Thrombosis on:
[Wikipedia]
[Google]
[Amazon]
Thrombosis (from
 A stroke is the rapid decline of brain function due to a disturbance in the supply of blood to the brain. This can be due to ischemia, thrombus,
A stroke is the rapid decline of brain function due to a disturbance in the supply of blood to the brain. This can be due to ischemia, thrombus,
This article was last reviewed on May 23, 2007 and was last modified on March 6, 2010. Inflammatory and other stimuli (such as
 Causes of disturbed blood flow include stagnation of blood flow past the point of injury, or
Causes of disturbed blood flow include stagnation of blood flow past the point of injury, or
Ancient Greek
Ancient Greek includes the forms of the Greek language used in ancient Greece and the ancient world from around 1500 BC to 300 BC. It is often roughly divided into the following periods: Mycenaean Greek (), Dark Ages (), the Archaic p ...
"clotting") is the formation of a blood clot inside a blood vessel
The blood vessels are the components of the circulatory system that transport blood throughout the human body. These vessels transport blood cells, nutrients, and oxygen to the tissues of the body. They also take waste and carbon dioxide away ...
, obstructing the flow of blood
Blood is a body fluid in the circulatory system of humans and other vertebrates that delivers necessary substances such as nutrients and oxygen to the cells, and transports metabolic waste products away from those same cells. Blood in the cir ...
through the circulatory system
The blood circulatory system is a system of organs that includes the heart, blood vessels, and blood which is circulated throughout the entire body of a human or other vertebrate. It includes the cardiovascular system, or vascular system, tha ...
. When a blood vessel (a vein
Veins are blood vessels in humans and most other animals that carry blood towards the heart. Most veins carry deoxygenated blood from the tissues back to the heart; exceptions are the pulmonary and umbilical veins, both of which carry oxygenat ...
or an artery) is injured, the body uses platelets (thrombocytes) and fibrin to form a blood clot to prevent blood loss. Even when a blood vessel is not injured, blood clots may form in the body under certain conditions. A clot, or a piece of the clot, that breaks free and begins to travel around the body is known as an embolus
An embolus (; plural emboli; from the Greek ἔμβολος "wedge", "plug") is an unattached mass that travels through the bloodstream and is capable of creating blockages. When an embolus occludes a blood vessel, it is called an embolism or emb ...
.
Thrombosis may occur in veins ( venous thrombosis) or in arteries ( arterial thrombosis). Venous thrombosis (sometimes called DVT, deep vein thrombosis) leads to a blood clot in the affected part of the body, while arterial thrombosis (and, rarely, severe venous thrombosis) affects the blood supply and leads to damage of the tissue supplied by that artery ( ischemia and necrosis). A piece of either an arterial or a venous thrombus can break off as an embolus, which could then travel through the circulation and lodge somewhere else as an embolism
An embolism is the lodging of an embolus, a blockage-causing piece of material, inside a blood vessel. The embolus may be a blood clot (thrombus), a fat globule (fat embolism), a bubble of air or other gas ( gas embolism), amniotic fluid (am ...
. This type of embolism is known as a ''thromboembolism''. Complications can arise when a venous thromboembolism (commonly called a VTE) lodges in the lung as a pulmonary embolism
Pulmonary embolism (PE) is a blockage of an artery in the lungs by a substance that has moved from elsewhere in the body through the bloodstream ( embolism). Symptoms of a PE may include shortness of breath, chest pain particularly upon breathin ...
. An arterial embolus may travel further down the affected blood vessel, where it can lodge as an embolism.
Signs and symptoms
Thrombosis is generally defined by the type of blood vessel affected (arterial or venous thrombosis) and the precise location of the blood vessel or the organ supplied by it.Venous thrombosis
Deep vein thrombosis
Deep vein thrombosis (DVT) is the formation of a blood clot within a deep vein. It most commonly affects leg veins, such as thefemoral vein
In the human body, the femoral vein is a blood vessel that accompanies the femoral artery in the femoral sheath. It begins at the adductor hiatus (an opening in the adductor magnus muscle) as the continuation of the popliteal vein. It ends a ...
. Three factors are important in the formation of a blood clot within a deep vein—these are the rate of blood flow, the thickness of the blood and qualities of the vessel wall. Classical signs of DVT include swelling, pain and redness of the affected area.
Paget-Schroetter disease
Paget-Schroetter disease or upper extremity DVT (UEDVT) is the obstruction of anarm
In human anatomy, the arm refers to the upper limb in common usage, although academically the term specifically means the upper arm between the glenohumeral joint (shoulder joint) and the elbow joint. The distal part of the upper limb between th ...
vein (such as the axillary vein
In human anatomy, the axillary vein is a large blood vessel that conveys blood from the lateral aspect of the thorax, axilla (armpit) and upper limb toward the heart. There is one axillary vein on each side of the body.
