Lupus, technically known as systemic lupus erythematosus (SLE), is an
autoimmune disease in which the body's
immune system
The immune system is a network of biological processes that protects an organism from diseases. It detects and responds to a wide variety of pathogens, from viruses to parasitic worms, as well as cancer cells and objects such as wood splint ...
mistakenly attacks healthy tissue in many parts of the body.
Symptoms vary among people and may be mild to severe.
[ Common symptoms include painful and swollen joints, ]fever
Fever, also referred to as pyrexia, is defined as having a temperature above the normal range due to an increase in the body's temperature set point. There is not a single agreed-upon upper limit for normal temperature with sources using val ...
, chest pain, hair loss
Hair loss, also known as alopecia or baldness, refers to a loss of hair from part of the head or body. Typically at least the head is involved. The severity of hair loss can vary from a small area to the entire body. Inflammation or scar ...
, mouth ulcer
A mouth ulcer (aphtha) is an ulcer that occurs on the mucous membrane of the oral cavity. Mouth ulcers are very common, occurring in association with many diseases and by many different mechanisms, but usually there is no serious underlying ca ...
s, swollen lymph nodes, feeling tired, and a red rash
A rash is a change of the human skin which affects its color, appearance, or texture.
A rash may be localized in one part of the body, or affect all the skin. Rashes may cause the skin to change color, itch, become warm, bumpy, chapped, dry, c ...
which is most commonly on the face.[ Often there are periods of illness, called flares, and periods of remission during which there are few symptoms.][
The cause of SLE is not clear.][ It is thought to involve a mixture of ]genetics
Genetics is the study of genes, genetic variation, and heredity in organisms.Hartl D, Jones E (2005) It is an important branch in biology because heredity is vital to organisms' evolution. Gregor Mendel, a Moravian Augustinian friar wor ...
combined with environmental factor
An environmental factor, ecological factor or eco factor is any factor, abiotic or biotic, that influences living organisms. Abiotic factors include ambient temperature, amount of sunlight, and pH of the water soil in which an organism lives. Bi ...
s.[ Among ]identical twins
Twins are two offspring produced by the same pregnancy.MedicineNet > Definition of TwinLast Editorial Review: 19 June 2000 Twins can be either ''monozygotic'' ('identical'), meaning that they develop from one zygote, which splits and forms two em ...
, if one is affected there is a 24% chance the other one will also develop the disease.[ Female sex hormones, sunlight, smoking, ]vitamin D deficiency
Vitamin D deficiency or hypovitaminosis D is a vitamin D level that is below normal. It most commonly occurs in people when they have inadequate exposure to sunlight, particularly sunlight with adequate ultraviolet B rays (UVB). Vitamin D defic ...
, and certain infections are also believed to increase a person's risk.[ The mechanism involves an immune response by autoantibodies against a person's own tissues.][ These are most commonly ]anti-nuclear antibodies
Antinuclear antibodies (ANAs, also known as antinuclear factor or ANF) are autoantibodies that bind to contents of the cell nucleus. In normal individuals, the immune system produces antibodies to foreign proteins (antigens) but not to human prote ...
and they result in inflammation
Inflammation (from la, inflammatio) is part of the complex biological response of body tissues to harmful stimuli, such as pathogens, damaged cells, or irritants, and is a protective response involving immune cells, blood vessels, and molec ...
.[ Diagnosis can be difficult and is based on a combination of symptoms and laboratory tests.][ There are a number of other kinds of ]lupus erythematosus
Lupus erythematosus is a collection of autoimmune diseases in which the human immune system becomes hyperactive and attacks healthy tissues. Symptoms of these diseases can affect many different body systems, including joints, skin, kidneys, blo ...
including discoid lupus erythematosus
Discoid lupus erythematosus is the most common type of chronic cutaneous lupus (CCLE), an autoimmune skin condition on the lupus erythematosus spectrum of illnesses. It presents with red, painful, inflamed and coin-shaped patches of skin with a sc ...
, neonatal lupus
Neonatal lupus erythematosus is an autoimmune disease in an infant born to a mother with anti-Ro/SSA and with or without anti-La/SSB antibodies. The disease most commonly presents with a rash resembling subacute cutaneous lupus erythematosus and ...
, and subacute cutaneous lupus erythematosus.[
There is no cure for SLE,][ but there are experimental and symptomatic treatments. Treatments may include ]NSAID
Non-steroidal anti-inflammatory drugs (NSAID) are members of a therapeutic drug class which reduces pain, decreases inflammation, decreases fever, and prevents blood clots. Side effects depend on the specific drug, its dose and duration of ...
s, corticosteroids, immunosuppressants
Immunosuppressive drugs, also known as immunosuppressive agents, immunosuppressants and antirejection medications, are drugs that inhibit or prevent activity of the immune system.
Classification
Immunosuppressive drugs can be classified int ...
, hydroxychloroquine
Hydroxychloroquine, sold under the brand name Plaquenil among others, is a medication used to prevent and treat malaria in areas where malaria remains sensitive to chloroquine. Other uses include treatment of rheumatoid arthritis, lupus, an ...
, and methotrexate.[ Although corticosteroids are rapidly effective, long-term use results in side effects. Alternative medicine has not been shown to affect the disease.][ Life expectancy is lower among people with SLE, but with modern treatment, 80-90% of patients can have a normal life span.][ While women with lupus have higher risk pregnancies, most are successful.][
Rate of SLE varies between countries from 20 to 70 per 100,000.][ Women of childbearing age are affected about nine times more often than men.]Chinese
Chinese can refer to:
* Something related to China
* Chinese people, people of Chinese nationality, citizenship, and/or ethnicity
**''Zhonghua minzu'', the supra-ethnic concept of the Chinese nation
** List of ethnic groups in China, people of ...
descent are at higher risk than those of European descent.[ Rates of disease in the developing world are unclear.]
Signs and symptoms
 SLE is one of several diseases known as "
SLE is one of several diseases known as "the great imitator
The Great Imitator (also the Great Masquerader) is a phrase used for medical conditions that feature nonspecific symptoms and may be confused with a number of other diseases.J.C. Segen. The Dictionary of Modern Medicine'. CRC Press; 1992. . p. 265 ...
" because it often mimics or is mistaken for other illnesses. SLE is a classical item in differential diagnosis,fever
Fever, also referred to as pyrexia, is defined as having a temperature above the normal range due to an increase in the body's temperature set point. There is not a single agreed-upon upper limit for normal temperature with sources using val ...
, malaise, joint pains, muscle pains
Myalgia (also called muscle pain and muscle ache in layman's terms) is the medical term for muscle pain. Myalgia is a symptom of many diseases. The most common cause of acute myalgia is the overuse of a muscle or group of muscles; another lik ...
, and fatigue. Because these symptoms are so often seen in association with other diseases, these signs and symptoms are not part of the diagnostic criteria for SLE. When occurring in conjunction with other signs and symptoms, however, they are considered suggestive.relapse
In internal medicine, relapse or recidivism is a recurrence of a past (typically medical) condition. For example, multiple sclerosis and malaria often exhibit peaks of activity and sometimes very long periods of dormancy, followed by relapse or ...
s, a low white blood cell count, more arthritis, Raynaud's phenomenon
Raynaud syndrome, also known as Raynaud's phenomenon, eponymously named after the physician Auguste Gabriel Maurice Raynaud, who first described it in his doctoral thesis in 1862, is a medical condition in which the spasm of small arteries cau ...
, and psychiatric symptoms. Males tend to have more seizure
An epileptic seizure, informally known as a seizure, is a period of symptoms due to abnormally excessive or synchronous neuronal activity in the brain. Outward effects vary from uncontrolled shaking movements involving much of the body with l ...
s, kidney disease, serositis
Serositis refers to inflammation of the serous tissues of the body, the tissues lining the lungs (pleura), heart (pericardium), and the inner lining of the abdomen (peritoneum) and organs within. It is commonly found with fat wrapping or creeping ...
(inflammation of tissues lining the lungs and heart), skin problems, and peripheral neuropathy
Peripheral neuropathy, often shortened to neuropathy, is a general term describing disease affecting the peripheral nerves, meaning nerves beyond the brain and spinal cord. Damage to peripheral nerves may impair sensation, movement, gland, or or ...
