi, and bacteria. The polysaccharide structure represents the main storage form of glucose in the body.
Glycogen functions as one of ...
that is necessary to maintain adequate blood sugar level
Glycaemia, also known as blood sugar level, blood sugar concentration, or blood glucose level is the measure of glucose concentrated in the blood of humans or other animals. Approximately 4 grams of glucose, a simple sugar, is present in the bl ...
s. GSD I is divided into two main types, GSD Ia and GSD Ib, which differ in cause, presentation, and treatment. GSD Ia is caused by a deficiency in the enzyme
Enzymes () are proteins that act as biological catalysts by accelerating chemical reactions. The molecules upon which enzymes may act are called substrates, and the enzyme converts the substrates into different molecules known as products ...
glucose-6-phosphatase
The enzyme glucose 6-phosphatase (EC 3.1.3.9, G6Pase; systematic name D-glucose-6-phosphate phosphohydrolase) catalyzes the hydrolysis of glucose 6-phosphate, resulting in the creation of a phosphate group and free glucose:
: D-glucose 6-phos ...
, while GSD Ib is caused a deficiency in the enzyme glucose-6-phosphate translocase. Since glycogenolysis is the principal metabolic
Metabolism (, from el, μεταβολή ''metabolē'', "change") is the set of life-sustaining chemical reactions in organisms. The three main functions of metabolism are: the conversion of the energy in food to energy available to run cell ...
mechanism by which the liver supplies glucose
Glucose is a simple sugar with the molecular formula . Glucose is overall the most abundant monosaccharide, a subcategory of carbohydrates. Glucose is mainly made by plants and most algae during photosynthesis from water and carbon dioxide, u ...
to the body during periods of fasting
Fasting is the abstention from eating and sometimes drinking. From a purely physiological context, "fasting" may refer to the metabolic status of a person who has not eaten overnight (see " Breakfast"), or to the metabolic state achieved after ...
, both deficiencies cause severe low blood sugar
Hypoglycemia, also called low blood sugar, is a fall in blood sugar to levels below normal, typically below 70 mg/dL (3.9 mmol/L). Whipple's triad is used to properly identify hypoglycemic episodes. It is defined as blood glucose bel ...
and, over time, excess glycogen storage in the liver and (in some cases) the kidney
The kidneys are two reddish-brown bean-shaped organs found in vertebrates. They are located on the left and right in the retroperitoneal space, and in adult humans are about in length. They receive blood from the paired renal arteries; blo ...
s.
GSD I patients typically present with an enlarged liver
Hepatomegaly is the condition of having an enlarged liver. It is a non-specific medical sign having many causes, which can broadly be broken down into infection, hepatic tumours, or metabolic disorder. Often, hepatomegaly will present as an abdomi ...
from non-alcoholic fatty liver disease
Non-alcoholic fatty liver disease (NAFLD), also known as metabolic (dysfunction) associated fatty liver disease (MAFLD), is excessive fat build-up in the liver without another clear cause such as alcohol use. There are two types; non-alcoholic ...
as the result of this glycogen buildup. Other functions of the liver and kidneys are initially intact in GSD I, but are susceptible to a variety of other problems. Without proper treatment, GSD I gives rise to chronic low blood sugar, which can result in derangements including excessive levels of lactic acid and abnormally high levels of lipids in the bloodstream. Frequent feedings of cornstarch
Corn starch, maize starch, or cornflour (British English) is the starch derived from corn (maize) grain. The starch is obtained from the endosperm of the kernel. Corn starch is a common food ingredient, often used to thicken sauces or sou ...
or other carbohydrate
In organic chemistry, a carbohydrate () is a biomolecule consisting of carbon (C), hydrogen (H) and oxygen (O) atoms, usually with a hydrogen–oxygen atom ratio of 2:1 (as in water) and thus with the empirical formula (where ''m'' may o ...
s are the principal treatment for all forms of GSD I.
GSD Ib also features chronic neutropenia
Neutropenia is an abnormally low concentration of neutrophils (a type of white blood cell) in the blood. Neutrophils make up the majority of circulating white blood cells and serve as the primary defense against infections by destroying bacteri ...
due to a dysfunction in the production of neutrophil
Neutrophils (also known as neutrocytes or heterophils) are the most abundant type of granulocytes and make up 40% to 70% of all white blood cells in humans. They form an essential part of the innate immune system, with their functions varying ...
s in the bone marrow
Bone marrow is a semi-solid biological tissue, tissue found within the Spongy bone, spongy (also known as cancellous) portions of bones. In birds and mammals, bone marrow is the primary site of new blood cell production (or haematopoiesis). It i ...
. This immunodeficiency
Immunodeficiency, also known as immunocompromisation, is a state in which the immune system's ability to fight infectious diseases and cancer is compromised or entirely absent. Most cases are acquired ("secondary") due to extrinsic factors that a ...
, if untreated, makes GSD Ib patients susceptible to infection. The principal treatment for this feature of GSD Ib is filgrastim; however, patients often still require treatment for frequent infections, and a chronically enlarged spleen
Splenomegaly is an enlargement of the spleen. The spleen usually lies in the left upper quadrant (LUQ) of the human abdomen. Splenomegaly is one of the four cardinal signs of ''hypersplenism'' which include: some reduction in number of circulatin ...
is a common side effect. GSD Ib patients often present with inflammatory bowel disease
Inflammatory bowel disease (IBD) is a group of inflammatory conditions of the colon and small intestine, Crohn's disease and ulcerative colitis being the principal types. Crohn's disease affects the small intestine and large intestine, as well ...
.
It is the most common of the glycogen storage disease
A glycogen storage disease (GSD, also glycogenosis and dextrinosis) is a metabolic disorder caused by an enzyme Deficiency (medicine), deficiency affecting glycogen synthesis, glycogen breakdown, or glycolysis, glucose breakdown, typically in musc ...
s. GSD I has an incidence of approximately 1 in 100,000 births in the American population, and approximately 1 in 20,000 births among Ashkenazi Jews
Ashkenazi Jews ( ; he, יְהוּדֵי אַשְׁכְּנַז, translit=Yehudei Ashkenaz, ; yi, אַשכּנזישע ייִדן, Ashkenazishe Yidn), also known as Ashkenazic Jews or ''Ashkenazim'',, Ashkenazi Hebrew pronunciation: , singu ...
. The disease was named after German doctor Edgar von Gierke, who first described it in 1929.
Signs and symptoms
Early research into GSD I identified numerous clinical manifestations falsely thought to be primary features of the genetic disorder. However, continuing research has revealed that these clinical features are the consequences of only one (in GSD Ia) or two (in GSD Ib) fundamental abnormalities: * impairment in the liver's ability to convert stored glycogen into glucose throughglycogenolysis
Glycogenolysis is the breakdown of glycogen (n) to glucose-1-phosphate and glycogen (n-1). Glycogen branches are catabolized by the sequential removal of glucose monomers via phosphorolysis, by the enzyme glycogen phosphorylase.
Mechanism
T ...
* in GSD Ib, impairment of the neutrophil
Neutrophils (also known as neutrocytes or heterophils) are the most abundant type of granulocytes and make up 40% to 70% of all white blood cells in humans. They form an essential part of the innate immune system, with their functions varying ...
's ability to take up glucose, resulting in neutrophil dysfunction and neutropenia
Neutropenia is an abnormally low concentration of neutrophils (a type of white blood cell) in the blood. Neutrophils make up the majority of circulating white blood cells and serve as the primary defense against infections by destroying bacteri ...
These fundamental abnormalities give rise to a small number of primary clinical manifestations, which are the features considered in diagnosis of GSD I:
* Low blood sugar
Hypoglycemia, also called low blood sugar, is a fall in blood sugar to levels below normal, typically below 70 mg/dL (3.9 mmol/L). Whipple's triad is used to properly identify hypoglycemic episodes. It is defined as blood glucose bel ...
(hypoglycemia), due to impairment of glycogen breakdown (glycogenolysis) causing insufficient fasting blood glucose
Glycaemia, also known as blood sugar level, blood sugar concentration, or blood glucose level is the measure of glucose concentrated in the blood of humans or other animals. Approximately 4 grams of glucose, a simple sugar, is present in the b ...