Structure
Its origin ...
or subclavian vein) by a thrombus. The condition usually comes to light after vigorous exercise and usually presents in younger, otherwise healthy people. Men are affected more than women.
Budd-Chiari syndrome
Budd-Chiari syndrome is the blockage of a hepatic vein or of the hepatic part of theinferior vena cava
The inferior vena cava is a large vein that carries the deoxygenated blood from the lower and middle body into the right atrium of the heart. It is formed by the joining of the right and the left common iliac veins, usually at the level of th ...
. This form of thrombosis presents with abdominal pain, ascites
Ascites is the abnormal build-up of fluid in the abdomen. Technically, it is more than 25 ml of fluid in the peritoneal cavity, although volumes greater than one liter may occur. Symptoms may include increased abdominal size, increased weight, a ...
and enlarged liver. Treatment varies between therapy and surgical intervention by the use of shunts.
Portal vein thrombosis
Portal vein thrombosis affects the hepatic portal vein, which can lead to portal hypertension and reduction of the blood supply to the liver. It usually happens in the setting of another disease such as pancreatitis,cirrhosis
Cirrhosis, also known as liver cirrhosis or hepatic cirrhosis, and end-stage liver disease, is the impaired liver function caused by the formation of scar tissue known as fibrosis due to damage caused by liver disease. Damage causes tissue rep ...
, diverticulitis or cholangiocarcinoma.
Renal vein thrombosis
Renal vein thrombosis is the obstruction of therenal vein
The renal veins are large-calibre veins that drain blood filtered by the kidneys into the inferior vena cava. There is one renal vein draining each kidney.
Because the inferior vena cava is on the right half of the body, the left renal vein is lo ...
by a thrombus. This tends to lead to reduced drainage from the kidney.
Cerebral venous sinus thrombosis
Cerebral venous sinus thrombosis (CVST) is a rare form of stroke which results from the blockage of the dural venous sinuses by a thrombus. Symptoms may include headache, abnormal vision, any of the symptoms of stroke such as weakness of the face and limbs on one side of the body andseizures
An epileptic seizure, informally known as a seizure, is a period of symptoms due to abnormally excessive or synchronous neuronal activity in the brain. Outward effects vary from uncontrolled shaking movements involving much of the body with l ...
. The diagnosis is usually made with a CT or MRI scan
Magnetic resonance imaging (MRI) is a medical imaging technique used in radiology to form pictures of the anatomy and the physiological processes of the body. MRI scanners use strong magnetic fields, magnetic field gradients, and radio waves ...
. The majority of persons affected make a full recovery. The mortality rate
Mortality rate, or death rate, is a measure of the number of deaths (in general, or due to a specific cause) in a particular population, scaled to the size of that population, per unit of time. Mortality rate is typically expressed in units of d ...
is 4.3%.
Jugular vein thrombosis
Jugular vein thrombosis is a condition that may occur due to infection, intravenous drug use or malignancy. Jugular vein thrombosis can have a varying list of complications, including: systemic sepsis,pulmonary embolism
Pulmonary embolism (PE) is a blockage of an artery in the lungs by a substance that has moved from elsewhere in the body through the bloodstream ( embolism). Symptoms of a PE may include shortness of breath, chest pain particularly upon breathin ...
, and papilledema
Papilledema or papilloedema is optic disc swelling that is caused by increased intracranial pressure due to any cause. The swelling is usually bilateral and can occur over a period of hours to weeks. Unilateral presentation is extremely rare.
In ...
. Though characterized by a sharp pain at the site of the vein, it can prove difficult to diagnose, because it can occur at random.
Cavernous sinus thrombosis
Cavernous sinus thrombosis is a specialised form of cerebral venous sinus thrombosis, where there is thrombosis of thecavernous sinus
The cavernous sinus within the human head is one of the dural venous sinuses creating a cavity called the lateral sellar compartment bordered by the temporal bone of the skull and the sphenoid bone, lateral to the sella turcica.
Structure
The cave ...
of the basal skull dura, due to the retrograde spread of infection and endothelial damage from the danger triangle of the face. The facial veins in this area anastomose with the superior and inferior ophthalmic veins of the orbit, which drain directly posteriorly into the cavernous sinus through the superior orbital fissure. Staphyloccoal or Streptococcal infections of the face, for example nasal or upper lip pustules may thus spread directly into the cavernous sinus, causing stroke-like symptoms of double vision
Diplopia is the simultaneous perception of two images of a single object that may be displaced horizontally or vertically in relation to each other. Also called double vision, it is a loss of visual focus under regular conditions, and is often v ...
, squint, as well as spread of infection to cause meningitis.
Arterial thrombosis
Arterial thrombosis is the formation of a thrombus within an artery. In most cases, arterial thrombosis follows rupture ofatheroma
An atheroma, or atheromatous plaque, is an abnormal and reversible accumulation of material in the inner layer of an arterial wall.
The material consists of mostly macrophage cells, or debris, containing lipids, calcium and a variable amount o ...