.
Skin
As many as 70% of people with lupus have some skin symptoms. The three main categories of lesions are chronic cutaneous (discoid) lupus, subacute cutaneous lupus, and acute cutaneous lupus. People with discoid lupus may exhibit thick, red scaly patches on the skin. Similarly, subacute cutaneous lupus manifests as red, scaly patches of skin but with distinct edges. Acute cutaneous lupus manifests as a rash. Some have the classic malar rash (commonly known as the ''butterfly rash'') associated with the disease. This rash occurs in 30 to 60% of people with SLE.
Hair loss
Hair loss, also known as alopecia or baldness, refers to a loss of hair from part of the head or body. Typically at least the head is involved. The severity of hair loss can vary from a small area to the entire body. Inflammation or scar ...
, mouth and nasal ulcers, and lesions on the skin are other possible manifestations.
Muscles and bones
The most commonly sought medical attention is for joint pain
Arthralgia (from Greek ''arthro-'', joint + ''-algos'', pain) literally means ''joint pain''. Specifically, arthralgia is a symptom of injury, infection, illness (in particular arthritis), or an allergic reaction to medication.
According to MeSH, ...
, with the small joints of the hand and wrist usually affected, although all joints are at risk. More than 90 percent of those affected will experience joint or muscle pain at some time during the course of their illness.[Joint and Muscle Pain](_blank)
Lupus Foundation of America Unlike rheumatoid arthritis
Rheumatoid arthritis (RA) is a long-term autoimmune disorder that primarily affects joints. It typically results in warm, swollen, and painful joints. Pain and stiffness often worsen following rest. Most commonly, the wrist and hands are invol ...
, lupus arthritis is less disabling and usually does not cause severe destruction of the joints. Fewer than ten percent of people with lupus arthritis will develop deformities of the hands and feet.tuberculosis
Tuberculosis (TB) is an infectious disease usually caused by '' Mycobacterium tuberculosis'' (MTB) bacteria. Tuberculosis generally affects the lungs, but it can also affect other parts of the body. Most infections show no symptoms, i ...
.rheumatoid arthritis
Rheumatoid arthritis (RA) is a long-term autoimmune disorder that primarily affects joints. It typically results in warm, swollen, and painful joints. Pain and stiffness often worsen following rest. Most commonly, the wrist and hands are invol ...
and SLE has been suggested,
Blood
Anemia
Anemia or anaemia (British English) is a blood disorder in which the blood has a reduced ability to carry oxygen due to a lower than normal number of red blood cells, or a reduction in the amount of hemoglobin. When anemia comes on slowly, t ...
is common in children with SLEthrombocytopenia
Thrombocytopenia is a condition characterized by abnormally low levels of platelets, also known as thrombocytes, in the blood. It is the most common coagulation disorder among intensive care patients and is seen in a fifth of medical patients a ...
) and low white blood cell count (leukopenia
Leukopenia () is a decrease in the number of leukocytes (WBC). Found in the blood, they are the white blood cells, and are the body's primary defense against an infection. Thus the condition of leukopenia places individuals at increased risk of in ...
) may be due to the disease or a side effect of pharmacological treatment. People with SLE may have an association with antiphospholipid antibody syndrome
Antiphospholipid syndrome, or antiphospholipid antibody syndrome (APS or APLS), is an autoimmune, hypercoagulable state caused by antiphospholipid antibodies. APS provokes blood clots (thrombosis) in both arteries and veins as well as pregnancy- ...
partial thromboplastin time
The partial thromboplastin time (PTT), also known as the activated partial thromboplastin time (aPTT or APTT), is a blood test that characterizes coagulation of the blood. A historical name for this measure is the kaolin-cephalin clotting time ( ...
(which usually occurs in hemorrhagic disorders) and a positive test for antiphospholipid antibodies; the combination of such findings have earned the term "lupus anticoagulant
Lupus anticoagulant is an immunoglobulin that binds to phospholipids and proteins associated with the cell membrane. Its name is a partial misnomer, as it is actually a prothrombotic antibody ''in vivo''. Lupus anticoagulant in living systems c ...
-positive". Another autoantibody finding in SLE is the anti-cardiolipin antibody, which can cause a false positive test for syphilis.
Heart
SLE may cause pericarditis—inflammation of the outer lining surrounding the heart, myocarditis—inflammation of the heart muscle, or endocarditis
Endocarditis is an inflammation of the inner layer of the heart, the endocardium. It usually involves the heart valves. Other structures that may be involved include the interventricular septum, the chordae tendineae, the mural endocardium, or the ...
—inflammation of the inner lining of the heart. The endocarditis of SLE is non-infectious, and is also called Libman–Sacks endocarditis. It involves either the mitral valve or the tricuspid valve
The tricuspid valve, or right atrioventricular valve, is on the right dorsal side of the mammalian heart, at the superior portion of the right ventricle. The function of the valve is to allow blood to flow from the right atrium to the right ven ...
. Atherosclerosis
Atherosclerosis is a pattern of the disease arteriosclerosis in which the wall of the artery develops abnormalities, called lesions. These lesions may lead to narrowing due to the buildup of atheromatous plaque. At onset there are usually no s ...
also occurs more often and advances more rapidly than in the general population.
Steroids are sometimes prescribed as an anti-inflammatory treatment for lupus; however, they can increase one's risk for heart disease, high cholesterol, and atherosclerosis.
Lungs
SLE can cause pleuritic pain as well as inflammation of the pleurae
The pulmonary pleurae (''sing.'' pleura) are the two opposing layers of serous membrane overlying the lungs and the inside of the surrounding chest walls.
The inner pleura, called the visceral pleura, covers the surface of each lung and dips be ...
known as pleurisy
Pleurisy, also known as pleuritis, is inflammation of the membranes that surround the lungs and line the chest cavity ( pleurae). This can result in a sharp chest pain while breathing. Occasionally the pain may be a constant dull ache. Other sy ...
, which can rarely give rise to shrinking lung syndrome involving a reduced lung volume.pneumonitis
Pneumonitis describes general inflammation of lung tissue. Possible causative agents include radiation therapy of the chest, exposure to medications used during chemo-therapy, the inhalation of debris (e.g., animal dander), aspiration, herbicide ...
, chronic diffuse interstitial lung disease
Interstitial lung disease (ILD), or diffuse parenchymal lung disease (DPLD), is a group of respiratory diseases affecting the interstitium (the tissue and space around the alveoli (air sacs)) of the lungs. It concerns alveolar epithelium, pu ...
, pulmonary hypertension, pulmonary emboli, and pulmonary hemorrhage
Pulmonary hemorrhage (or pulmonary haemorrhage) is an acute bleeding from the lung, from the upper respiratory tract and the trachea, and the pulmonary alveoli. When evident clinically, the condition is usually massive. .
Kidneys
Painless passage of blood
Blood is a body fluid in the circulatory system of humans and other vertebrates that delivers necessary substances such as nutrients and oxygen to the cells, and transports metabolic waste products away from those same cells. Blood in the cir ...
or protein in the urine may often be the only presenting sign of kidney involvement. Acute or chronic renal impairment may develop with lupus nephritis
Lupus nephritis is an inflammation of the kidneys caused by systemic lupus erythematosus (SLE), an autoimmune disease. It is a type of glomerulonephritis in which the glomeruli become inflamed. Since it is a result of SLE, this type of glomerulo ...
, leading to acute or end-stage kidney failure
Kidney failure, also known as end-stage kidney disease, is a medical condition in which the kidneys can no longer adequately filter waste products from the blood, functioning at less than 15% of normal levels. Kidney failure is classified as eit ...
. Because of early recognition and management of SLE with immunosuppressive drugs or corticosteroids, end-stage renal failure occurs in less than 5%glomerulonephritis
Glomerulonephritis (GN) is a term used to refer to several kidney diseases (usually affecting both kidneys). Many of the diseases are characterised by inflammation either of the glomeruli or of the small blood vessels in the kidneys, hence the ...
with "wire loop" abnormalities. This finding is due to immune complex deposition along the glomerular basement membrane, leading to a typical granular appearance in immunofluorescence testing.
