|
Ventilator-associated Lung Injury
Ventilator-associated lung injury (VALI) is an acute lung injury that develops during mechanical ventilation and is termed ventilator-induced lung injury (VILI) if it can be proven that the mechanical ventilation caused the acute lung injury. In contrast, ventilator-associated lung injury (VALI) exists if the cause cannot be proven. VALI is the appropriate term in most situations because it is virtually impossible to prove what actually caused the lung injury in the hospital. Cause It is generally regarded, based on animal models and human studies, that volutrauma is the most harmful aspect of mechanical ventilation. This may be regarded as the over-stretching of the airways and alveoli. During mechanical ventilation, the flow of gas into the lung will take the path of least resistance. Areas of the lung that are collapsed (atelectasis) or filled with secretions will be underinflated, while those areas that are relatively normal will be overinflated. These areas will become over ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |
Mechanical Ventilation
Mechanical ventilation, assisted ventilation or intermittent mandatory ventilation (IMV), is the medical term for using a machine called a ventilator to fully or partially provide artificial ventilation. Mechanical ventilation helps move air into and out of the lungs, with the main goal of helping the delivery of oxygen and removal of carbon dioxide. Mechanical ventilation is used for many reasons, including to protect the airway due to mechanical or neurologic cause, to ensure adequate oxygenation, or to remove excess carbon dioxide from the lungs. Various healthcare providers are involved with the use of mechanical ventilation and people who require ventilators are typically monitored in an intensive care unit. Mechanical ventilation is termed invasive if it involves an instrument to create an airway that is placed inside the trachea. This is done through an endotracheal tube or nasotracheal tube. For non-invasive ventilation in people who are conscious, face or nasal ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |
Positive End-expiratory Pressure
Positive end-expiratory pressure (PEEP) is the pressure in the lungs (alveolar pressure) above atmospheric pressure (the pressure outside of the body) that exists at the end of expiration. The two types of PEEP are extrinsic PEEP (PEEP applied by a ventilator) and intrinsic PEEP (PEEP caused by an incomplete exhalation). Pressure that is applied or increased during an inspiration is termed pressure support. Intrinsic (auto-) PEEP Auto-PEEP is an incomplete expiration prior to the initiation of the next breath causes progressive air trapping ( hyperinflation). This accumulation of air increases alveolar pressure at the end of expiration, which is referred to as auto-PEEP. Auto-PEEP develops commonly in high minute ventilation (hyperventilation), expiratory flow limitation (obstructed airway) and expiratory resistance (narrow airway). Once auto-PEEP is identified, steps should be taken to stop or reduce the pressure build-up. When auto-PEEP persists despite management of its ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |
Medical Equipment
A medical device is any device intended to be used for medical purposes. Significant potential for hazards are inherent when using a device for medical purposes and thus medical devices must be proved safe and effective with reasonable assurance before regulating governments allow marketing of the device in their country. As a general rule, as the associated risk of the device increases the amount of testing required to establish safety and efficacy also increases. Further, as associated risk increases the potential benefit to the patient must also increase. Discovery of what would be considered a medical device by modern standards dates as far back as c. 7000 BC in Baluchistan where Neolithic dentists used flint-tipped drills and bowstrings. Study of archeology and Roman medical literature also indicate that many types of medical devices were in widespread use during the time of ancient Rome. In the United States it wasn't until the Federal Food, Drug, and Cosmetic Act (FD&C ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |
Emergency Medicine