(a fat-rich deposit in the blood vessel wall), and is therefore referred to as ''atherothrombosis''. Arterial embolism occurs when clots then migrate downstream and can affect any organ.Alternatively, arterial occlusion occurs as a consequence of embolism of blood clots originating from the heart ("cardiogenic" emboli). The most common cause is atrial fibrillation, which causes a blood stasis within the atria with easy thrombus formation, but blood clots can develop inside the heart for other reasons too as infective endocarditis.
Stroke
 A stroke is the rapid decline of brain function due to a disturbance in the supply of blood to the brain. This can be due to ischemia, thrombus,
A stroke is the rapid decline of brain function due to a disturbance in the supply of blood to the brain. This can be due to ischemia, thrombus, embolus
An embolus (; plural emboli; from the Greek ἔμβολος "wedge", "plug") is an unattached mass that travels through the bloodstream and is capable of creating blockages. When an embolus occludes a blood vessel, it is called an embolism or emb ...
(a lodged particle) or hemorrhage (a bleed). In thrombotic stroke, a thrombus (blood clot) usually forms around atherosclerotic
Atherosclerosis is a pattern of the disease arteriosclerosis in which the wall of the artery develops abnormalities, called lesions. These lesions may lead to narrowing due to the buildup of atheromatous plaque. At onset there are usually no ...
plaques. Since blockage of the artery is gradual, the onset of symptomatic thrombotic strokes is slower. Thrombotic stroke can be divided into two categories — large vessel disease or small vessel disease. The former affects vessels such as the internal carotids, vertebral
The vertebral column, also known as the backbone or spine, is part of the axial skeleton. The vertebral column is the defining characteristic of a vertebrate in which the notochord (a flexible rod of uniform composition) found in all chordates ...
and the circle of Willis. The latter can affect smaller vessels, such as the branches of the circle of Willis.
Myocardial infarction
Myocardial infarction (MI), or heart attack, is caused by ischemia (restriction in the blood supply), which is often due to the obstruction of acoronary artery
The coronary arteries are the arterial blood vessels of coronary circulation, which transport oxygenated blood to the heart muscle. The heart requires a continuous supply of oxygen to function and survive, much like any other tissue or organ ...
by a thrombus. This restriction gives an insufficient supply of oxygen to the heart muscle which then results in tissue death (infarction). A lesion is then formed which is the infarct
Infarction is tissue death (necrosis) due to inadequate blood supply to the affected area. It may be caused by artery blockages, rupture, mechanical compression, or vasoconstriction. The resulting lesion is referred to as an infarct
(from the ...
. MI can quickly become fatal if emergency medical treatment is not received promptly. If diagnosed within 12 hours of the initial episode (attack) then thrombolytic therapy
Thrombolysis, also called fibrinolytic therapy, is the breakdown (lysis) of blood clots formed in blood vessels, using medication. It is used in ST elevation myocardial infarction, stroke, and in cases of severe venous thromboembolism (massive p ...
is initiated.
Limb ischemia
An arterial thrombus or embolus can also form in the limbs, which can lead to acute limb ischemia.Other sites
Hepatic artery thrombosis
Hepatic artery thrombosis occurs when a blood clot forms in the artery that provides blood flow to the liver. Hepatic artery thrombosis may occur as a complication after liver transplantation, and represents the most common complication of liver t ...
usually occurs as a devastating complication after liver transplantation.
Causes
Thrombosis prevention is initiated with assessing the risk for its development. Some people have a higher risk of developing thrombosis and its possible development into thromboembolism. Some of these risk factors are related toinflammation
Inflammation (from la, inflammatio) is part of the complex biological response of body tissues to harmful stimuli, such as pathogens, damaged cells, or irritants, and is a protective response involving immune cells, blood vessels, and molec ...
. "Virchow's triad
Virchow's triad or the triad of Virchow () describes the three broad categories of factors that are thought to contribute to thrombosis.
*Hypercoagulability
*Hemodynamic changes (stasis, turbulence)
*Endothelial injury/dysfunction
It is named a ...
" has been suggested to describe the three factors necessary for the formation of thrombosis: stasis of blood, vessel wall injury, and altered blood coagulation. Some risk factors predispose for venous thrombosis while others increase the risk of arterial thrombosis. Newborn babies in the neonatal period are also at risk of a thromboembolism.
Mechanism
Pathogenesis
The main causes of thrombosis are given inVirchow's triad
Virchow's triad or the triad of Virchow () describes the three broad categories of factors that are thought to contribute to thrombosis.
*Hypercoagulability
*Hemodynamic changes (stasis, turbulence)
*Endothelial injury/dysfunction
It is named a ...
which lists thrombophilia, endothelial cell injury, and disturbed blood flow
Hemodynamics or haemodynamics are the dynamics of blood flow. The circulatory system is controlled by homeostatic mechanisms of autoregulation, just as hydraulic circuits are controlled by control systems. The hemodynamic response continuously m ...