Neuropsychiatric
Neuropsychiatric
Neuropsychiatry or Organic Psychiatry is a branch of medicine that deals with psychiatry as it relates to neurology, in an effort to understand and attribute behavior to the interaction of neurobiology and social psychology factors. Within neurop ...
syndromes can result when SLE affects the central or peripheral nervous system
The peripheral nervous system (PNS) is one of two components that make up the nervous system of bilateral animals, with the other part being the central nervous system (CNS). The PNS consists of nerves and ganglia, which lie outside the brain ...
. The American College of Rheumatology The American College of Rheumatology (ACR; until 1985 called American Rheumatism Association) is an organization of and for physicians, health professionals, and scientists that advances rheumatology through programs of education, research, advocacy ...
defines 19 neuropsychiatric syndromes in systemic lupus erythematosus.cognitive dysfunction
Cognitive disorders (CDs), also known as neurocognitive disorders (NCDs), are a category of mental health disorders that primarily affect cognitive abilities including learning, memory, perception, and problem solving. Neurocognitive disorders i ...
, mood disorder
A mood disorder, also known as an affective disorder, is any of a group of conditions of mental and behavioral disorder where a disturbance in the person's mood is the main underlying feature. The classification is in the '' Diagnostic and St ...
, cerebrovascular disease
Cerebrovascular disease includes a variety of medical conditions that affect the blood vessels of the brain and the cerebral circulation. Arteries supplying oxygen and nutrients to the brain are often damaged or deformed in these disorders. Th ...
,seizures
An epileptic seizure, informally known as a seizure, is a period of symptoms due to abnormally excessive or synchronous neuronal activity in the brain. Outward effects vary from uncontrolled shaking movements involving much of the body with l ...
, polyneuropathy,psychosis
Psychosis is a condition of the mind that results in difficulties determining what is real and what is not real. Symptoms may include delusions and hallucinations, among other features. Additional symptoms are incoherent speech and behavior ...
, depression, and in some extreme cases, personality disorders. Steroid psychosis can also occur as a result of treating the disease.intracranial pressure
Intracranial pressure (ICP) is the pressure exerted by fluids such as cerebrospinal fluid (CSF) inside the skull and on the brain tissue. ICP is measured in millimeters of mercury ( mmHg) and at rest, is normally 7–15 mmHg for a supine adult ...
, papilledema
Papilledema or papilloedema is optic disc swelling that is caused by increased intracranial pressure due to any cause. The swelling is usually bilateral and can occur over a period of hours to weeks. Unilateral presentation is extremely rare.
In ...
, and headache with occasional abducens nerve
The abducens nerve or abducent nerve, also known as the sixth cranial nerve, cranial nerve VI, or simply CN VI, is a cranial nerve in humans and various other animals that controls the movement of the lateral rectus muscle, one of the extraocul ...
paresis
In medicine, paresis () is a condition typified by a weakness of voluntary movement, or by partial loss of voluntary movement or by impaired movement. When used without qualifiers, it usually refers to the limbs, but it can also be used to desc ...
, absence of a space-occupying lesion or ventricular enlargement, and normal cerebrospinal fluid
Cerebrospinal fluid (CSF) is a clear, colorless body fluid found within the tissue that surrounds the brain and spinal cord of all vertebrates.
CSF is produced by specialised ependymal cells in the choroid plexus of the ventricles of the ...
chemical
A chemical substance is a form of matter having constant chemical composition and characteristic properties. Some references add that chemical substance cannot be separated into its constituent elements by physical separation methods, i.e., w ...
and hematological
Hematology ( always spelled haematology in British English) is the branch of medicine concerned with the study of the cause, prognosis, treatment, and prevention of diseases related to blood. It involves treating diseases that affect the produc ...
constituents.acute confusional state
Delirium (also known as acute confusional state) is an organically caused decline from a previous baseline of mental function that develops over a short period of time, typically hours to days. Delirium is a syndrome encompassing disturbances in ...
, Guillain–Barré syndrome
Guillain–Barré syndrome (GBS) is a rapid-onset muscle weakness caused by the immune system damaging the peripheral nervous system. Typically, both sides of the body are involved, and the initial symptoms are changes in sensation or pain oft ...
, aseptic meningitis
Aseptic meningitis is the inflammation of the meninges, a membrane covering the brain and spinal cord, in patients whose cerebral spinal fluid test result is negative with routine bacterial cultures. Aseptic meningitis is caused by viruses, my ...
, autonomic disorder, demyelinating syndrome, mononeuropathy (which might manifest as mononeuritis multiplex
Peripheral neuropathy, often shortened to neuropathy, is a general term describing disease affecting the peripheral nerves, meaning nerves beyond the brain and spinal cord. Damage to peripheral nerves may impair sensation, movement, gland, or or ...
), movement disorder
Movement disorder refers to any clinical syndrome with either an excess of movement or a paucity of voluntary and involuntary movements, unrelated to weakness or spasticity. Movement disorders are synonymous with basal ganglia or extrapyramidal ...
(more specifically, chorea
Chorea (or choreia, occasionally) is an abnormal involuntary movement disorder, one of a group of neurological disorders called dyskinesias. The term ''chorea'' is derived from the grc, χορεία ("dance"; see choreia), as the quick movem ...
), myasthenia gravis, myelopathy
Myelopathy describes any neurologic deficit related to the spinal cord. The most common form of myelopathy in humans, ''Spinal cord compression, cervical spondylotic myelopathy (CSM)'', also called ''degenerative cervical myelopathy'', results fro ...
, cranial neuropathy and plexopathy Plexopathy is a disorder of the wikt:network, network of nerves in the brachial plexus, brachial or lumbosacral plexus. Symptoms include pain, muscle weakness, and sensory deficits (numbness).
Types
There are two main types of plexopathy, based on ...
.
Neurological disorders contribute to a significant percentage of morbidity and mortality in people with lupus.
Eyes
Eye involvement is seen in up to one-third of people. The most common diseases are dry eye syndrome
Dry eye syndrome (DES), also known as keratoconjunctivitis sicca (KCS), is the condition of having dry eyes. Other associated symptoms include irritation, redness, discharge, and easily fatigued eyes. Blurred vision may also occur. Symptoms range ...
and secondary Sjögren's syndrome, but episcleritis
Episcleritis is a benign, self-limiting inflammatory disease affecting part of the eye called the episclera. The episclera is a thin layer of tissue that lies between the conjunctiva and the connective tissue layer that forms the white of the e ...
, scleritis
Scleritis is a serious inflammatory disease that affects the white outer coating of the eye, known as the sclera. The disease is often contracted through association with other diseases of the body, such as granulomatosis with polyangiitis or ...
, retinopathy
Retinopathy is any damage to the retina of the eyes, which may cause vision impairment. Retinopathy often refers to retinal vascular disease, or damage to the retina caused by abnormal blood flow. Age-related macular degeneration is technically inc ...
(more often affecting both eyes than one), ischemic optic neuropathy
Ischemic optic neuropathy (ION) is the loss of structure and function of a portion of the optic nerve due to obstruction of blood flow to the nerve (i.e. ischemia). Ischemic forms of optic neuropathy are typically classified as either anterior is ...
, retinal detachment, and secondary angle-closure glaucoma may occur. In addition, the medications used to treat SLE can cause eye disease: long-term glucocorticoid
Glucocorticoids (or, less commonly, glucocorticosteroids) are a class of corticosteroids, which are a class of steroid hormones. Glucocorticoids are corticosteroids that bind to the glucocorticoid receptor that is present in almost every verteb ...
use can cause cataract
A cataract is a cloudy area in the lens of the eye that leads to a decrease in vision. Cataracts often develop slowly and can affect one or both eyes. Symptoms may include faded colors, blurry or double vision, halos around light, trouble ...
s and secondary open-angle glaucoma, and long-term hydroxychloroquine
Hydroxychloroquine, sold under the brand name Plaquenil among others, is a medication used to prevent and treat malaria in areas where malaria remains sensitive to chloroquine. Other uses include treatment of rheumatoid arthritis, lupus, an ...
treatment can cause vortex keratopathy and maculopathy
A maculopathy is any pathological condition of the macula, an area at the centre of the retina that is associated with highly sensitive, accurate vision.
Forms of maculopathies
* Age-Related Macular Degeneration is a degenerative maculopathy ass ...
.