* hepatomegaly
Hepatomegaly is the condition of having an enlarged liver. It is a non-specific medical sign having many causes, which can broadly be broken down into infection, hepatic tumours, or metabolic disorder. Often, hepatomegaly will present as an abdo ...
of non-alcoholic fatty liver disease
Non-alcoholic fatty liver disease (NAFLD), also known as metabolic (dysfunction) associated fatty liver disease (MAFLD), is excessive fat build-up in the liver without another clear cause such as alcohol use. There are two types; non-alcoholic ...
, due to impairment of glycogenolysis causing glycogen accumulation in the liver
* in GSD Ib, increased infection risk, due to neutropenia and neutrophil dysfunction
Affected people commonly present with secondary clinical manifestations, linked to one or more of the primary clinical manifestations:
* High levels of uric acid in the blood and attendant risk of gout or kidney damage, caused by low serum insulin levels in prolonged hypoglycemia
* High levels of lactic acid in the blood, in extreme cases leading to lactic acidosis
Lactic acidosis is a medical condition characterized by a build-up of lactate (especially -lactate) in the body, with formation of an excessively low pH in the bloodstream. It is a form of metabolic acidosis, in which excessive acid accumulates d ...
, caused by prolonged hypoglycemia
* hepatic adenomas developing in adulthood and attendant risk of anemia
Anemia or anaemia (British English) is a blood disorder in which the blood has a reduced ability to carry oxygen due to a lower than normal number of red blood cells, or a reduction in the amount of hemoglobin. When anemia comes on slowly, t ...
, suspected to be caused by blood glucose dysregulation in the presence of non-alcoholic fatty liver disease
Non-alcoholic fatty liver disease (NAFLD), also known as metabolic (dysfunction) associated fatty liver disease (MAFLD), is excessive fat build-up in the liver without another clear cause such as alcohol use. There are two types; non-alcoholic ...
* in GSD Ib, inflammatory bowel disease
Inflammatory bowel disease (IBD) is a group of inflammatory conditions of the colon and small intestine, Crohn's disease and ulcerative colitis being the principal types. Crohn's disease affects the small intestine and large intestine, as well ...
and attendant risk of anemia
Anemia or anaemia (British English) is a blood disorder in which the blood has a reduced ability to carry oxygen due to a lower than normal number of red blood cells, or a reduction in the amount of hemoglobin. When anemia comes on slowly, t ...
, caused by neutrophil dysfunction and exacerbated by the increased carbohydrate intake required to prevent hypoglycemia
In addition, there are several clinical manifestations that often result from the treatment of the primary clinical manifestations:
* pancreatic
The pancreas is an organ of the digestive system and endocrine system of vertebrates. In humans, it is located in the abdomen behind the stomach and functions as a gland. The pancreas is a mixed or heterocrine gland, i.e. it has both an endocr ...
hypertrophy
Hypertrophy is the increase in the volume of an organ or tissue due to the enlargement of its component cells. It is distinguished from hyperplasia, in which the cells remain approximately the same size but increase in number.Updated by Linda J. ...
, due to increased carbohydrate intake causing frequent engagement of the insulin response
* in GSD Ib, splenomegaly
Splenomegaly is an enlargement of the spleen. The spleen usually lies in the left upper quadrant (LUQ) of the human abdomen. Splenomegaly is one of the four cardinal signs of ''hypersplenism'' which include: some reduction in number of circulatin ...
, due to the long-term use of filgrastim to treat neutropenia causing sequestration of blood factors in the spleen
* in GSD Ib, an abnormally low number of platelets in the blood may occur, due to long-term use of filgrastim causing sequestration of platelets in the spleen
The spleen is an organ found in almost all vertebrates. Similar in structure to a large lymph node, it acts primarily as a blood filter. The word spleen comes .
* in GSD Ib, anemia
Anemia or anaemia (British English) is a blood disorder in which the blood has a reduced ability to carry oxygen due to a lower than normal number of red blood cells, or a reduction in the amount of hemoglobin. When anemia comes on slowly, t ...
, due to long-term use of filgrastim causing sequestration of hemoglobin
Hemoglobin (haemoglobin BrE) (from the Greek word αἷμα, ''haîma'' 'blood' + Latin ''globus'' 'ball, sphere' + ''-in'') (), abbreviated Hb or Hgb, is the iron-containing oxygen-transport metalloprotein present in red blood cells (erythroc ...
in the spleen, potentially exacerbated by uncontrolled inflammatory bowel disease
Inflammatory bowel disease (IBD) is a group of inflammatory conditions of the colon and small intestine, Crohn's disease and ulcerative colitis being the principal types. Crohn's disease affects the small intestine and large intestine, as well ...
Hypoglycemia
Low blood sugar
Hypoglycemia, also called low blood sugar, is a fall in blood sugar to levels below normal, typically below 70 mg/dL (3.9 mmol/L). Whipple's triad is used to properly identify hypoglycemic episodes. It is defined as blood glucose bel ...
(hypoglycemia) is the primary clinical symptom
Signs and symptoms are the observed or detectable signs, and experienced symptoms of an illness, injury, or condition. A sign for example may be a higher or lower temperature than normal, raised or lowered blood pressure or an abnormality showi ...
common to both GSD Ia and GSD Ib and most often prompts initial diagnosis of the disease. During fetal
A fetus or foetus (; plural fetuses, feti, foetuses, or foeti) is the unborn offspring that develops from an animal embryo. Following embryonic development the fetal stage of development takes place. In human prenatal development, fetal develo ...
development in utero, maternal glucose transferred across the placenta
The placenta is a temporary embryonic and later fetal organ that begins developing from the blastocyst shortly after implantation. It plays critical roles in facilitating nutrient, gas and waste exchange between the physically separate mate ...
prevents hypoglycemia
Hypoglycemia, also called low blood sugar, is a fall in blood sugar to levels below normal, typically below 70 mg/dL (3.9 mmol/L). Whipple's triad is used to properly identify hypoglycemic episodes. It is defined as blood glucose bel ...
. However, after birth, the inability to maintain blood glucose from stored glycogen in the liver causes measurable hypoglycemia in no more than 1–2 hours after feedings. Without proper dietary treatment after birth, prolonged hypoglycemia often leads to sudden lactic acidosis
Lactic acidosis is a medical condition characterized by a build-up of lactate (especially -lactate) in the body, with formation of an excessively low pH in the bloodstream. It is a form of metabolic acidosis, in which excessive acid accumulates d ...
that can induce primary respiratory distress in the newborn period, as well as ketoacidosis
Ketoacidosis is a metabolic state caused by uncontrolled production of ketone bodies that cause a metabolic acidosis. While ketosis refers to any elevation of blood ketones, ketoacidosis is a specific pathologic condition that results in changes ...
.
Neurological
Neurology (from el, νεῦρον (neûron), "string, nerve" and the suffix -logia, "study of") is the branch of medicine dealing with the diagnosis and treatment of all categories of conditions and disease involving the brain, the spinal c ...
manifestations of hypoglycemia are less severe in GSD I than in other instances. Rather than acute hypoglycemia, GSD I patients experience persistent mild hypoglycemia. The diminished likelihood of neurological manifestations is due to the habituation of the brain to mild hypoglycemia. Given the reduced blood glucose level, the brain adapts to using alternative fuels like lactate
Lactate may refer to:
* Lactation, the secretion of milk from the mammary glands
* Lactate, the conjugate base of lactic acid
Lactic acid is an organic acid. It has a molecular formula . It is white in the solid state and it is miscible with w ...
. These gradual metabolic adaptations during infancy make severe symptoms like unconsciousness
Unconsciousness is a state in which a living individual exhibits a complete, or near-complete, inability to maintain an awareness of self and environment or to respond to any human or environmental stimulus. Unconsciousness may occur as the r ...
or seizure
An epileptic seizure, informally known as a seizure, is a period of symptoms due to abnormally excessive or synchronous neuronal activity in the brain. Outward effects vary from uncontrolled shaking movements involving much of the body with lo ...
uncommon before diagnosis.