. Generally speaking the risk for thrombosis increases over the life course of individuals, depending on life style factors like smoking, diet, and physical activity, the presence of other diseases like cancer or autoimmune disease, while also platelet properties change in aging individuals which is an important consideration as well.
Hypercoagulability
Hypercoagulability or ''thrombophilia'', is caused by, for example, genetic deficiencies orautoimmune disorder
An autoimmune disease is a condition arising from an abnormal immune response to a functioning body part. At least 80 types of autoimmune diseases have been identified, with some evidence suggesting that there may be more than 100 types. Nearly ...
s. Recent studies indicate that white blood cells play a pivotal role in deep vein thrombosis, mediating numerous pro-thrombotic actions.
Endothelial cell injury
Any inflammatory process, such as trauma, surgery or infection, can cause damage to the endothelial lining of the vessel's wall. The main mechanism is exposure of tissue factor to the blood coagulation system.labtestsonline > Hypercoagulable DisordersThis article was last reviewed on May 23, 2007 and was last modified on March 6, 2010. Inflammatory and other stimuli (such as
hypercholesterolemia
Hypercholesterolemia, also called high cholesterol, is the presence of high levels of cholesterol in the blood. It is a form of hyperlipidemia (high levels of lipids in the blood), hyperlipoproteinemia (high levels of lipoproteins in the blood), ...
) can lead to changes in gene expression in endothelium producing to a pro-thrombotic state. When this occurs, endothelial cells downregulate substances such as thrombomodulin
Thrombomodulin (TM), CD141 or BDCA-3 is an integral membrane protein expressed on the surface of endothelial cells and serves as a cofactor for thrombin. It reduces blood coagulation by converting thrombin to an anticoagulant enzyme from a procoag ...