Reproductive
While most pregnancies have positive outcomes, there is a greater risk of adverse events occurring during pregnancy. SLE causes an increased rate of fetal death ''in utero'' and spontaneous abortion (miscarriage). The overall live-birth rate in people with SLE has been estimated to be 72%. Pregnancy outcome appears to be worse in people with SLE whose disease flares up during pregnancy.
Neonatal lupus
Neonatal lupus erythematosus is an autoimmune disease in an infant born to a mother with anti-Ro/SSA and with or without anti-La/SSB antibodies. The disease most commonly presents with a rash resembling subacute cutaneous lupus erythematosus and ...
is the occurrence of SLE symptoms in an infant born from a mother with SLE, most commonly presenting with a rash resembling discoid lupus erythematosus
Discoid lupus erythematosus is the most common type of chronic cutaneous lupus (CCLE), an autoimmune skin condition on the lupus erythematosus spectrum of illnesses. It presents with red, painful, inflamed and coin-shaped patches of skin with a sc ...
, and sometimes with systemic abnormalities such as heart block
Heart block (HB) is a disorder in the heart's rhythm due to a fault in the natural pacemaker. This is caused by an obstruction – a block – in the electrical conduction system of the heart. Sometimes a disorder can be inherited. Despite the se ...
or enlargement of the liver and spleen.[thefreedictionary.com > neonatal lupus]
Citing: Dorland's Medical Dictionary for Health Consumers. Copyright 2007 Neonatal lupus is usually benign and self-limited.[
Medications for treatment of SLE can carry severe risks for female and male reproduction. Cyclophosphamide (also known as Cytoxan), can lead to infertility by causing premature ovarian insufficiency (POI), the loss of normal function of one's ovaries prior to age forty. Methotrexate can cause termination or deformity in fetuses and is a common abortifacient, and for men taking a high dose and planning to father, a discontinuation period of 6 months is recommended before insemination.
]
Systemic
Fatigue in SLE is probably multifactorial and has been related to not only disease activity or complications such as anemia
Anemia or anaemia (British English) is a blood disorder in which the blood has a reduced ability to carry oxygen due to a lower than normal number of red blood cells, or a reduction in the amount of hemoglobin. When anemia comes on slowly, t ...
or hypothyroidism, but also to pain, depression, poor sleep
Sleep is a sedentary state of mind and body. It is characterized by altered consciousness, relatively inhibited sensory activity, reduced muscle activity and reduced interactions with surroundings. It is distinguished from wakefulness by a de ...
quality, poor physical fitness and lack of social support.
Causes
SLE is presumably caused by a genetic susceptibility coupled with an environmental trigger which results in defects in the immune system. One of the factors associated with SLE is vitamin D deficiency
Vitamin D deficiency or hypovitaminosis D is a vitamin D level that is below normal. It most commonly occurs in people when they have inadequate exposure to sunlight, particularly sunlight with adequate ultraviolet B rays (UVB). Vitamin D defic ...
.
Genetics
SLE does run in families, but no single causal gene has been identified. Instead, multiple genes appear to influence a person's chance of developing lupus when triggered by environmental factors. HLA class I, class II, and class III genes are associated with SLE, but only classes I and II contribute independently to increased risk
In simple terms, risk is the possibility of something bad happening. Risk involves uncertainty about the effects/implications of an activity with respect to something that humans value (such as health, well-being, wealth, property or the environm ...
of SLE.IRF5
Interferon regulatory factor 5 is a protein that in humans is encoded by the ''IRF5'' gene. The IRF family is a group of transcription factors that are involved in signaling for virus responses in mammals along with regulation of certain cellular ...
'', '' PTPN22'', ''STAT4
Signal transducer and activator of transcription 4 (STAT4) is a transcription factor belonging to the STAT protein family, composed of STAT1, STAT2, STAT3, STAT5A, STAT5B, STAT6. STAT proteins are key activators of gene transcription which bind ...
'',CDKN1A
p21Cip1 (alternatively p21Waf1), also known as cyclin-dependent kinase inhibitor 1 or CDK-interacting protein 1, is a cyclin-dependent kinase inhibitor (CKI) that is capable of inhibiting all cyclin/CDK complexes, though is primarily associated ...
'',monozygotic
Twins are two offspring produced by the same pregnancy.MedicineNet > Definition of TwinLast Editorial Review: 19 June 2000 Twins can be either ''monozygotic'' ('identical'), meaning that they develop from one zygote, which splits and forms two ...
) twins were found to share susceptibility to the disease at >35% rate compared to fraternal (dizygotic
Twins are two offspring produced by the same pregnancy.MedicineNet > Definition of TwinLast Editorial Review: 19 June 2000 Twins can be either ''monozygotic'' ('identical'), meaning that they develop from one zygote, which splits and forms two em ...
) twins and other full siblings who only showed a 2–5% concordance in shared inheritance.oligogenic
Oligogenic inheritance (Greek ὀλίγος – ''ὀligos'' = few, a little) describes a trait that is influenced by a few genes. Oligogenic inheritance represents an intermediate between monogenic inheritance in which a trait is determined by a ...
trait, meaning that there are several genes that control susceptibility to the disease.
Drug reactions
Drug-induced lupus erythematosus
Drug-induced lupus erythematosus is an autoimmune disorder caused by chronic use of certain drugs. These drugs cause an autoimmune response (the body attacks its own cells) producing symptoms similar to those of systemic lupus erythematosus (SLE ...
is a (generally) reversible condition that usually occurs in people being treated for a long-term illness. Drug-induced lupus mimics SLE. However, symptoms of drug-induced lupus generally disappear once the medication that triggered the episode is stopped. More than 38 medications can cause this condition, the most common of which are procainamide
Procainamide (PCA) is a medication of the antiarrhythmic class used for the treatment of cardiac arrhythmias. It is classified by the Vaughan Williams classification system as class Ia; thus it is a sodium channel blocker of cardiomyocytes. In add ...
, isoniazid
Isoniazid, also known as isonicotinic acid hydrazide (INH), is an antibiotic used for the treatment of tuberculosis. For active tuberculosis it is often used together with rifampicin, pyrazinamide, and either streptomycin or ethambutol. For la ...
, hydralazine
Hydralazine, sold under the brand name Apresoline among others, is a medication used to treat high blood pressure and heart failure. This includes high blood pressure in pregnancy and very high blood pressure resulting in symptoms. It has been ...
, quinidine
Quinidine is a class I antiarrhythmic agent, class IA antiarrhythmic agent used to treat heart rhythm disturbances. It is the enantiomer of Antimalarial medication, antimalarial agent quinine, originally derived from the bark of the cinchona tre ...
, and phenytoin
Phenytoin (PHT), sold under the brand name Dilantin among others, is an anti-seizure medication. It is useful for the prevention of tonic-clonic seizures (also known as grand mal seizures) and focal seizures, but not absence seizures. The in ...
.
Non-systemic forms of lupus
Discoid (cutaneous) lupus is limited to skin symptoms and is diagnosed by biopsy of rash on the face, neck, scalp or arms. Approximately 5% of people with DLE progress to SLE.
Pathophysiology
SLE is triggered by environmental factors that are unknown. In SLE, the body's immune system produces antibodies against self-protein Self-protein refers to all proteins endogenously produced by DNA-level transcription and translation within an organism of interest. This does not include proteins synthesized due to viral infection, but may include those synthesized by commensal ...
, particularly against proteins in the cell nucleus. These antibody attacks are the immediate cause of SLE.titer
Titer (American English) or titre (British English) is a way of expressing concentration. Titer testing employs serial dilution to obtain approximate quantitative information from an analytical procedure that inherently only evaluates as positiv ...
s of anti-cardiolipin antibodies
Anti-cardiolipin antibodies (ACA) are antibodies often directed against cardiolipin and found in several diseases, including syphilis, antiphospholipid syndrome, livedoid vasculitis, vertebrobasilar insufficiency, Behçet's syndrome, idiopathic ...
, or a consequence of therapy.
People with SLE have intense polyclonal B-cell activation, with a population shift towards immature B cells. Memory B cells with increased CD27
CD27 is a member of the tumor necrosis factor receptor superfamily. It is currently of interest to immunologists as a co-stimulatory immune checkpoint molecule, and is the target of an anti-cancer drug in clinical trials.
Expression
During mous ...