In the early weeks of life, undiagnosed infants with GSD I tolerate persistent hypoglycemia and compensated lactic acidosis between feedings without symptoms. Without consistent carbohydrate feeding, infant blood glucose levels typically measure between 25 and 50 mg/dL (1.4 to 2.8 mmol/L). After weeks to months without treatment with consistent oral carbohydrates, infants will progress to show clear symptoms of hypoglycemia and lactic acidosis. Infants may present with paleness, clamminess, irritability, respiratory distress, and an inability to sleep through the night even in the second year of life. Developmental delay
Global developmental delay is an umbrella term used when children are significantly delayed in their cognitive and physical development. It can be diagnosed when a child is delayed in one or more milestones, categorised into motor skills, speech ...
is not an intrinsic effect of GSD I, but is common if the diagnosis is not made in early infancy.
Genetics
GSD I is inherited in anautosomal recessive
In genetics, dominance is the phenomenon of one variant ( allele) of a gene on a chromosome masking or overriding the effect of a different variant of the same gene on the other copy of the chromosome. The first variant is termed dominant an ...
manner. People with one copy of the faulty gene are carrier
Carrier may refer to:
Entertainment
* ''Carrier'' (album), a 2013 album by The Dodos
* ''Carrier'' (board game), a South Pacific World War II board game
* ''Carrier'' (TV series), a ten-part documentary miniseries that aired on PBS in April 20 ...
s of the disease and have no symptoms. As with other autosomal recessive diseases, each child born to two carriers of the disease has a 25% chance of inheriting both copies of the faulty gene and manifesting the disease. Unaffected parents of a child with GSD I can be assumed to be carriers. Prenatal diagnosis has been made by fetal liver biopsy
Liver biopsy is the biopsy (removal of a small sample of tissue) from the liver. It is a medical test that is done to aid diagnosis of liver disease, to assess the severity of known liver disease, and to monitor the progress of treatment.
Medica ...
at 18–22 weeks of gestation, but no fetal treatment has been proposed. Prenatal diagnosis is possible with fetal DNA obtained by chorionic villus sampling
Chorionic villus sampling (CVS), sometimes called "chorionic ''villous'' sampling" (as "villous" is the adjectival form of the word "villus"), is a form of prenatal diagnosis done to determine chromosomal or genetic disorders in the fetus. It ent ...
when a fetus is known to be at risk.
The most common forms of GSD I are designated GSD Ia and GSD Ib, the former accounting for over 80% of diagnosed cases and the latter for less than 20%. A few rarer forms have been described.
* GSD Ia results from mutations of ''G6PC'', the gene
In biology, the word gene (from , ; "...Wilhelm Johannsen coined the word gene to describe the Mendelian units of heredity..." meaning ''generation'' or ''birth'' or ''gender'') can have several different meanings. The Mendelian gene is a b ...
for glucose-6-phosphatase, located on chromosome 17
Chromosome 17 is one of the 23 pairs of chromosomes in humans. People normally have two copies of this chromosome. Chromosome 17 spans more than 83 million base pairs (the building material of DNA) and represents between 2.5 and 3% of the total D ...
q21.
* GSD Ib results from mutations of the gene for SLC37A4
Glucose-6-phosphate exchanger SLC37A4, also known as glucose-6-phosphate translocase, is an enzyme that in humans is encoded by the ''SLC37A4'' gene
In biology, the word gene (from , ; "...Wilhelm Johannsen coined the word gene to describe t ...
or "G6PT1", the glucose-6-phosphate transporter.
* GSD Ic results from mutations of SLC17A3 or SLC37A4
Glucose-6-phosphate exchanger SLC37A4, also known as glucose-6-phosphate translocase, is an enzyme that in humans is encoded by the ''SLC37A4'' gene
In biology, the word gene (from , ; "...Wilhelm Johannsen coined the word gene to describe t ...
.
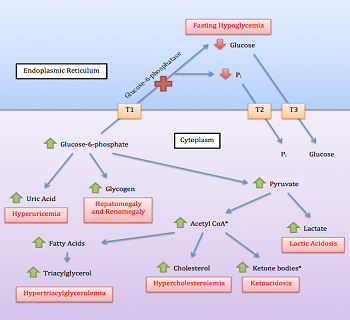
Glucose-6-phosphatase is an enzyme located on the inner membrane
A membrane is a selective barrier; it allows some things to pass through but stops others. Such things may be molecules, ions, or other small particles. Membranes can be generally classified into synthetic membranes and biological membranes. ...
of the endoplasmic reticulum
The endoplasmic reticulum (ER) is, in essence, the transportation system of the eukaryotic cell, and has many other important functions such as protein folding. It is a type of organelle made up of two subunits – rough endoplasmic reticulum ...
. The catalytic unit is associated with a calcium
Calcium is a chemical element with the symbol Ca and atomic number 20. As an alkaline earth metal, calcium is a reactive metal that forms a dark oxide-nitride layer when exposed to air. Its physical and chemical properties are most similar ...
binding protein
Proteins are large biomolecules and macromolecules that comprise one or more long chains of amino acid residues. Proteins perform a vast array of functions within organisms, including catalysing metabolic reactions, DNA replication, res ...
, and three transport proteins (T1, T2, T3) that facilitate movement of glucose-6-phosphate (G6P), phosphate
In chemistry, a phosphate is an anion, salt, functional group or ester derived from a phosphoric acid. It most commonly means orthophosphate, a derivative of orthophosphoric acid .
The phosphate or orthophosphate ion is derived from phosph ...
, and glucose
Glucose is a simple sugar with the molecular formula . Glucose is overall the most abundant monosaccharide, a subcategory of carbohydrates. Glucose is mainly made by plants and most algae during photosynthesis from water and carbon dioxide, u ...
(respectively) into and out of the enzyme.
Pathophysiology
Normal carbohydrate balance and maintenance of blood glucose levels
Glycogen in liver and (to a lesser degree) kidneys serves as a form of stored, rapidly accessible glucose, so that the blood glucose level can be maintained between meals. For about 3 hours after a carbohydrate-containing meal, high insulin levels direct liver cells to take glucose from the blood, to convert it to glucose-6-phosphate (G6P) with the enzyme glucokinase, and to add the G6P molecules to the ends of chains of glycogen (glycogen synthesis). Excess G6P is also shunted into production oftriglyceride
A triglyceride (TG, triacylglycerol, TAG, or triacylglyceride) is an ester derived from glycerol and three fatty acids (from ''tri-'' and ''glyceride'').
Triglycerides are the main constituents of body fat in humans and other vertebrates, as ...
s and exported for storage in adipose tissue
Adipose tissue, body fat, or simply fat is a loose connective tissue composed mostly of adipocytes. In addition to adipocytes, adipose tissue contains the stromal vascular fraction (SVF) of cells including preadipocytes, fibroblasts, vascular ...
as fat.
When digestion
Digestion is the breakdown of large insoluble food molecules into small water-soluble food molecules so that they can be absorbed into the watery blood plasma. In certain organisms, these smaller substances are absorbed through the small intest ...
of a meal is complete, insulin levels fall, and enzyme systems in the liver cells begin to remove glucose molecules from strands of glycogen in the form of G6P. This process is termed glycogenolysis
Glycogenolysis is the breakdown of glycogen (n) to glucose-1-phosphate and glycogen (n-1). Glycogen branches are catabolized by the sequential removal of glucose monomers via phosphorolysis, by the enzyme glycogen phosphorylase.
Mechanism
T ...
. The G6P remains within the liver cell unless the phosphate is cleaved by glucose-6-phosphatase. This dephosphorylation
In biochemistry, dephosphorylation is the removal of a phosphate (PO43−) group from an organic compound by hydrolysis. It is a reversible post-translational modification. Dephosphorylation and its counterpart, phosphorylation, activate and de ...
reaction produces free glucose and free anion
An ion () is an atom or molecule with a net electrical charge.