, which is a key modulator of thrombin activity. The result is a sustained activation of thrombin and reduced production of protein C
Protein C, also known as autoprothrombin IIA and blood coagulation factor XIX, is a zymogen, that is, an inactive enzyme. The activated form plays an important role in regulating anticoagulation, inflammation, and cell death and maintainin ...
and tissue factor inhibitor, which furthers the pro-thrombotic state.
Endothelial injury is almost invariably involved in the formation of thrombi in arteries, as high rates of blood flow normally hinder clot formation. In addition, arterial and cardiac clots are normally rich in platelets–which are required for clot formation in areas under high stress due to blood flow.
Disturbed blood flow
 Causes of disturbed blood flow include stagnation of blood flow past the point of injury, or
Causes of disturbed blood flow include stagnation of blood flow past the point of injury, or venous stasis
Venostasis, or venous stasis, is a condition of slow blood flow in the veins, usually of the legs.
Presentation Complications
Potential complications of venous stasis are:
* Venous ulcers
* Blood clot formation in veins (venous thrombosis), that ...
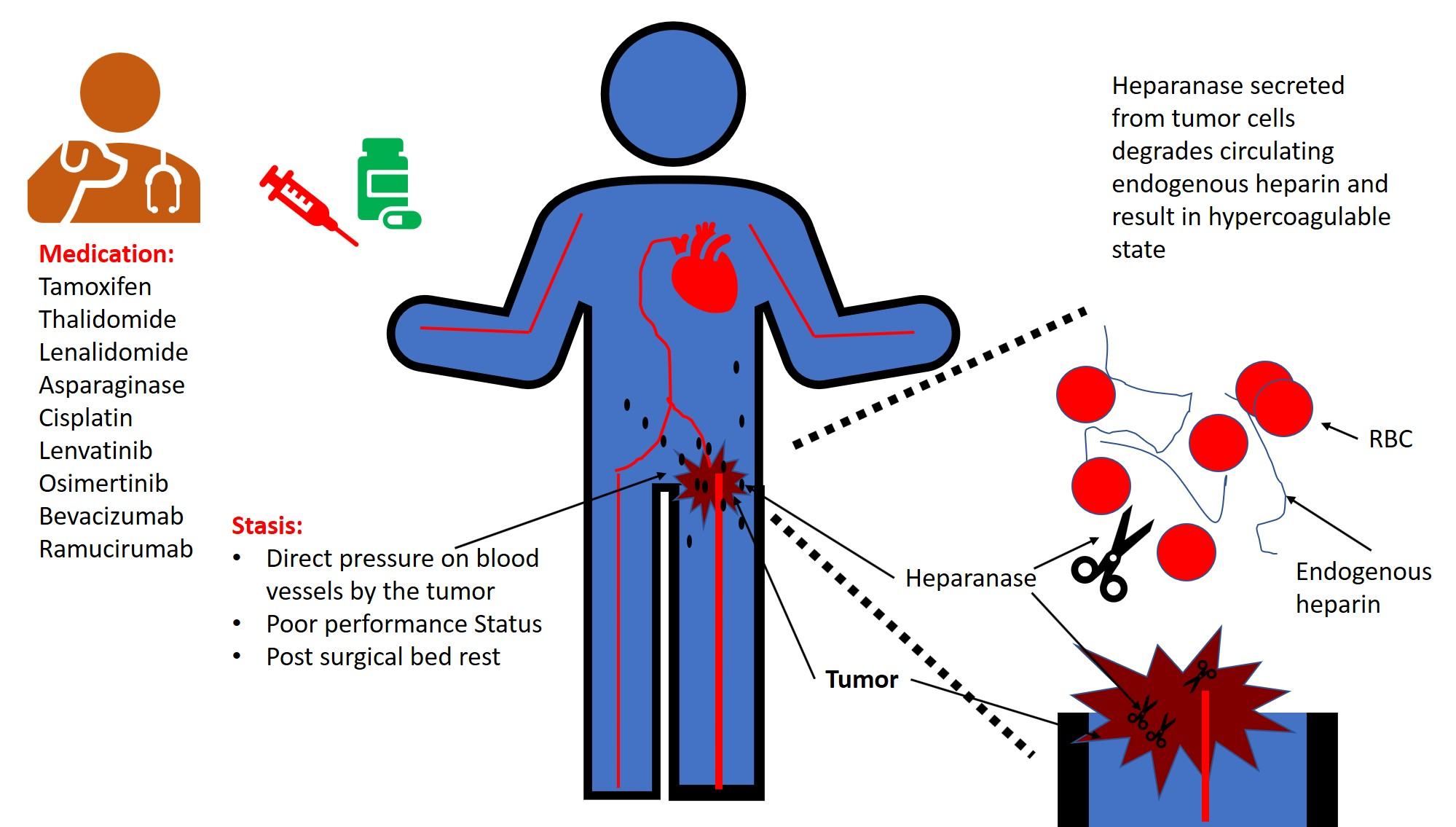
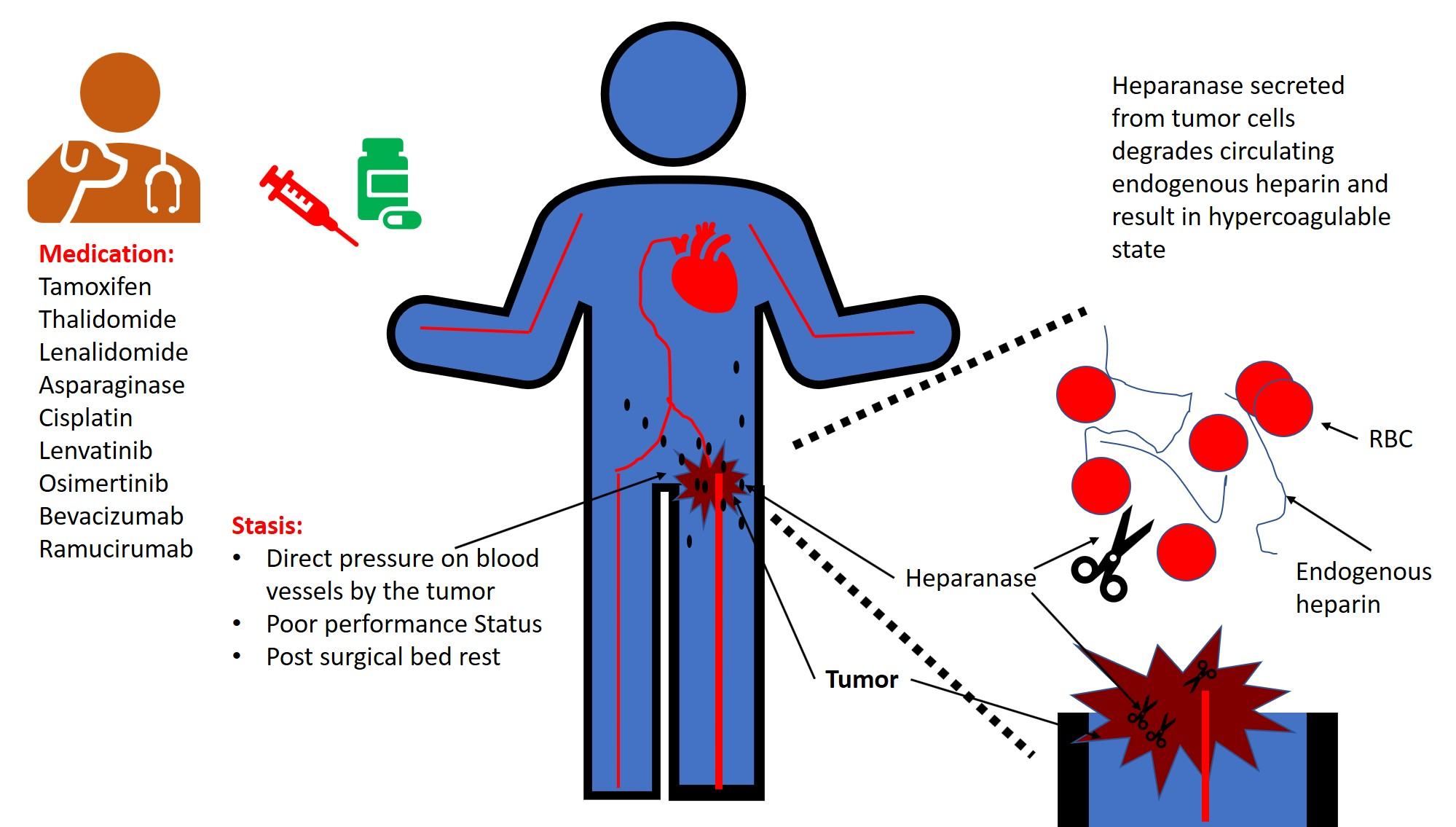
which may occur in heart failure, or after long periods of sedentary behaviour, such as sitting on a long airplane flight. Also, atrial fibrillation, causes stagnant blood in the left atrium (LA), or left atrial appendage (LAA), and can lead to a thromboembolism. Cancers
Cancer is a group of diseases involving abnormal cell growth with the potential to invade or spread to other parts of the body. These contrast with benign tumors, which do not spread. Possible signs and symptoms include a lump, abnormal bl ...