+/ IgD—are less susceptible to immunosuppression. CD27-/IgD- memory B cells are associated with increased disease activity and renal lupus. T cells, which regulate B-cell responses and infiltrate target tissues, have defects in signaling, adhesion, co-stimulation, gene transcription, and alternative splicing. The cytokines B-lymphocyte stimulator (BLyS), also known as B-cell activating factor
B-cell activating factor (BAFF) also known as tumor necrosis factor ligand superfamily member 13B and CD257 among other names, is a protein that in humans is encoded by the ''TNFSF13B'' gene. BAFF is also known as B Lymphocyte Stimulator (BLyS) a ...
(BAFF), interleukin 6, interleukin 17, interleukin 18, type I interferons, and tumor necrosis factor α (TNFα) are involved in the inflammatory process and are potential therapeutic targets.
Cell death signaling
*Apoptosis is increased in monocyte
Monocytes are a type of leukocyte or white blood cell. They are the largest type of leukocyte in blood and can differentiate into macrophages and conventional dendritic cells. As a part of the vertebrate innate immune system monocytes also ...
s and keratinocyte
Keratinocytes are the primary type of cell found in the epidermis, the outermost layer of the skin. In humans, they constitute 90% of epidermal skin cells.
Basal cells in the basal layer (''stratum basale'') of the skin are sometimes referre ...
s
*Expression
Expression may refer to:
Linguistics
* Expression (linguistics), a word, phrase, or sentence
* Fixed expression, a form of words with a specific meaning
* Idiom, a type of fixed expression
* Metaphorical expression, a particular word, phrase, o ...
of Fas by B cells and T cell
A T cell is a type of lymphocyte. T cells are one of the important white blood cells of the immune system and play a central role in the adaptive immune response. T cells can be distinguished from other lymphocytes by the presence of a T-cell r ...
s is increased
*There are correlations between the apoptotic rates of lymphocytes and disease activity.
*Necrosis is increased in T lymphocytes.
Tingible body macrophage
A tingible body macrophage (TBMs) is a type of macrophage predominantly found in germinal centers, containing many phagocytosis, phagocytized, apoptosis, apoptotic cells in various states of degradation, referred to as tingible bodies (tingible me ...
s (TBMs) – large phagocytic cells
Phagocytes are cells that protect the body by ingesting harmful foreign particles, bacteria, and dead or dying cells. Their name comes from the Greek ', "to eat" or "devour", and "-cyte", the suffix in biology denoting "cell", from the Greek ' ...
in the germinal center
Germinal centers or germinal centres (GCs) are transiently formed structures within B cell zone (follicles) in secondary lymphoid organs – lymph nodes, ileal Peyer's patches, and the spleen – where mature B cells are activated, prolifera ...
s of secondary lymph nodes – express CD68
CD68 ( Cluster of Differentiation 68) is a protein highly expressed by cells in the monocyte lineage (e.g., monocytic phagocytes, osteoclasts), by circulating macrophages, and by tissue macrophages (e.g., Kupffer cells, microglia).
Structure a ...
protein. These cells normally engulf B cells that have undergone apoptosis after somatic hypermutation. In some people with SLE, significantly fewer TBMs can be found, and these cells rarely contain material from apoptotic B cells. Also, uningested apoptotic nuclei can be found outside of TBMs. This material may present a threat to the tolerization of B cells and T cells. Dendritic cells in the germinal center may endocytose such antigenic material and present it to T cells, activating them. Also, apoptotic chromatin and nuclei may attach to the surfaces of follicular dendritic cells and make this material available for activating other B cells that may have randomly acquired self-protein Self-protein refers to all proteins endogenously produced by DNA-level transcription and translation within an organism of interest. This does not include proteins synthesized due to viral infection, but may include those synthesized by commensal ...
specificity through somatic hypermutation. Necrosis, a pro-inflammatory form of cell death, is increased in T lymphocytes, due to mitochondrial dysfunction, oxidative stress, and depletion of ATP.
Clearance deficiency
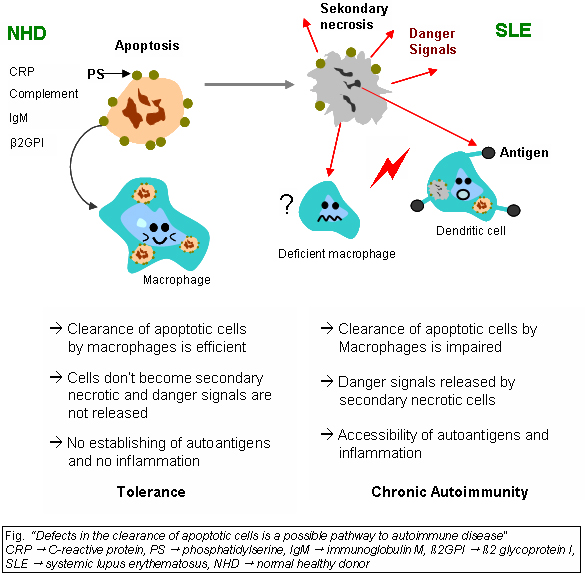 Impaired clearance of dying cells is a potential pathway for the development of this systemic autoimmune disease. This includes deficient phagocytic activity, impaired lysosomal degradation, and scant serum components in addition to increased apoptosis.
SLE is associated with defects in apoptosis, apoptotic clearance, and the damaging effects caused by apoptotic debris. Early apoptotic cells express “eat-me” signals, of cell-surface proteins such as phosphatidylserine, that prompt immune cells to engulf them. Apoptotic cells also express find-me signals to attract macrophages and dendritic cells. When apoptotic material is not removed correctly by phagocytes, they are captured instead by antigen-presenting cells, which leads to the development of antinuclear antibodies.
Impaired clearance of dying cells is a potential pathway for the development of this systemic autoimmune disease. This includes deficient phagocytic activity, impaired lysosomal degradation, and scant serum components in addition to increased apoptosis.
SLE is associated with defects in apoptosis, apoptotic clearance, and the damaging effects caused by apoptotic debris. Early apoptotic cells express “eat-me” signals, of cell-surface proteins such as phosphatidylserine, that prompt immune cells to engulf them. Apoptotic cells also express find-me signals to attract macrophages and dendritic cells. When apoptotic material is not removed correctly by phagocytes, they are captured instead by antigen-presenting cells, which leads to the development of antinuclear antibodies.[
Monocytes isolated from whole blood of people with SLE show reduced expression of CD44 surface molecules involved in the uptake of apoptotic cells. Most of the monocytes and tingible body macrophages (TBMs), which are found in the germinal centres of lymph nodes, even show a definitely different morphology; they are smaller or scarce and die earlier. Serum components like Complement system, complement factors, C-reactive protein, CRP, and some glycoproteins are, furthermore, decisively important for an efficiently operating phagocytosis. With SLE, these components are often missing, diminished, or inefficient.
Macrophages during SLE fail to mature their lysosomes and as a result have impaired degradation of internalized apoptotic debris, which results in chronic activation of Toll-like receptors and permeabilization of the phagolysosomal membrane, allowing activation of cytosolic sensors. In addition, intact apoptotic debris recycles back to the cell membrane and accumulate on the surface of the cell.
Recent research has found an association between certain people with lupus (especially those with ]lupus nephritis
Lupus nephritis is an inflammation of the kidneys caused by systemic lupus erythematosus (SLE), an autoimmune disease. It is a type of glomerulonephritis in which the glomeruli become inflamed. Since it is a result of SLE, this type of glomerulo ...
) and an impairment in degrading neutrophil extracellular traps (NETs). These were due to Deoxyribonuclease I, DNAse1 inhibiting factors, or NET protecting factors in people's serum, rather than abnormalities in the DNAse1 itself. DNAse1 mutations in lupus have so far only been found in some Japanese cohorts.