The charge of an electron is considered to be negative by convention and this charge is equal and opposite to the charge of a proton, which is considered to be positive by conve ...
s. The free glucose molecules can be transported out of the liver cells into the blood to maintain an adequate supply of glucose to the brain
A brain is an organ (biology), organ that serves as the center of the nervous system in all vertebrate and most invertebrate animals. It is located in the head, usually close to the sensory organs for senses such as Visual perception, vision. I ...
and other organs of the body. Glycogenolysis can supply the glucose needs of an adult body for 12–18 hours.
When fasting continues for more than a few hours, falling insulin levels permit catabolism
Catabolism () is the set of metabolic pathways that breaks down molecules into smaller units that are either oxidized to release energy or used in other anabolic reactions. Catabolism breaks down large molecules (such as polysaccharides, li ...
of muscle
Skeletal muscles (commonly referred to as muscles) are organs of the vertebrate muscular system and typically are attached by tendons to bones of a skeleton. The muscle cells of skeletal muscles are much longer than in the other types of mus ...
protein and triglycerides from adipose tissue. The products of these processes are amino acid
Amino acids are organic compounds that contain both amino and carboxylic acid functional groups. Although hundreds of amino acids exist in nature, by far the most important are the alpha-amino acids, which comprise proteins. Only 22 alpha ...
s (mainly alanine
Alanine (symbol Ala or A), or α-alanine, is an α-amino acid that is used in the biosynthesis of proteins. It contains an amine group and a carboxylic acid group, both attached to the central carbon atom which also carries a methyl group side ...
), free fatty acid
In chemistry, particularly in biochemistry, a fatty acid is a carboxylic acid with an aliphatic chain, which is either saturated or unsaturated. Most naturally occurring fatty acids have an unbranched chain of an even number of carbon atoms, fr ...
s, and lactic acid
Lactic acid is an organic acid. It has a molecular formula . It is white in the solid state and it is miscible with water. When in the dissolved state, it forms a colorless solution. Production includes both artificial synthesis as well as nat ...
. Free fatty acids from triglycerides are converted to ketone
In organic chemistry, a ketone is a functional group with the structure R–C(=O)–R', where R and R' can be a variety of carbon-containing substituents. Ketones contain a carbonyl group –C(=O)– (which contains a carbon-oxygen double b ...
s, and to acetyl-CoA
Acetyl-CoA (acetyl coenzyme A) is a molecule that participates in many biochemical reactions in protein, carbohydrate and lipid metabolism. Its main function is to deliver the acetyl group to the citric acid cycle (Krebs cycle) to be oxidized for ...
. Amino acids and lactic acid are used to synthesize new G6P in liver cells by the process of gluconeogenesis
Gluconeogenesis (GNG) is a metabolic pathway that results in the generation of glucose from certain non- carbohydrate carbon substrates. It is a ubiquitous process, present in plants, animals, fungi, bacteria, and other microorganisms. In verteb ...
. The last step of normal gluconeogenesis, like the last step of glycogenolysis, is the dephosphorylation of G6P by glucose-6-phosphatase to free glucose and .
Thus glucose-6-phosphatase mediates the final, key, step in both of the two main processes of glucose production during fasting. The effect is amplified because the resulting high levels of glucose-6-phosphate inhibit earlier key steps in both glycogenolysis and gluconeogenesis.
Pathophysiology
The principal metabolic effects of deficiency of glucose-6-phosphatase arehypoglycemia
Hypoglycemia, also called low blood sugar, is a fall in blood sugar to levels below normal, typically below 70 mg/dL (3.9 mmol/L). Whipple's triad is used to properly identify hypoglycemic episodes. It is defined as blood glucose bel ...
, lactic acidosis
Lactic acidosis is a medical condition characterized by a build-up of lactate (especially -lactate) in the body, with formation of an excessively low pH in the bloodstream. It is a form of metabolic acidosis, in which excessive acid accumulates d ...
, hypertriglyceridemia
Hypertriglyceridemia is the presence of high amounts of triglycerides in the blood. Triglycerides are the most abundant fatty molecule in most organisms. Hypertriglyceridemia occurs in various physiologic conditions and in various diseases, and ...
, and hyperuricemia
Hyperuricaemia or hyperuricemia is an abnormally high level of uric acid in the blood. In the pH conditions of body fluid, uric acid exists largely as urate, the ion form. Serum uric acid concentrations greater than 6 mg/dL for females, 7&nbs ...
.
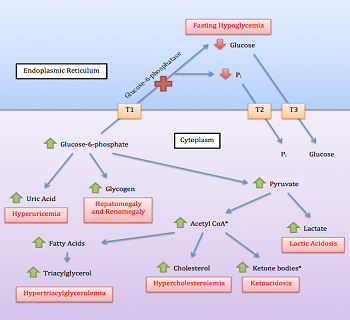 The hypoglycemia of GSD I is termed "fasting", or "post-absorptive", usually about 4 hours after the complete digestion of a meal. This inability to maintain adequate blood glucose levels during fasting results from the combined impairment of both glycogenolysis and gluconeogenesis. Fasting hypoglycemia is often the most significant problem in GSD I, and typically the problem that leads to the diagnosis. Chronic hypoglycemia produces secondary metabolic adaptations, including chronically low
The hypoglycemia of GSD I is termed "fasting", or "post-absorptive", usually about 4 hours after the complete digestion of a meal. This inability to maintain adequate blood glucose levels during fasting results from the combined impairment of both glycogenolysis and gluconeogenesis. Fasting hypoglycemia is often the most significant problem in GSD I, and typically the problem that leads to the diagnosis. Chronic hypoglycemia produces secondary metabolic adaptations, including chronically low insulin
Insulin (, from Latin ''insula'', 'island') is a peptide hormone produced by beta cells of the pancreatic islets encoded in humans by the ''INS'' gene. It is considered to be the main anabolic hormone of the body. It regulates the metabolism ...
levels and high levels of glucagon
Glucagon is a peptide hormone, produced by alpha cells of the pancreas. It raises concentration of glucose and fatty acids in the bloodstream, and is considered to be the main catabolic hormone of the body. It is also used as a medication to tre ...
and cortisol
Cortisol is a steroid hormone, in the glucocorticoid class of hormones. When used as a medication, it is known as hydrocortisone.
It is produced in many animals, mainly by the '' zona fasciculata'' of the adrenal cortex in the adrenal g ...
.
Lactic acidosis arises from impairment of gluconeogenesis. Lactic acid is generated both in the liver and muscle and is oxidized by NAD+ to pyruvic acid
Pyruvic acid (CH3COCOOH) is the simplest of the alpha-keto acids, with a carboxylic acid and a ketone functional group. Pyruvate, the conjugate base, CH3COCOO−, is an intermediate in several metabolic pathways throughout the cell.
Pyruvic aci ...
and then converted via the gluconeogenic pathway to G6P. Accumulation of G6P inhibits conversion of lactate to pyruvate. The lactic acid level rises during fasting as glucose falls. In people with GSD I, it may not fall entirely to normal even when normal glucose levels are restored.
Hypertriglyceridemia resulting from amplified triglyceride production is another indirect effect of impaired gluconeogenesis, amplified by chronically low insulin levels. During fasting, the normal conversion of triglycerides to free fatty acids, ketones, and ultimately acetyl-CoA is impaired. Triglyceride levels in GSD I can reach several times normal and serve as a clinical index of "metabolic control".
Hyperuricemia results from a combination of increased generation and decreased excretion of uric acid
Uric acid is a heterocyclic compound of carbon, nitrogen, oxygen, and hydrogen with the formula C5H4N4O3. It forms ions and salts known as urates and acid urates, such as ammonium acid urate. Uric acid is a product of the metabolic breakdown ...
, which is generated when increased amounts of G6P are metabolized via the pentose phosphate pathway. It is also a byproduct of purine
Purine is a heterocyclic aromatic organic compound that consists of two rings ( pyrimidine and imidazole) fused together. It is water-soluble. Purine also gives its name to the wider class of molecules, purines, which include substituted purines ...
degradation. Uric acid competes with lactic acid and other organic acids for renal excretion in the urine. In GSD I increased availability of G6P for the pentose phosphate pathway, increased rates of catabolism, and diminished urinary excretion due to high levels of lactic acid all combine to produce uric acid levels several times normal. Although hyperuricemia is asymptomatic for years, kidney and joint damage gradually accrue.
Elevated lactate and lactic acidosis
High levels of lactic acid in the blood are observed in all people with GSD I, due to impairedgluconeogenesis
Gluconeogenesis (GNG) is a metabolic pathway that results in the generation of glucose from certain non- carbohydrate carbon substrates. It is a ubiquitous process, present in plants, animals, fungi, bacteria, and other microorganisms. In verteb ...
. Baseline elevations generally range from 4 to 10 mol/mL, which will not cause any clinical impact. However, during and after an episode of low blood sugar, lactate levels will abruptly rise to exceed 15 mol/mL, the threshold for lactic acidosis
Lactic acidosis is a medical condition characterized by a build-up of lactate (especially -lactate) in the body, with formation of an excessively low pH in the bloodstream. It is a form of metabolic acidosis, in which excessive acid accumulates d ...
. Symptoms of lactic acidosis include vomiting and hyperpnea, both of which can exacerbate hypoglycemia in the setting of GSD I. In cases of acute lactic acidosis, patients need emergency care to stabilize blood oxygen, and restore blood glucose. Proper identification of lactic acidosis in undiagnosed children presents a challenge, since the first symptoms are typically vomiting and dehydration, both of which mimic childhood infections like gastroenteritis
Gastroenteritis, also known as infectious diarrhea and gastro, is an inflammation of the gastrointestinal tract including the stomach and intestine. Symptoms may include diarrhea, vomiting, and abdominal pain. Fever, lack of energy, and dehydr ...
or pneumonia
Pneumonia is an inflammatory condition of the lung primarily affecting the small air sacs known as alveoli. Symptoms typically include some combination of productive or dry cough, chest pain, fever, and difficulty breathing. The severit ...
. Moreover, both of these common infections can precipitate more severe hypoglycemia in undiagnosed children, making diagnosis of the underlying cause difficult.
As elevated lactate persists, uric acid, ketoacids, and free fatty acid
In chemistry, particularly in biochemistry, a fatty acid is a carboxylic acid with an aliphatic chain, which is either saturated or unsaturated. Most naturally occurring fatty acids have an unbranched chain of an even number of carbon atoms, fr ...
s further increase the anion gap
The anion gap (AG or AGAP) is a value calculated from the results of multiple individual medical lab tests. It may be reported with the results of an electrolyte panel, which is often performed as part of a comprehensive metabolic panel.
The an ...
. In adults and children, the high concentrations of lactate cause significant discomfort in the muscles. This discomfort is an amplified form of the burning sensation a runner may feel in the quadriceps
The quadriceps femoris muscle (, also called the quadriceps extensor, quadriceps or quads) is a large muscle group that includes the four prevailing muscles on the front of the thigh. It is the sole extensor muscle of the knee, forming a large ...
after sprinting, which is caused by a brief buildup of lactic acid. Proper control of hypoglycemia in GSD I eliminates the possibility for lactic acidosis.
Elevated urate and complications
High levels ofuric acid
Uric acid is a heterocyclic compound of carbon, nitrogen, oxygen, and hydrogen with the formula C5H4N4O3. It forms ions and salts known as urates and acid urates, such as ammonium acid urate. Uric acid is a product of the metabolic breakdown ...
often present as a consequence of elevated lactic acid in GSD I patients. When lactate levels are elevated, blood-borne lactic acid competes for the same kidney tubular transport mechanism as urate, limiting the rate that urate can be cleared by the kidneys into the urine. If present, increased purine
Purine is a heterocyclic aromatic organic compound that consists of two rings ( pyrimidine and imidazole) fused together. It is water-soluble. Purine also gives its name to the wider class of molecules, purines, which include substituted purines ...
catabolism is an additional contributing factor. Uric acid levels of 6 to 12 mg/dl (530 to 1060 umol/L) are common among GSD I patients, if the disease is not properly treated. In some affected people, the use of the medication allopurinol
Allopurinol is a medication used to decrease high blood uric acid levels. It is specifically used to prevent gout, prevent specific types of kidney stones and for the high uric acid levels that can occur with chemotherapy. It is taken by mouth ...
is necessary to lower blood urate levels. Consequences of hyperuricemia among GSD I patients include the development of kidney stones
Kidney stone disease, also known as nephrolithiasis or urolithiasis, is a crystallopathy where a calculus (medicine), solid piece of material (kidney stone) develops in the urinary tract. Kidney stones typically form in the kidney and leave the ...
and the accumulation of uric acid crystals in joints, leading to kidney disease
Kidney disease, or renal disease, technically referred to as nephropathy, is damage to or disease of a kidney. Nephritis is an inflammatory kidney disease and has several types according to the location of the inflammation. Inflammation can ...
and gout
Gout ( ) is a form of inflammatory arthritis characterized by recurrent attacks of a red, tender, hot and swollen joint, caused by deposition of monosodium urate monohydrate crystals. Pain typically comes on rapidly, reaching maximal intens ...
, respectively.
Hyperlipidemia and plasma effects
Elevated triglycerides in GSD I result from low seruminsulin
Insulin (, from Latin ''insula'', 'island') is a peptide hormone produced by beta cells of the pancreatic islets encoded in humans by the ''INS'' gene. It is considered to be the main anabolic hormone of the body. It regulates the metabolism ...
in patients with frequent prolonged hypoglycemia. It may also be caused by intracellular accumulation of glucose-6-phosphate with secondary shunting to pyruvate
Pyruvic acid (CH3COCOOH) is the simplest of the alpha-keto acids, with a carboxylic acid and a ketone functional group. Pyruvate, the conjugate base, CH3COCOO−, is an intermediate in several metabolic pathways throughout the cell.
Pyruvic a ...
, which is converted into Acetyl-CoA
Acetyl-CoA (acetyl coenzyme A) is a molecule that participates in many biochemical reactions in protein, carbohydrate and lipid metabolism. Its main function is to deliver the acetyl group to the citric acid cycle (Krebs cycle) to be oxidized for ...
, which is transported to the cytosol
The cytosol, also known as cytoplasmic matrix or groundplasm, is one of the liquids found inside cells ( intracellular fluid (ICF)). It is separated into compartments by membranes. For example, the mitochondrial matrix separates the mitochondri ...
where the synthesis of fatty acid
In chemistry, particularly in biochemistry, a fatty acid is a carboxylic acid with an aliphatic chain, which is either saturated or unsaturated. Most naturally occurring fatty acids have an unbranched chain of an even number of carbon atoms, f ...
s and cholesterol
Cholesterol is any of a class of certain organic molecules called lipids. It is a sterol (or modified steroid), a type of lipid. Cholesterol is biosynthesized by all animal cells and is an essential structural component of animal cell memb ...
occurs. Triglycerides above the 3.4 mmol/L (300 mg/dL) range may produce visible lipemia, and even a mild pseudohyponatremia due to a reduced aqueous fraction of the blood plasma
Blood plasma is a light amber-colored liquid component of blood in which blood cells are absent, but contains proteins and other constituents of whole blood in suspension. It makes up about 55% of the body's total blood volume. It is the int ...
. In GSD I, cholesterol
Cholesterol is any of a class of certain organic molecules called lipids. It is a sterol (or modified steroid), a type of lipid. Cholesterol is biosynthesized by all animal cells and is an essential structural component of animal cell memb ...
is typically only mildly elevated compared to other lipid
Lipids are a broad group of naturally-occurring molecules which includes fats, waxes, sterols, fat-soluble vitamins (such as vitamins A, D, E and K), monoglycerides, diglycerides, phospholipids, and others. The functions of lipids in ...
s.