or malignancies such as leukemia
Leukemia ( also spelled leukaemia and pronounced ) is a group of blood cancers that usually begin in the bone marrow and result in high numbers of abnormal blood cells. These blood cells are not fully developed and are called ''blasts'' or ...
may cause increased risk of thrombosis by possible activation of the coagulation system by cancer cells or secretion of procoagulant substances ( paraneoplastic syndrome), by external compression on a blood vessel when a solid tumor is present, or (more rarely) extension into the vasculature (for example, renal cell cancers extending into the renal veins). Also, treatments for cancer (radiation, chemotherapy) often cause additional hypercoagulability. There are scores that correlate different aspects of patient data (comorbidities, vital signs, and others) to risk of thrombosis, such as the POMPE-C, which stratifies risk of mortality due to pulmonary embolism in patients with cancer, who typically have higher rates of thrombosis. Also, there are several predictive scores for thromboembolic events, such as Padua, Khorana, and ThroLy score.
Pathophysiology
Natural history
Fibrinolysis
Fibrinolysis is a process that prevents blood clots from growing and becoming problematic. Primary fibrinolysis is a normal body process, while secondary fibrinolysis is the breakdown of clots due to a medicine, a medical disorder, or some other ...
is the physiological breakdown of blood clots by enzymes such as plasmin
Plasmin is an important enzyme () present in blood that degrades many blood plasma proteins, including fibrin clots. The degradation of fibrin is termed fibrinolysis. In humans, the plasmin protein (in the zymogen form of plasminogen) is encode ...
.
Organisation: following the thrombotic event, residual vascular thrombus will be re-organised histologically with several possible outcomes. For an occlusive thrombus (defined as thrombosis within a small vessel that leads to complete occlusion), wound healing
Wound healing refers to a living organism's replacement of destroyed or damaged tissue by newly produced tissue.
In undamaged skin, the epidermis (surface, epithelial layer) and dermis (deeper, connective layer) form a protective barrier again ...
will reorganise the occlusive thrombus into collagenous scar
A scar (or scar tissue) is an area of fibrous tissue that replaces normal skin after an injury. Scars result from the biological process of wound repair in the skin, as well as in other organs, and tissues of the body. Thus, scarring is a n ...
tissue, where the scar tissue will either permanently obstruct the vessel, or contract down with myofibroblastic activity to unblock the lumen. For a mural thrombus (defined as a thrombus in a large vessel that restricts the blood flow but does not occlude completely), histological reorganisation of the thrombus does not occur via the classic wound healing
Wound healing refers to a living organism's replacement of destroyed or damaged tissue by newly produced tissue.
In undamaged skin, the epidermis (surface, epithelial layer) and dermis (deeper, connective layer) form a protective barrier again ...
mechanism. Instead, the platelet-derived growth factor degranulated by the clotted platelet
Platelets, also called thrombocytes (from Greek θρόμβος, "clot" and κύτος, "cell"), are a component of blood whose function (along with the coagulation factors) is to react to bleeding from blood vessel injury by clumping, thereby i ...
s will attract a layer of smooth muscle cells to cover the clot, and this layer of mural smooth muscle will be vascularised by the blood inside the vessel lumen rather than by the vasa vasorum
Vasa vasorum are small blood vessels that comprise a vascular network supplying the walls of large blood vessels, such as elastic arteries (e.g., the aorta) and large veins (e.g., the venae cavae).
The name derives . Occasionally two differen ...
.