The clearance of early apoptotic cells is an important function in multicellular organisms. It leads to a progression of the apoptosis process and finally to secondary necrosis of the cells if this ability is disturbed. Necrotic cells release nuclear fragments as potential autoantigens, as well as internal danger signals, inducing maturation of dendritic cells (DCs) since they have lost their membranes' integrity. Increased appearance of apoptotic cells also stimulates inefficient clearance. That leads to the maturation of DCs and also to the presentation of intracellular antigens of late apoptotic or secondary necrotic cells, via MHC molecules.T cell
A T cell is a type of lymphocyte. T cells are one of the important white blood cells of the immune system and play a central role in the adaptive immune response. T cells can be distinguished from other lymphocytes by the presence of a T-cell r ...
tolerance for apoptotic cells is abrogated, and the lymphocytes get activated by these autoantigens; inflammation
Inflammation (from la, inflammatio) is part of the complex biological response of body tissues to harmful stimuli, such as pathogens, damaged cells, or irritants, and is a protective response involving immune cells, blood vessels, and molec ...
and the production of autoantibodies by plasma cells is initiated. A clearance deficiency in the skin for apoptotic cells has also been observed in people with cutaneous lupus erythematosus (CLE).
Germinal centers
 In healthy conditions, apoptotic lymphocytes are removed in
In healthy conditions, apoptotic lymphocytes are removed in germinal center
Germinal centers or germinal centres (GCs) are transiently formed structures within B cell zone (follicles) in secondary lymphoid organs – lymph nodes, ileal Peyer's patches, and the spleen – where mature B cells are activated, prolifera ...
s (GC) by specialized phagocytes, the tingible body macrophages (TBM), which is why no free apoptotic and potential autoantigenic material can be seen. In some people with SLE, a buildup of apoptotic debris can be observed in GC because of an ineffective clearance of apoptotic cells. Close to TBM, follicular dendritic cells (FDC) are localised in GC, which attach antigen material to their surface and, in contrast to bone marrow-derived DC, neither take it up nor present it via Major histocompatibility complex, MHC molecules.
Autoreactive B cells can accidentally emerge during somatic hypermutation and migrate into the germinal center light zone. Autoreactive B cells, maturated coincidentally, normally do not receive survival signals by antigen planted on follicular dendritic cells and perish by apoptosis. In the case of clearance deficiency, apoptotic nuclear debris accumulates in the light zone of GC and gets attached to FDC.
This serves as a germinal centre survival signal for autoreactive B-cells. After migration into the mantle zone, autoreactive B cells require further survival signals from autoreactive helper T cells, which promote the maturation of autoantibody-producing plasma cells and B memory cells. In the presence of autoreactive T cells, a chronic autoimmune disease may be the consequence.
Anti-nRNP autoimmunity
Anti-nRNP autoantibodies to nRNP A and nRNP C initially targeted restricted, proline-rich sequence motif, motifs. Antibody binding subsequently spread to other epitopes. The similarity and cross-reactivity between the initial targets of nRNP and Sm protein, Sm autoantibodies identifies a likely commonality in cause and a focal point for intermolecular epitope spreading.
Others
Elevated expression of HMGB1 was found in the sera of people and mice with systemic lupus erythematosus, high mobility group box 1 (HMGB1) is a Cell nucleus, nuclear protein participating in chromatin architecture and Transcription (genetics), transcriptional regulation. Recently, there is increasing evidence HMGB1 contributes to the pathogenesis of chronic (medicine), chronic Inflammation, inflammatory and autoimmune diseases due to its inflammatory and adjuvant, immune stimulating properties.
Diagnosis

Laboratory tests
Antinuclear antibody (ANA) testing and anti-extractable nuclear antigen (anti-ENA) form the mainstay of Serology, serologic testing for SLE. If ANA is negative the disease can be ruled out.
Several techniques are used to detect ANAs. The most widely used is indirect immunofluorescence (IF). The pattern of fluorescence suggests the type of antibody present in the people's serum. Direct immunofluorescence can detect deposits of immunoglobulins and complement proteins in people's skin. When skin not exposed to the sun is tested, a positive direct IF (the so-called lupus band test) is evidence of systemic lupus erythematosus.
ANA screening yields positive results in many connective tissue disorders and other autoimmune diseases, and may occur in normal individuals. Subtypes of antinuclear antibodies include LSm, anti-Smith and anti-double stranded DNA (dsDNA) antibodies (which are linked to SLE) and anti-histone antibodies (which are linked to drug-induced lupus). Anti-dsDNA antibodies are highly specific for SLE; they are present in 70% of cases, whereas they appear in only 0.5% of people without SLE.titer
Titer (American English) or titre (British English) is a way of expressing concentration. Titer testing employs serial dilution to obtain approximate quantitative information from an analytical procedure that inherently only evaluates as positiv ...
s also tend to reflect disease activity, although not in all cases.lupus erythematosus
Lupus erythematosus is a collection of autoimmune diseases in which the human immune system becomes hyperactive and attacks healthy tissues. Symptoms of these diseases can affect many different body systems, including joints, skin, kidneys, blo ...
(LE) cell test was commonly used for diagnosis, but it is no longer used because the LE cells are only found in 50–75% of SLE cases and they are also found in some people with rheumatoid arthritis, scleroderma, and drug sensitivities. Because of this, the LE cell test is now performed only rarely and is mostly of historical significance.
Diagnostic criteria
Some physicians make a diagnosis based on the American College of Rheumatology The American College of Rheumatology (ACR; until 1985 called American Rheumatism Association) is an organization of and for physicians, health professionals, and scientists that advances rheumatology through programs of education, research, advocacy ...
(ACR) classification criteria. However, these criteria were primarily established for use in scientific research, including selection for randomized controlled trials, which require higher confidence levels. As a result, many people with SLE may not meet the full ACR criteria.
Criteria
The American College of Rheumatology (ACR) established eleven criteria in 1982, which were revised in 1997 as a classificatory instrument to operationalise the definition of SLE in clinical trials. They were not intended to be used to diagnose individuals and do not do well in that capacity. For the purpose of identifying people for clinical studies, a person has SLE if any 4 out of 11 symptoms are present simultaneously or serially on two separate occasions.
# Malar rash (rash on cheeks); Sensitivity and specificity, sensitivity = 57%; Sensitivity and specificity, specificity = 96%.leukopenia
Leukopenia () is a decrease in the number of leukocytes (WBC). Found in the blood, they are the white blood cells, and are the body's primary defense against an infection. Thus the condition of leukopenia places individuals at increased risk of in ...
(white blood cell count<4000/µl), lymphopenia (<1500/µl), or thrombocytopenia, low platelet count (<100000/µl) in the absence of offending drug; sensitivity = 59%; specificity = 89%.psychosis
Psychosis is a condition of the mind that results in difficulties determining what is real and what is not real. Symptoms may include delusions and hallucinations, among other features. Additional symptoms are incoherent speech and behavior ...
; sensitivity = 20%; specificity = 98%.Raynaud's phenomenon
Raynaud syndrome, also known as Raynaud's phenomenon, eponymously named after the physician Auguste Gabriel Maurice Raynaud, who first described it in his doctoral thesis in 1862, is a medical condition in which the spasm of small arteries cau ...
)
Criteria for individual diagnosis
Some people, especially those with antiphospholipid syndrome, may have SLE without four of the above criteria, and also SLE may present with features other than those listed in the criteria.
Treatment
The treatment of SLE involves preventing flares and reducing their severity and duration when they occur.
Treatment can include corticosteroids and anti-malarial drugs. Certain types of lupus nephritis such as diffuse proliferative glomerulonephritis require intermittent cytotoxic drugs. These drugs include cyclophosphamide and mycophenolate. Cyclophosphamide increases the risk of developing infections, pancreas problems, high blood sugar, and high blood pressure.
Hydroxychloroquine was approved by the Food and Drug Administration, FDA for lupus in 1955.[ Some drugs approved for other diseases are used for SLE 'off-label'. In November 2010, an FDA advisory panel recommended approving belimumab (Benlysta) as a treatment for the pain and flare-ups common in lupus. The drug was approved by the FDA in March 2011.]
Medications
Due to the variety of symptoms and organ system involvement with SLE, its severity in an individual must be assessed to successfully treat SLE. Mild or remittent disease may, sometimes, be safely left untreated. If required, nonsteroidal anti-inflammatory drugs and malaria, antimalarials may be used. Medications such as prednisone, mycophenolic acid and tacrolimus have been used in the past.
Disease-modifying antirheumatic drugs
Disease-modifying antirheumatic drugs (DMARDs) are used preventively to reduce the incidence of flares, the progress of the disease, and the need for steroid use; when flares occur, they are treated with corticosteroids. DMARDs commonly in use are antimalarials such as hydroxychloroquine
Hydroxychloroquine, sold under the brand name Plaquenil among others, is a medication used to prevent and treat malaria in areas where malaria remains sensitive to chloroquine. Other uses include treatment of rheumatoid arthritis, lupus, an ...
and immunosuppressants (e.g. methotrexate and azathioprine). Hydroxychloroquine is an FDA-approved antimalarial used for constitutional, cutaneous, and articular manifestations. Hydroxychloroquine has relatively few side effects, and there is evidence that it improves survival among people who have SLE.glomerulonephritis
Glomerulonephritis (GN) is a term used to refer to several kidney diseases (usually affecting both kidneys). Many of the diseases are characterised by inflammation either of the glomeruli or of the small blood vessels in the kidneys, hence the ...
or other organ-damaging complications. Mycophenolic acid is also used for the treatment of lupus nephritis, but it is not FDA-approved for this indication, and FDA is investigating reports that it may be associated with birth defects when used by pregnant women.
Immunosuppressive drugs
In more severe cases, medications that modulate the immune system (primarily corticosteroids and immunosuppressants
Immunosuppressive drugs, also known as immunosuppressive agents, immunosuppressants and antirejection medications, are drugs that inhibit or prevent activity of the immune system.
Classification
Immunosuppressive drugs can be classified int ...
) are used to control the disease and prevent recurrence of symptoms (known as flares). Depending on the dosage, people who require steroids may develop Cushing's syndrome, symptoms of which may include obesity, puffy round face, diabetes mellitus, increased appetite, difficulty sleeping, and osteoporosis. These may subside if and when the large initial dosage is reduced, but long-term use of even low doses can cause elevated blood pressure and cataracts.
Numerous new immunosuppressive drugs are being actively tested for SLE. Rather than broadly suppressing the immune system, as corticosteroids do, they target the responses of specific types of immune cells. Some of these drugs are already FDA-approved for treatment of rheumatoid arthritis
Rheumatoid arthritis (RA) is a long-term autoimmune disorder that primarily affects joints. It typically results in warm, swollen, and painful joints. Pain and stiffness often worsen following rest. Most commonly, the wrist and hands are invol ...
, however due to high-toxicity, their use remains limited.[
]
Analgesia
Since a large percentage of people with SLE have varying amounts of chronic pain, stronger prescription analgesics (painkillers) may be used if over-the-counter drugs (mainly nonsteroidal anti-inflammatory drugs) do not provide effective relief. Potent NSAIDs such as indomethacin and diclofenac are relatively contraindicated for people with SLE because they increase the risk of kidney failure and heart failure.[
Pain is typically treated with opioids, varying in potency based on the severity of symptoms. When opioids are used for prolonged periods, drug tolerance, chemical dependency, and addiction may occur. Opiate addiction is not typically a concern since the condition is not likely to ever completely disappear. Thus, lifelong treatment with opioids is fairly common for chronic pain symptoms, accompanied by periodic titration that is typical of any long-term opioid regimen.
]
Intravenous immunoglobulins (IVIGs)
Intravenous immunoglobulins may be used to control SLE with organ involvement, or vasculitis. It is believed that they reduce antibody production or promote the clearance of immune complexes from the body, even though their mechanism of action is not well understood. Unlike immunosuppressives and corticosteroids, IVIGs do not suppress the immune system
The immune system is a network of biological processes that protects an organism from diseases. It detects and responds to a wide variety of pathogens, from viruses to parasitic worms, as well as cancer cells and objects such as wood splint ...
, so there is less risk of serious infections with these drugs.
Lifestyle changes
Avoiding sunlight in SLE is critical since sunlight is known to exacerbate skin manifestations of the disease. Avoiding activities that induce fatigue is also important since those with SLE fatigue easily and it can be debilitating. These two problems can lead to people becoming housebound for long periods of time. Drugs unrelated to SLE should be prescribed only when known not to exacerbate the disease. Occupational exposure to silica, pesticides, and mercury (element), mercury can also worsen the disease.
Kidney transplantation
Kidney transplants are the treatment of choice for end-stage renal disease, end-stage kidney disease, which is one of the complications of lupus nephritis
Lupus nephritis is an inflammation of the kidneys caused by systemic lupus erythematosus (SLE), an autoimmune disease. It is a type of glomerulonephritis in which the glomeruli become inflamed. Since it is a result of SLE, this type of glomerulo ...
, but the recurrence of the full disease is common in up to 30% of people.
Antiphospholipid syndrome
Approximately 20% of people with SLE have clinically significant levels of antiphospholipid antibodies, which are associated with antiphospholipid syndrome. Antiphospholipid syndrome is also related to the onset of neural lupus symptoms in the brain. In this form of the disease, the cause is very different from lupus: thromboses (blood clots or "sticky blood") form in blood vessels, which prove to be fatal if they move within the bloodstream.
Management of pregnancy
While most infants born to mothers who have SLE are healthy, pregnant mothers with SLE should remain under medical care until delivery. Neonatal lupus
Neonatal lupus erythematosus is an autoimmune disease in an infant born to a mother with anti-Ro/SSA and with or without anti-La/SSB antibodies. The disease most commonly presents with a rash resembling subacute cutaneous lupus erythematosus and ...
is rare, but identification of mothers at the highest risk for complications allows for prompt treatment before or after birth. In addition, SLE can flare up during pregnancy, and proper treatment can maintain the health of the mother longer. Women pregnant and known to have Anti-Ro antibodies, anti-Ro (SSA) or anti-La antibodies (SSB) often have echocardiograms during the 16th and 30th weeks of pregnancy to monitor the health of the heart and surrounding vasculature.
Prognosis
No cure is available for SLE but there are many treatments for the disease.[
In the 1950s, most people diagnosed with SLE lived fewer than five years. Today, over 90% now survive for more than ten years, and many live relatively symptom-free. 80–90% can expect to live a normal lifespan.][ To reduce the potential for cardiovascular issues, high blood pressure and high cholesterol should be prevented or treated aggressively. Steroids should be used at the lowest dose for the shortest possible period, and other drugs that can reduce symptoms should be used whenever possible.][
]
Epidemiology
The global rates of SLE are approximately 20–70 per 100,000 people. In females, the rate is highest between 45 and 64 years of age. The lowest overall rate exists in Iceland and Japan. The highest rates exist in the US and France. However, there is not sufficient evidence to conclude why SLE is less common in some countries compared to others; it could be the environmental variability in these countries. For example, different countries receive different levels of sunlight, and exposure to UV rays affects dermatological symptoms of SLE.[
Certain studies hypothesize that a genetic connection exists between race and lupus which affects disease prevalence. If this is true, the racial composition of countries affects disease and will cause the incidence in a country to change as the racial makeup changes. To understand if this is true, countries with largely homogenous and racially stable populations should be studied to better understand incidence.][ Rates of disease in the developing world are unclear.][
The rate of SLE varies between countries, ethnicity, and sex, and changes over time.][ another estimate places the total affected population at 322,000 to over 1 million (98 to over 305 per 100,000).][ In Northern Europe the rate is about 40 per 100,000 people.][ Childhood-onset systemic lupus erythematosus generally presents between the ages of 3 and 15 and is four times more common in girls.
While the onset and persistence of SLE can show disparities between genders, socioeconomic status also plays a major role. Women with SLE and of lower socioeconomic status have been shown to have higher depression scores, higher body mass index, and more restricted access to medical care than women of higher socioeconomic statuses with the illness. People with SLE had more self-reported anxiety and depression scores if they were from a lower socioeconomic status.
]
Ethnicity
There are assertions that race affects the rate of SLE. However, a 2010 review of studies that correlate race and SLE identified several sources of systematic and methodological error, indicating that the connection between race and SLE may be spurious.[ Studies have not been conducted to determine whether people of different racial backgrounds receive differing levels of social support.][
If there is a difference, this could act as a confounding variable in studies correlating race and SLE. Another caveat to note when examining studies about SLE is that symptoms are often self-reported. This process introduces additional sources of methodological error. Studies have shown that self-reported data is affected by more than just the patient's experience with the disease- social support, the level of helplessness, and abnormal illness-related behaviors also factor into a self-assessment. Additionally, other factors like the degree of social support that a person receives, socioeconomic status, health insurance, and access to care can contribute to an individual's disease progression.][
Racial differences in lupus progression have not been found in studies that control for the socioeconomic status [SES] of participants.][ The people who receive medical care have often accrued less disease-related damage and are less likely to be below the poverty line.][
]
Sex
SLE, like many autoimmune diseases, affects females more frequently than males, at a rate of about 9 to 1.[ The X chromosome carries immunological related genes, which can mutate and contribute to the onset of SLE. The Y chromosome has no identified mutations associated with autoimmune disease.]