Hepatomegaly
 Impairment in the liver's ability to perform gluconeogenesis leads to clinically apparent
Impairment in the liver's ability to perform gluconeogenesis leads to clinically apparent hepatomegaly
Hepatomegaly is the condition of having an enlarged liver. It is a non-specific medical sign having many causes, which can broadly be broken down into infection, hepatic tumours, or metabolic disorder. Often, hepatomegaly will present as an abdo ...
. Without this process, the body is unable to liberate glycogen from the liver and convert it into blood glucose, leading to an accumulation of stored glycogen in the liver. Hepatomegaly from the accumulation of stored glycogen in the liver is considered a form of non-alcoholic fatty liver disease
Non-alcoholic fatty liver disease (NAFLD), also known as metabolic (dysfunction) associated fatty liver disease (MAFLD), is excessive fat build-up in the liver without another clear cause such as alcohol use. There are two types; non-alcoholic ...
. GSD I patients present with a degree of hepatomegaly
Hepatomegaly is the condition of having an enlarged liver. It is a non-specific medical sign having many causes, which can broadly be broken down into infection, hepatic tumours, or metabolic disorder. Often, hepatomegaly will present as an abdo ...
throughout life, but severity often relates to the consumption of excess dietary carbohydrate
In organic chemistry, a carbohydrate () is a biomolecule consisting of carbon (C), hydrogen (H) and oxygen (O) atoms, usually with a hydrogen–oxygen atom ratio of 2:1 (as in water) and thus with the empirical formula (where ''m'' may o ...
. Reductions in the mass of the liver are possible, since most patients retain residual hepatic function that allows for the liberation of stored glycogen
Glycogen is a multibranched polysaccharide of glucose that serves as a form of energy storage in animals, fungi, and bacteria. The polysaccharide structure represents the main storage form of glucose in the body.
Glycogen functions as one of ...
at a limited rate.
GSD I patients often present with hepatomegaly from the time of birth. In fetal development, maternal glucose transferred to the fetus prevents hypoglycemia, but the storage of glucose as glycogen in the liver leads to hepatomegaly. There is no evidence that this hepatomegaly presents any risk to proper fetal development.
Hepatomegaly in GSD type I generally occurs without sympathetic enlargement of the spleen. GSD Ib patients may present with splenomegaly, but this is connected to the use of filgrastim to treat neutropenia in this subtype, not comorbid hepatomegaly. Hepatomegaly will persist to some degree throughout life, often causing the abdomen to protrude, and in severe cases may be palpable at or below the navel
The navel (clinically known as the umbilicus, commonly known as the belly button or tummy button) is a protruding, flat, or hollowed area on the abdomen at the attachment site of the umbilical cord. All placental mammals have a navel, altho ...
. In GSD-related non-alcoholic fatty liver disease, hepatic function is usually spared, with liver enzymes and bilirubin
Bilirubin (BR) ( Latin for "red bile") is a red-orange compound that occurs in the normal catabolic pathway that breaks down heme in vertebrates. This catabolism is a necessary process in the body's clearance of waste products that arise from t ...
remaining within the normal range. However, liver function may be affected by other hepatic complications in adulthood, including the development of hepatic adenomas.
Hepatic adenomas
The specificetiology
Etiology (pronounced ; alternatively: aetiology or ætiology) is the study of causation or origination. The word is derived from the Greek (''aitiología'') "giving a reason for" (, ''aitía'', "cause"); and ('' -logía''). More completely, ...
of hepatic adenomas in GSD I remains unknown, despite ongoing research. The typical GSD I patient presenting with at least one adenoma
An adenoma is a benign tumor of epithelial tissue with glandular origin, glandular characteristics, or both. Adenomas can grow from many glandular organs, including the adrenal glands, pituitary gland, thyroid, prostate, and others. Some adenom ...
is an adult, though lesion
A lesion is any damage or abnormal change in the tissue of an organism, usually caused by disease or trauma. ''Lesion'' is derived from the Latin "injury". Lesions may occur in plants as well as animals.
Types
There is no designated classif ...
s have been observed in patients as young as fourteen. Adenomas, composed of heterogeneous neoplasms, may occur individually or in multiples. Estimates on the rate of conversion of a hepatocellular adenoma into hepatocellular carcinoma
Hepatocellular carcinoma (HCC) is the most common type of primary liver cancer in adults and is currently the most common cause of death in people with cirrhosis. HCC is the third leading cause of cancer-related deaths worldwide.
It occurs in t ...
in GSD I range from 0% to 11%, with the latter figure representing more recent research. One reason for the increasing estimate is the growing population of GSD I patients surviving into adulthood, when most adenomas develop.
Treatment standards dictate regular observation of the liver by MRI or CT scan to monitor for structural abnormalities. Hepatic adenomas may be misidentified as focal nodular hyperplasia
Focal nodular hyperplasia (FNH) is a benign tumor of the liver
The liver is a major organ only found in vertebrates which performs many essential biological functions such as detoxification of the organism, and the synthesis of proteins and ...
in diagnostic imaging, though this condition is rare. However, hepatic adenomas in GSD I uniquely involve diffuse Mallory hyaline deposition, which is otherwise commonly observed in focal nodular hyperplasia. Unlike common hepatic adenomas related to oral contraception, hemorrhaging in GSD I patients is rare.
While the reason for the high prevalence of adenomas in GSD I is unclear, research since the 1970s has implicated serum glucagon
Glucagon is a peptide hormone, produced by alpha cells of the pancreas. It raises concentration of glucose and fatty acids in the bloodstream, and is considered to be the main catabolic hormone of the body. It is also used as a medication to tre ...
as a potential driver. In studies, patients that have been put on a dietary regimen to keep blood sugar in a normal range spanning 72 to 108 mg/dL (4.0 to 6.0 mmol/L) have shown a decreased likelihood of developing adenomas. Moreover, patients with well controlled blood glucose have consistently seen a reduction in the size and number of hepatic adenomas, suggesting that adenomas may be caused by imbalances of hepatotropic agents like serum insulin and especially serum glucagon in the liver.
Osteopenia
Patients with GSD I will often develop osteopenia. The specific etiology of low bone mineral density in GSD is not known, though it is strongly associated with poor metabolic control. Osteopenia may be directly caused by hypoglycemia, or the resulting endocrine and metabolic sequelae. Improvements in metabolic control have consistently been shown to prevent or reverse clinically relevant osteopenia in GSD I patients. In cases where osteopenia progresses with age, bone mineral density in the ribs is typically more severe than in the vertebrae. In some cases bone mineral density T-score will drop below -2.5, indicating osteoporosis. There is some evidence that osteopenia may be connected with associated kidney abnormalities in GSD I, particularly glomular hyperfiltration. The condition also seems responsive to calcium supplementation. In many cases bone mineral density can increase and return to the normal range given proper metabolic control and calcium supplementation alone, reversing osteopenia.Kidney effects
The kidneys are usually 10 to 20% enlarged with stored glycogen. In adults with GSD I, chronic glomerular damage similar todiabetic nephropathy
Diabetic nephropathy, also known as diabetic kidney disease, is the chronic loss of kidney function occurring in those with diabetes mellitus. Diabetic nephropathy is the leading causes of chronic kidney disease (CKD) and end-stage renal disease ...
may lead to kidney failure
Kidney failure, also known as end-stage kidney disease, is a medical condition in which the kidneys can no longer adequately filter waste products from the blood, functioning at less than 15% of normal levels. Kidney failure is classified as eit ...
. GSD I may present with various kidney complications. Renal tubular abnormalities related to hyperlactatemia are seen early in life, likely because prolonged lactic acidosis is more likely to occur in childhood. This will often present as Fanconi syndrome with multiple derangements of renal tubular reabsorption, including tubular acidosis with bicarbonate and phosphate wasting. These tubular abnormalities in GSD I are typically detected and monitored by urinary calcium. Long term these derangements can exacerbate uric acid nephropathy, otherwise driven by hyperlactatemia. In adolescence and beyond, glomerular disease may independently develop, initially presenting as glomerular hyperfiltration Glomerular hyperfiltration is a situation where the filtration elements in the kidneys called glomeruli produce excessive amounts of pro-urine. It can be part of a number of medical conditions particularly diabetic nephropathy (kidney damage associa ...
indicated by elevated urinary eGFR.