Ischemia/infarction: if an arterial thrombus cannot be lysed by the body and it does not embolise, and if the thrombus is large enough to impair or occlude blood flow in the involved artery, then local ischemia or infarction
Infarction is tissue death ( necrosis) due to inadequate blood supply to the affected area. It may be caused by artery blockages, rupture, mechanical compression, or vasoconstriction. The resulting lesion is referred to as an infarct
(from th ...
will result. A venous thrombus may or may not be ischemic, since veins distribute deoxygenated blood that is less vital for cellular metabolism. Nevertheless, non-ischemic venous thrombosis may still be problematic, due to the swelling caused by blockage to venous drainage. In deep vein thrombosis
Deep vein thrombosis (DVT) is a type of venous thrombosis involving the formation of a blood clot in a deep vein, most commonly in the legs or pelvis. A minority of DVTs occur in the arms. Symptoms can include pain, swelling, redness, and enla ...
this manifests as pain, redness, and swelling; in retinal vein occlusion this may result in macular oedema and visual acuity impairment, which if severe enough can lead to blindness
Visual impairment, also known as vision impairment, is a medical definition primarily measured based on an individual's better eye visual acuity; in the absence of treatment such as correctable eyewear, assistive devices, and medical treatment� ...
.
Embolization
A thrombus may become detached and enter circulation as anembolus
An embolus (; plural emboli; from the Greek ἔμβολος "wedge", "plug") is an unattached mass that travels through the bloodstream and is capable of creating blockages. When an embolus occludes a blood vessel, it is called an embolism or emb ...
, finally lodging in and completely obstructing a blood vessel, which unless treated very quickly will lead to tissue necrosis (an infarction
Infarction is tissue death ( necrosis) due to inadequate blood supply to the affected area. It may be caused by artery blockages, rupture, mechanical compression, or vasoconstriction. The resulting lesion is referred to as an infarct
(from th ...
) in the area past the occlusion. Venous thrombosis can lead to pulmonary embolism when the migrated embolus becomes lodged in the lung. In people with a "shunt" (a connection between the pulmonary and systemic circulation), either in the heart or in the lung, a venous clot can also end up in the arteries and cause arterial embolism.
Arterial embolism can lead to obstruction of blood flow through the blood vessel that is obstructed by it, and a lack of oxygen and nutrients ( ischemia) of the downstream tissue. The tissue can become irreversibly damaged, a process known as necrosis. This can affect any organ; for instance, arterial embolism of the brain is one of the causes of stroke.
Prevention
The use of heparin following surgery is common if there are no issues with bleeding. Generally, a risk-benefit analysis is required, as all anticoagulants lead to an increased risk of bleeding. In people admitted to hospital, thrombosis is a major cause for complications and occasionally death. In the UK, for instance, the Parliamentary Health Select Committee heard in 2005 that the annual rate of death due to thrombosis was 25,000, with at least 50% of these being hospital-acquired. Hence ''thromboprophylaxis'' (prevention of thrombosis) is increasingly emphasized. In patients admitted for surgery, graded compression stockings are widely used, and in severe illness, prolonged immobility and in allorthopedic surgery
Orthopedic surgery or orthopedics ( alternatively spelt orthopaedics), is the branch of surgery concerned with conditions involving the musculoskeletal system. Orthopedic surgeons use both surgical and nonsurgical means to treat musculoskeletal ...
, professional guidelines recommend low molecular weight heparin
Low-molecular-weight heparin (LMWH) is a class of anticoagulant medications. They are used in the prevention of blood clots and treatment of venous thromboembolism (deep vein thrombosis and pulmonary embolism) and in the treatment of myocardial in ...
(LMWH) administration, mechanical calf compression or (if all else is contraindicated and the patient has recently developed deep vein thrombosis) the insertion of a vena cava filter. In patients with medical rather than surgical illness, LMWH too is known to prevent thrombosis, and in the United Kingdom
The United Kingdom of Great Britain and Northern Ireland, commonly known as the United Kingdom (UK) or Britain, is a country in Europe, off the north-western coast of the European mainland, continental mainland. It comprises England, Scotlan ...
the Chief Medical Officer has issued guidance to the effect that preventative measures should be used in medical patients, in anticipation of formal guidelines.
Treatment
The treatment for thrombosis depends on whether it is in a vein or an artery, the impact on the person, and the risk of complications from treatment.Anticoagulation
Warfarin andvitamin K antagonists
Vitamin K antagonists (VKA) are a group of substances that reduce blood clotting by reducing the action of vitamin K. The term "vitamin K antagonist" is technically a misnomer, as the drugs do not directly antagonise the action of vitamin K in t ...
are anticoagulants that can be taken orally to reduce thromboembolic occurrence. Where a more effective response is required, heparin can be given (by injection) concomitantly. As a side effect of any anticoagulant, the risk of bleeding
Bleeding, hemorrhage, haemorrhage or blood loss, is blood escaping from the circulatory system from damaged blood vessels. Bleeding can occur internally, or externally either through a natural opening such as the mouth, nose, ear, urethra, vag ...