Changing rate of disease
The rate of SLE in the United States increased from 1.0 in 1955 to 7.6 in 1974. Whether the increase is due to better diagnosis or an increased frequency of the disease is unknown.[
]
History
The history of SLE can be divided into three periods: classical, neoclassical, and modern. In each period, research and documentation advanced the understanding and diagnosis of SLE, leading to its classification as an autoimmune disease in 1851, and to the various diagnostic options and treatments now available to people with SLE. The advances made by medical science in the diagnosis and treatment of SLE have dramatically improved the life expectancy of a person diagnosed with SLE.
Etymology
There are several explanations ventured for the term lupus erythematosus. Lupus is Latin for "wolf",[ and "erythro" is derived from , Greek for "red". All explanations originate with the reddish, butterfly-shaped malar rash that the disease classically exhibits across the nose and cheeks. The reason the term lupus was used to describe this disease comes from the mid-19th century. Many diseases that caused ulceration or necrosis were given the term "lupus" due to the wound being reminiscent of a wolf's bite. This is similar to the naming of lupus vulgaris or chronic facial tuberculosis, where the lesions are ragged and punched out and are said to resemble the bite of a wolf.
]
Classical period
The classical period began when the disease was first recognized in the Middle Ages. The term lupus is attributed to 12th-century Italian physician Rogerius (physician), Rogerius Frugard, who used it to describe ulcerating sores on the legs of people.
Neoclassical period
The neoclassical period began in 1851 when the skin disease which is now known as discoid lupus was documented by the French physician, Pierre Louis Alphée Cazenave, Pierre Cazenave. Cazenave termed the illness lupus and added the word erythematosus to distinguish this disease from other illnesses that affected the skin except they were infectious.
Modern period
The modern period, beginning in 1920, saw major developments in research into the cause and treatment of discoid and systemic lupus. Research conducted in the 1920s and 1930s led to the first detailed pathologic descriptions of lupus and demonstrated how the disease affected the kidney, heart, and lung tissue.
Research
A study called BLISS-76 tested the drug belimumab, a fully human monoclonal antibody, monoclonal anti-B-cell activating factor, BAFF (or anti-BLyS) antibody.self-protein Self-protein refers to all proteins endogenously produced by DNA-level transcription and translation within an organism of interest. This does not include proteins synthesized due to viral infection, but may include those synthesized by commensal ...
. It was approved by the FDA in March 2011.[ Genetically engineered immune cells are also being studied in animal models of the disease as of 2019.
In September 2022, researchers at the University of Erlangen–Nuremberg, University of Erlangen-Nuremberg published promising results using genetically altered immune cells to treat severely ill patients. Four women and one man received transfusions of CAR T cell, CAR T cells modified to attack their B cell, B cells, eliminating the aberrant ones. The therapy drove the disease into remission in all five patients, who have been off lupus medication for several months after the treatment ended.]
See also
* Canine discoid lupus erythematosus in dogs
* List of people with lupus
References
External links
*
Systemic Lupus Erythematosus
at the National Institute of Arthritis and Musculoskeletal and Skin Diseases
{{Autoimmune diseases
Autoimmune diseases
Cutaneous lupus erythematosus
Disorders causing seizures
Disorders of fascia
Epstein–Barr virus–associated diseases
Steroid-responsive inflammatory conditions
Systemic connective tissue disorders
Wikipedia medicine articles ready to translate
William Osler
 SLE is one of several diseases known as "
SLE is one of several diseases known as "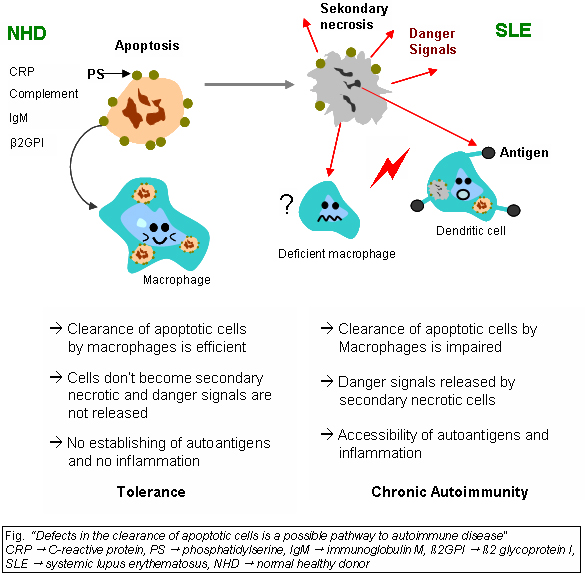 Impaired clearance of dying cells is a potential pathway for the development of this systemic autoimmune disease. This includes deficient phagocytic activity, impaired lysosomal degradation, and scant serum components in addition to increased apoptosis.
SLE is associated with defects in apoptosis, apoptotic clearance, and the damaging effects caused by apoptotic debris. Early apoptotic cells express “eat-me” signals, of cell-surface proteins such as phosphatidylserine, that prompt immune cells to engulf them. Apoptotic cells also express find-me signals to attract macrophages and dendritic cells. When apoptotic material is not removed correctly by phagocytes, they are captured instead by antigen-presenting cells, which leads to the development of antinuclear antibodies.
Monocytes isolated from whole blood of people with SLE show reduced expression of CD44 surface molecules involved in the uptake of apoptotic cells. Most of the monocytes and tingible body macrophages (TBMs), which are found in the germinal centres of lymph nodes, even show a definitely different morphology; they are smaller or scarce and die earlier. Serum components like Complement system, complement factors, C-reactive protein, CRP, and some glycoproteins are, furthermore, decisively important for an efficiently operating phagocytosis. With SLE, these components are often missing, diminished, or inefficient.
Macrophages during SLE fail to mature their lysosomes and as a result have impaired degradation of internalized apoptotic debris, which results in chronic activation of Toll-like receptors and permeabilization of the phagolysosomal membrane, allowing activation of cytosolic sensors. In addition, intact apoptotic debris recycles back to the cell membrane and accumulate on the surface of the cell.
Recent research has found an association between certain people with lupus (especially those with
Impaired clearance of dying cells is a potential pathway for the development of this systemic autoimmune disease. This includes deficient phagocytic activity, impaired lysosomal degradation, and scant serum components in addition to increased apoptosis.
SLE is associated with defects in apoptosis, apoptotic clearance, and the damaging effects caused by apoptotic debris. Early apoptotic cells express “eat-me” signals, of cell-surface proteins such as phosphatidylserine, that prompt immune cells to engulf them. Apoptotic cells also express find-me signals to attract macrophages and dendritic cells. When apoptotic material is not removed correctly by phagocytes, they are captured instead by antigen-presenting cells, which leads to the development of antinuclear antibodies.
Monocytes isolated from whole blood of people with SLE show reduced expression of CD44 surface molecules involved in the uptake of apoptotic cells. Most of the monocytes and tingible body macrophages (TBMs), which are found in the germinal centres of lymph nodes, even show a definitely different morphology; they are smaller or scarce and die earlier. Serum components like Complement system, complement factors, C-reactive protein, CRP, and some glycoproteins are, furthermore, decisively important for an efficiently operating phagocytosis. With SLE, these components are often missing, diminished, or inefficient.
Macrophages during SLE fail to mature their lysosomes and as a result have impaired degradation of internalized apoptotic debris, which results in chronic activation of Toll-like receptors and permeabilization of the phagolysosomal membrane, allowing activation of cytosolic sensors. In addition, intact apoptotic debris recycles back to the cell membrane and accumulate on the surface of the cell.
Recent research has found an association between certain people with lupus (especially those with  In healthy conditions, apoptotic lymphocytes are removed in
In healthy conditions, apoptotic lymphocytes are removed in 