Splenomegaly
Enlargement of the spleen (splenomegaly) is common in GSD I and has two primary causes. In GSD Ia, splenomegaly may be caused by a relation between the liver and the spleen which causes either to grow or shrink to match the relative size of the other, to a lessened degree. In GSD Ib, it is a side effect of the use of filgrastim to treat neutropenia.Bowel effects
Intestinal involvement can cause mildmalabsorption
Malabsorption is a state arising from abnormality in absorption of food nutrients across the gastrointestinal (GI) tract. Impairment can be of single or multiple nutrients depending on the abnormality. This may lead to malnutrition and a variety ...
with greasy stools (steatorrhea
Steatorrhea (or steatorrhoea) is the presence of excess fat in feces. Stools may be bulky and difficult to flush, have a pale and oily appearance, and can be especially foul-smelling. An oily anal leakage or some level of fecal incontinence may o ...
), but usually requires no treatment.
Infection risk
Neutropenia
Neutropenia is an abnormally low concentration of neutrophils (a type of white blood cell) in the blood. Neutrophils make up the majority of circulating white blood cells and serve as the primary defense against infections by destroying bacteri ...
is a distinguishing feature of GSD Ib, absent in GSD Ia. The microbiological cause of neutropenia in GSD Ib is not well understood. Broadly, the problem arises from compromised cellular metabolism in the neutrophil, resulting in accelerated neutrophil apoptosis. The neutropenia in GSD is characterized by both a decrease in absolute neutrophil count and diminished neutrophil function. Neutrophils use a specific G6P metabolic pathway which relies on the presence of G6Pase-β or G6PT to maintain energy homeostasis within the cell. The absence of G6PT in GSD Ib limits this pathway, leading to endoplasmic reticulum
The endoplasmic reticulum (ER) is, in essence, the transportation system of the eukaryotic cell, and has many other important functions such as protein folding. It is a type of organelle made up of two subunits – rough endoplasmic reticulum ...
stress, oxidative stress within the neutrophil, triggering premature apoptosis. Granulocyte colony-stimulating factor
Granulocyte colony-stimulating factor (G-CSF or GCSF), also known as colony-stimulating factor 3 (CSF 3), is a glycoprotein that stimulates the bone marrow to produce granulocytes and stem cells and release them into the bloodstream.
Functiona ...
(G-CSF), available as filgrastim, can reduce the risk of infection. In some cases, G-CSF formulated as pegfilgrastim
Pegfilgrastim, sold under the brand name Neulasta among others, is a PEGylated form of the recombinant human granulocyte colony-stimulating factor (GCSF) analog filgrastim. It serves to stimulate the production of white blood cells (neutrophils) ...
, sold under the trade name Neulasta, may be used as a slow-acting alternative, requiring less frequent dosing.
Thrombocytopenia and blood clotting problems
Impaired platelet aggregation is an uncommon consequence of chronic hypoglycemia, seen in GSD I patients. Research has demonstrated decreased platelet function, characterized by decreasedprothrombin
Thrombin (, ''fibrinogenase'', ''thrombase'', ''thrombofort'', ''topical'', ''thrombin-C'', ''tropostasin'', ''activated blood-coagulation factor II'', ''blood-coagulation factor IIa'', ''factor IIa'', ''E thrombin'', ''beta-thrombin'', ''gamma- ...
consumption, abnormal aggregation reactions, prolonged bleeding time, and low platelet adhesiveness. Severity of platelet dysfunction typically correlates with clinical condition, with the most severe cases correlating with lactic acidosis and severely lipidemia. It may cause clinically significant bleeding, especially epistaxis
A nosebleed, also known as epistaxis, is bleeding from the nose. Blood can flow down into the stomach, and cause nausea and vomiting. In more severe cases, blood may come out of both nostrils. Rarely, bleeding may be so significant that low bl ...
. Additionally, GSD I patients may present with thrombocytopenia as a consequence of splenomegaly. In the setting of splenomegaly various hematologic factors may be sequestered in the tissues of the spleen as blood is filtered through the organ. This can diminish levels of platelets
Platelets, also called thrombocytes (from Greek θρόμβος, "clot" and κύτος, "cell"), are a component of blood whose function (along with the coagulation factors) is to react to bleeding from blood vessel injury by clumping, thereby ...
available in the bloodstream, leading to thrombocytopenia
Thrombocytopenia is a condition characterized by abnormally low levels of platelets, also known as thrombocytes, in the blood. It is the most common coagulation disorder among intensive care patients and is seen in a fifth of medical patients a ...
.
Developmental effects
Developmental delay
Global developmental delay is an umbrella term used when children are significantly delayed in their cognitive and physical development. It can be diagnosed when a child is delayed in one or more milestones, categorised into motor skills, speech ...
is a potential secondary effect of chronic or recurrent hypoglycemia, but is at least theoretically preventable. Normal neuronal and muscle cells do not express glucose-6-phosphatase, and are thus not impacted by GSD I directly. However, without proper treatment of hypoglycemia, growth failure
Failure to thrive (FTT), also known as weight faltering or faltering growth, indicates insufficient weight gain or absence of appropriate physical growth in children. FTT is usually defined in terms of weight, and can be evaluated either by a low ...
commonly results from chronically low insulin levels, persistent acidosis, chronic elevation of catabolic hormones, and calorie
The calorie is a unit of energy. For historical reasons, two main definitions of "calorie" are in wide use. The large calorie, food calorie, or kilogram calorie was originally defined as the amount of heat needed to raise the temperature of o ...
insufficiency (or malabsorption
Malabsorption is a state arising from abnormality in absorption of food nutrients across the gastrointestinal (GI) tract. Impairment can be of single or multiple nutrients depending on the abnormality. This may lead to malnutrition and a variety ...
). The most dramatic developmental delays are often the cause of severe (not just persistent) episodes of hypoglycemia.
Diagnosis
Several different problems may lead to the diagnosis, usually by two years of age: * seizures or other manifestations of severe fasting hypoglycemia * hepatomegaly with abdominal protuberance * hyperventilation and apparent respiratory distress due to metabolic acidosis * episodes of vomiting due to metabolic acidosis, often precipitated by minor illness and accompanied by hypoglycemia Once the diagnosis is suspected, the multiplicity of clinical and laboratory features usually makes a strong circumstantial case. If hepatomegaly, fasting hypoglycemia, and poor growth are accompanied by lactic acidosis, hyperuricemia, hypertriglyceridemia, and enlarged kidneys by ultrasound, GSD I is the most likely diagnosis. The differential diagnosis list includes glycogenoses types III and VI, fructose 1,6-bisphosphatase deficiency, and a few other conditions (page 5), but none are likely to produce all of the features of GSD I. The next step is usually a carefully monitored fast. Hypoglycemia often occurs within six hours. A critical blood specimen obtained at the time of hypoglycemia typically reveals a mild metabolic acidosis, high free fatty acids and beta-hydroxybutyrate, very low insulin levels, and high levels of glucagon, cortisol, and growth hormone. Administration of intramuscular or intravenous glucagon (0.25 to 1 mg, depending on age) or epinephrine produces little rise of blood sugar. The diagnosis is definitively confirmed by liver biopsy with electron microscopy and assay of glucose-6-phosphatase activity in the tissue and/or specific gene testing, available in recent years.Treatment
The primary treatment goal is prevention of hypoglycemia and the secondary metabolic derangements by frequent feedings of foods high in glucose or starch (which is readily digested to glucose). To compensate for the inability of the liver to provide sugar, the total amount of dietary carbohydrate should approximate the 24-hour glucose production rate. The diet should contain approximately 65–70% carbohydrate, 10–15% protein, and 20–25% fat. At least a third of the carbohydrates should be supplied through the night, so that a young child goes no more than 3–4 hours without carbohydrate intake. Once a diagnosis is made, the priority in GSD I treatment is to maintain an adequate blood glucose. Patients aim to maintain a blood glucose above the 72 mg/dL (4.0 mmol/L) cutoff for hypoglycemia. GSD Ib patients have an additional treatment priority relating to neutropenia. Proper management of blood glucose in GSD I is critical in avoiding the more severe effects of high leves oflactic acid
Lactic acid is an organic acid. It has a molecular formula . It is white in the solid state and it is miscible with water. When in the dissolved state, it forms a colorless solution. Production includes both artificial synthesis as well as nat ...
and uric acid in the blood, and the development of hepatic adenomas.
In the last 30 years, two methods have been used to achieve this goal in young children: (1) continuous nocturnal gastric infusion of glucose or starch; and (2) night-time feedings of uncooked cornstarch. An elemental formula, glucose polymer, and/or cornstarch can be infused continuously through the night at a rate supplying 0.5–0.6 g/kg/h of glucose for an infant, or 0.3–0.4 for an older child. This method requires a nasogastric or gastrostomy tube and pump. Sudden death from hypoglycemia has occurred due to malfunction or disconnection, and periodic cornstarch feedings are now preferred to continuous infusion.
Cornstarch is an inexpensive way to provide gradually digested glucose. One tablespoon contains nearly 9 g carbohydrate (36 calories). Although it is safer, less expensive, and requires no equipment, this method does require that parents arise every 3–4 hours to administer the cornstarch. A typical requirement for a young child is 1.6 g/kg every 4 hours.
Long-term management should eliminate hypoglycemic symptoms and maintain normal growth. Treatment should achieve normal glucose, lactic acid, and electrolyte levels, and only mild elevations of uric acid and triglycerides.
Avoidance of other sugars
Intake ofcarbohydrate
In organic chemistry, a carbohydrate () is a biomolecule consisting of carbon (C), hydrogen (H) and oxygen (O) atoms, usually with a hydrogen–oxygen atom ratio of 2:1 (as in water) and thus with the empirical formula (where ''m'' may o ...
s which must be converted to G6P to be utilized (e.g., galactose
Galactose (, '' galacto-'' + ''-ose'', "milk sugar"), sometimes abbreviated Gal, is a monosaccharide sugar that is about as sweet as glucose, and about 65% as sweet as sucrose. It is an aldohexose and a C-4 epimer of glucose. A galactose molecu ...
and fructose
Fructose, or fruit sugar, is a ketonic simple sugar found in many plants, where it is often bonded to glucose to form the disaccharide sucrose. It is one of the three dietary monosaccharides, along with glucose and galactose, that are absorb ...
) should be minimized. Although elemental formulas are available for infants, many foods contain fructose or galactose in the forms of sucrose
Sucrose, a disaccharide, is a sugar composed of glucose and fructose subunits. It is produced naturally in plants and is the main constituent of white sugar. It has the molecular formula .
For human consumption, sucrose is extracted and refine ...
or lactose
Lactose is a disaccharide sugar synthesized by galactose and glucose subunits and has the molecular formula C12H22O11. Lactose makes up around 2–8% of milk (by mass). The name comes from ' (gen. '), the Latin word for milk, plus the suffix ' ...
. Adherence becomes a contentious treatment issue after infancy.
Other therapeutic measures
Persistent elevation of uric acid above 6.5 mg/dl warrants treatment with allopurinol to prevent uric acid deposition in kidneys and joints. Because of the potential for impaired platelet function, coagulation ability should be checked and the metabolic state normalized before surgery. Bleeding time may be normalized with 1–2 days of glucose loading, and improved with ddavp. During surgery, IV fluids should contain 10% dextrose and no lactate. A patient with GSD, type 1b was treated with a liver transplant at UCSF Medical Center in 1993 that resulted in the resolution of hypoglycemic episodes and the need for the patient to stay away from natural sources of sugar. Other patients have undergone this procedure as well with positive results. Although a liver transplant resulted in the resolution of hypoglycemia it did not however resolve the chronic neutropenia and the risk of infection among patients.Treatment of acute metabolic acidosis episodes
The most significant acute problem in childhood is a vulnerability to episodes of metabolic acidosis precipitated by minor illnesses. If a vomiting illness persists longer than 2–4 hours, the child should be seen and assessed for dehydration, acidosis, and hypoglycemia. If these are developing, intravenous fluids should be provided at a rate above maintenance. For mild acidosis, an effective fluid is 10% dextrose in ½ normal saline with 20 mEq/L KCl, but if acidosis is severe, 75–100 mEq/L and 20 mEq/L of K acetate can be substituted for the NaCl and KCl.Metabolic control
Metabolic control often diminishes during and after puberty, as a result of a patient outgrowing their dietary treatment plan.Prognosis
Without adequate metabolic treatment, patients with GSD I have died in infancy or childhood of overwhelming hypoglycemia and acidosis. Those who survived were stunted in physical growth and delayed in puberty because of chronically low insulin levels.Intellectual disability
Intellectual disability (ID), also known as general learning disability in the United Kingdom and formerly mental retardation, Rosa's Law, Pub. L. 111-256124 Stat. 2643(2010). is a generalized neurodevelopmental disorder characterized by signif ...
resulting from recurrent, severe hypoglycemia is considered preventable with appropriate treatment.
Liver complications have been serious in some patients. Adenoma
An adenoma is a benign tumor of epithelial tissue with glandular origin, glandular characteristics, or both. Adenomas can grow from many glandular organs, including the adrenal glands, pituitary gland, thyroid, prostate, and others. Some adenom ...
s of the liver can develop in the second decade or later, with a small chance of later malignant transformation to hepatoma or hepatic carcinomas (detectable by alpha-fetoprotein screening). Several children with advanced hepatic complications have improved after liver transplantation.
Additional problems reported in adolescents and adults with GSD I have included hyperuricemic gout
Gout ( ) is a form of inflammatory arthritis characterized by recurrent attacks of a red, tender, hot and swollen joint, caused by deposition of monosodium urate monohydrate crystals. Pain typically comes on rapidly, reaching maximal intens ...
, pancreatitis
Pancreatitis is a condition characterized by inflammation of the pancreas. The pancreas is a large organ behind the stomach that produces digestive enzymes and a number of hormones. There are two main types: acute pancreatitis, and chronic p ...
, and chronic kidney failure
Kidney failure, also known as end-stage kidney disease, is a medical condition in which the kidneys can no longer adequately filter waste products from the blood, functioning at less than 15% of normal levels. Kidney failure is classified as eit ...
. Despite hyperlipidemia
Hyperlipidemia is abnormally elevated levels of any or all lipids (fats, cholesterol, or triglycerides) or lipoproteins in the blood. citing: and The term ''hyperlipidemia'' refers to the laboratory finding itself and is also used as an umbre ...
, atherosclerotic complications are uncommon.
With diagnosis before serious harm occurs, prompt reversal of acidotic episodes, and appropriate long-term treatment, most children will be healthy. With exceptions and qualifications, adult health and life span may also be fairly good, although lack of effective treatment before the mid-1980s means information on long-term efficacy is limited.
Epidemiology
In the United States, GSD I has an incidence of approximately 1 in 50,000 to 100,000https://rarediseases.org/rare-diseases/glycogen-storage-disease-type-i/ Nation Organization for Rare Disorders births. None of the glycogenoses are currently detected by standard or extendednewborn screening
Newborn screening (NBS) is a public health program of screening in infants shortly after birth for conditions that are treatable, but not clinically evident in the newborn period. The goal is to identify infants at risk for these conditions ea ...
.
The disease is more common in people of Ashkenazi Jewish
Ashkenazi Jews ( ; he, יְהוּדֵי אַשְׁכְּנַז, translit=Yehudei Ashkenaz, ; yi, אַשכּנזישע ייִדן, Ashkenazishe Yidn), also known as Ashkenazic Jews or ''Ashkenazim'',, Ashkenazi Hebrew pronunciation: , singu ...
, Mexican, Chinese, and Japanese descent.
References
Further reading
GeneReview/NIH/UW entry on Glycogen Storage Disease Type I
External links
* {{DEFAULTSORT:Glycogen Storage Disease Type I Autosomal recessive disorders Hepatology Inborn errors of carbohydrate metabolism