is increased, so the international normalized ratio of blood is monitored. Self-monitoring and self-management are safe options for competent patients, though their practice varies. In Germany, about 20% of patients were self-managed while only 1% of U.S. patients did home self-testing (according to one 2012 study). Other medications such as direct thrombin inhibitor Direct thrombin inhibitors (DTIs) are a class of medication that act as anticoagulants (delaying blood clotting) by directly inhibiting the enzyme thrombin (factor IIa). Some are in clinical use, while others are undergoing clinical development. Sev ...
s and direct Xa inhibitor
Direct factor Xa inhibitors (xabans) are anticoagulants (blood thinning drugs), used to both treat and prevent blood clots in veins, and prevent stroke and embolism in people with atrial fibrillation (AF).
Medical use
Direct factor Xa inhibito ...
s are increasingly being used instead of warfarin.
Thrombolysis
Thrombolysis
Thrombolysis, also called fibrinolytic therapy, is the breakdown (lysis) of blood clots formed in blood vessels, using medication. It is used in ST elevation myocardial infarction, stroke, and in cases of severe venous thromboembolism (massive ...
is the pharmacological destruction of blood clots by administering thrombolytic drug
Thrombolysis, also called fibrinolytic therapy, is the breakdown (lysis) of blood clots formed in blood vessels, using medication. It is used in ST elevation myocardial infarction, stroke, and in cases of severe venous thromboembolism (massive ...
s including recombinant tissue plasminogen activator
Tissue plasminogen activator (abbreviated tPA or PLAT) is a protein involved in the breakdown of blood clots. It is a serine protease () found on endothelial cells, the cells that line the blood vessels. As an enzyme, it catalysis, catalyzes the c ...
, which enhances the normal destruction of blood clots by the body's enzymes. This carries an increased risk of bleeding so is generally only used for specific situations (such as severe stroke or a massive pulmonary embolism).
Surgery
Arterial thrombosis may require surgery if it causes acute limb ischemia.Endovascular treatment
Mechanical clot retrieval and catheter-guided thrombolysis are used in certain situations.Antiplatelet agents
Arterial thrombosis is platelet-rich, and inhibition of platelet aggregation withantiplatelet drug
An antiplatelet drug (antiaggregant), also known as a platelet agglutination inhibitor or platelet aggregation inhibitor, is a member of a class of pharmaceuticals that decrease platelet aggregation and inhibit thrombus formation. They are effecti ...
s such as aspirin
Aspirin, also known as acetylsalicylic acid (ASA), is a nonsteroidal anti-inflammatory drug (NSAID) used to reduce pain, fever, and/or inflammation, and as an antithrombotic. Specific inflammatory conditions which aspirin is used to treat inc ...
may reduce the risk of recurrence or progression.
Targeting ischemia/reperfusion injury
With reperfusion comes ischemia/reperfusion (IR) injury (IRI), which paradoxically causes cell death in reperfused tissue and contributes significantly to post-reperfusion mortality and morbidity. For example, in a feline model of intestinal ischemia, four hours of ischemia resulted in less injury than three hours of ischemia followed by one hour of reperfusion. In ST-elevation myocardial infarction (STEMI), IRI contributes up to 50% of final infarct size despite timely primary percutaneous coronary intervention. This is a key reason for the continued high mortality and morbidity in these conditions, despite endovascular reperfusion treatments and continuous efforts to improve timeliness and access to these treatments. Hence, protective therapies are required to attenuate IRI alongside reperfusion in acute ischemic conditions to improve clinical outcomes. Therapeutic strategies that have potential to improve clinical outcomes in reperfused STEMI patients include remote ischemic conditioning (RIC), exenatide, and metoprolol. These have emerged amongst a multitude of cardioprotective interventions investigated with largely neutral clinical data. Of these, RIC has the most robust clinical evidence, especially in the context of STEMI, but also emerging for other indications such as acute ischemic stroke and aneurysmal subarachnoid hemorrhage.Neonatal thrombosis
Treatment options for full-term and preterm babies who develop thromboembolism include expectant management (with careful observation), nitroglycerin ointment, pharmacological therapy (thrombolytics and/or anticoagulants), and surgery. The evidence supporting these treatment approaches is weak. For anticoagulant treatment, t is not clear if unfractionated and/or low molecular weight heparin treatment is effective at decreasing mortality and serious adverse events in this population. There is also insufficient evidence to understand the risk of adverse effects associated with these treatment approaches in term or preterm infants.See also
* Blood clotting tests * Disseminated intravascular coagulation *Hepatic artery thrombosis
Hepatic artery thrombosis occurs when a blood clot forms in the artery that provides blood flow to the liver. Hepatic artery thrombosis may occur as a complication after liver transplantation, and represents the most common complication of liver t ...
* Thrombotic microangiopathy
References
Bibliography
* * * * *External links
* * {{Authority control Hematology