Emergency medicine is the Medical specialty, medical speciality concerned with the care of illnesses or Injury, injuries requiring immediate medical attention. Emergency physicians (often called “ER doctors” in the United States) continuously learn to care for unscheduled and undifferentiated patients of all ages. As first-line providers, in coordination with Emergency Medical Services, they are primarily responsible for initiating resuscitation and stabilization and performing the initial investigations and interventions necessary to diagnose and treat illnesses or injuries in the acute phase. Emergency physicians generally practise in Hospital, hospital emergency Emergency room, departments, Pre-hospital emergency medicine, pre-hospital settings via emergency medical services, and intensive care units. Still, they may also work in primary care settings such as urgent care clinics. Sub-specializations of emergency medicine include; disaster medicine, medical toxicology, Eme ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |
Pulmonology
Pulmonology (, , from Latin ''pulmō, -ōnis'' "lung" and the Ancient Greek, Greek suffix "study of"), pneumology (, built on Greek πνεύμων "lung") or pneumonology () is a specialty (medicine), medical specialty that deals with Respiratory disease, diseases involving the respiratory tract.ACP: Pulmonology: Internal Medicine Subspecialty . Acponline.org. Retrieved on 2011-09-30. It is also known as respirology, respiratory medicine, or chest medicine in some countries and areas. Pulmonology is considered a branch of internal medicine, and is related to intensive care medicine. Pulmonology often involves managing patients who need life support and mechanical ventilation. Pulmonologists are specially trained in diseases and conditions of the chest, ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |
Respiratory Therapy
A respiratory therapist is a specialized healthcare practitioner trained in critical care and cardio-pulmonary medicine in order to work therapeutically with people who have acute critical conditions, cardiac and pulmonary disease. Respiratory therapists graduate from a college or university with a degree in respiratory therapy and have passed a national board certifying examination. The NBRC (National Board for Respiratory Care) is responsible for credentialing as a CRT ( certified respiratory therapist), or RRT ( registered respiratory therapist), The specialty certifications of respiratory therapy include: CPFT and RPFT (Certified or Registered Pulmonary Function Technologist), ACCS (Adult Critical Care Specialist), NPS (Neonatal/Pediatric Specialist), and SDS (Sleep Disorder Specialist). Respiratory therapists work in hospitals in the intensive care units (Adult, Pediatric, and Neonatal), on hospital floors, in emergency departments, in pulmonary functioning laboratories ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |
Hypoxaemia
Hypoxemia is an abnormally low level of oxygen in the blood. More specifically, it is oxygen deficiency in arterial blood. Hypoxemia has many causes, and often causes hypoxia as the blood is not supplying enough oxygen to the tissues of the body. Definition ''Hypoxemia'' refers to the low level of oxygen in blood, and the more general term ''hypoxia'' is an abnormally low oxygen content in any tissue or organ, or the body as a whole. Hypoxemia can cause hypoxia (hypoxemic hypoxia), but hypoxia can also occur via other mechanisms, such as anemia. Hypoxemia is usually defined in terms of reduced partial pressure of oxygen (mm Hg) in arterial blood, but also in terms of reduced content of oxygen (ml oxygen per dl blood) or percentage saturation of hemoglobin (the oxygen-binding protein within red blood cells) with oxygen, which is either found singly or in combination. While there is general agreement that an arterial blood gas measurement which shows that the partial pressure ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |
Permissive Hypercapnia
Permissive hypercapnia is hypercapnia (i.e. high concentration of carbon dioxide in blood) in respiratory insufficient patients in which oxygenation has become so difficult that the optimal mode of mechanical ventilation (with oxygenation in mind) is not capable of exchanging enough carbon dioxide. Carbon dioxide is a gaseous product of the body's metabolism and is normally expelled through the lungs. In acute respiratory distress syndrome (ARDS), decreasing the tidal volume on the ventilator (usually 6-8 mL/kg) to 4-6 mL/kg may decrease barotrauma by decreasing ventilatory peak airway pressures and leads to improved respiratory recovery. Hypercapnia (increased pCO2) sometimes needs to be tolerated in order to achieve these lower tidal volumes. The permissive hypercapnia leads to respiratory acidosis which might have negative side effects, but given that the patient is in ARDS, improving ventilatory function is more important. Since hypoxemia is a major life-threatening condit ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |
Acute Lung Injury
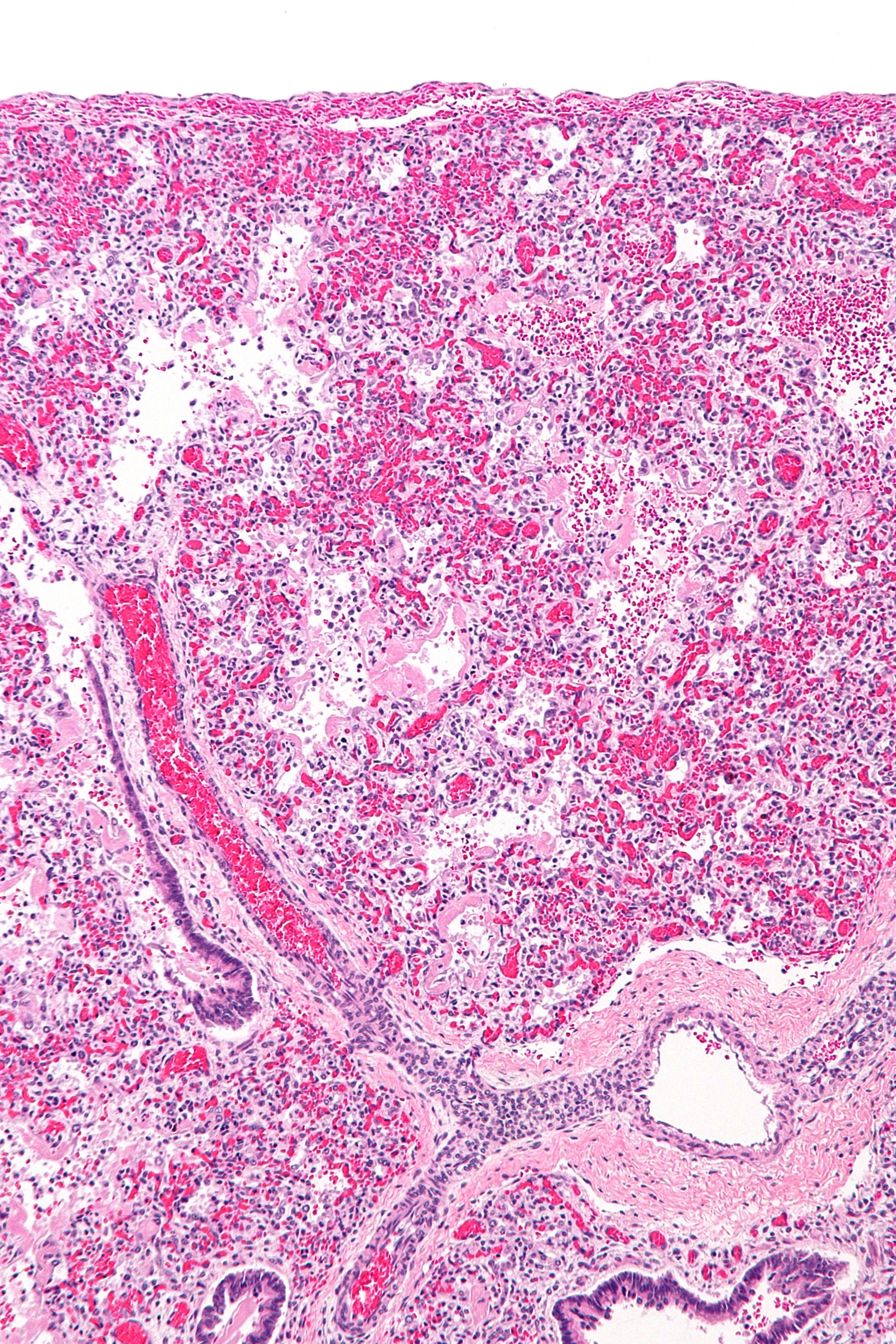
Acute respiratory distress syndrome (ARDS) is a type of respiratory failure characterized by rapid onset of widespread inflammation in the lungs. Symptoms include shortness of breath (dyspnea), rapid breathing (tachypnea), and bluish skin coloration (cyanosis). For those who survive, a decreased quality of life is common. Causes may include sepsis, pancreatitis, trauma, pneumonia, and aspiration. The underlying mechanism involves diffuse injury to cells which form the barrier of the microscopic air sacs of the lungs, surfactant dysfunction, activation of the immune system, and dysfunction of the body's regulation of blood clotting. In effect, ARDS impairs the lungs' ability to exchange oxygen and carbon dioxide. Adult diagnosis is based on a PaO2/FiO2 ratio (ratio of partial pressure arterial oxygen and fraction of inspired oxygen) of less than 300 mm Hg despite a positive end-expiratory pressure (PEEP) of more than 5 cm H2O. Cardiogenic pulmonary edema, as t ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |
ARDS
Acute respiratory distress syndrome (ARDS) is a type of respiratory failure characterized by rapid onset of widespread inflammation in the lungs. Symptoms include shortness of breath (dyspnea), rapid breathing (tachypnea), and bluish skin coloration (cyanosis). For those who survive, a decreased quality of life is common. Causes may include sepsis, pancreatitis, trauma, pneumonia, and aspiration. The underlying mechanism involves diffuse injury to cells which form the barrier of the microscopic air sacs of the lungs, surfactant dysfunction, activation of the immune system, and dysfunction of the body's regulation of blood clotting. In effect, ARDS impairs the lungs' ability to exchange oxygen and carbon dioxide. Adult diagnosis is based on a PaO2/FiO2 ratio (ratio of partial pressure arterial oxygen and fraction of inspired oxygen) of less than 300 mm Hg despite a positive end-expiratory pressure (PEEP) of more than 5 cm H2O. Cardiogenic pulmonary edema, as th ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |
High Frequency Ventilation
Modes of mechanical ventilation are one of the most important aspects of the usage of mechanical ventilation. The mode refers to the method of inspiratory support. In general, mode selection is based on clinician familiarity and institutional preferences, since there is a paucity of evidence indicating that the mode affects clinical outcome. The most frequently used forms of volume-limited mechanical ventilation are intermittent mandatory ventilation (IMV) and continuous mandatory ventilation (CMV). There have been substantial changes in the nomenclature of mechanical ventilation over the years, but more recently it has become standardized by many respirology and pulmonology groups. Writing a mode is most proper in all capital letters with a dash between the control variable and the strategy (i.e. PC-IMV, or VC-MMV etc.). Taxonomy for mechanical ventilation The taxonomy is a logical classification system based on 10 maxims of ventilator design 10 maxims #A breath is one cyc ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |
The Cochrane Collaboration
Cochrane (previously known as the Cochrane Collaboration) is a British international charitable organisation formed to organise medical research findings to facilitate evidence-based choices about health interventions involving health professionals, patients and policy makers. It includes 53 review groups that are based at research institutions worldwide. Cochrane has approximately 30,000 volunteer experts from around the world. The group conducts systematic reviews of health-care interventions and diagnostic tests and publishes them in the Cochrane Library. According to the Library, articles are available via one-click access, but some require paid subscription or registration before reading. A few reviews, in occupational health for example, incorporate results from non-randomised observational studies as well as controlled before–after (CBA) studies and interrupted time-series studies. History Cochrane, previously known as the Cochrane Collaboration, was founded in ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |