orchiectomy on:
[Wikipedia]
[Google]
[Amazon]
Orchiectomy (also named orchidectomy, and sometimes shortened as orchi or orchie) is a
surgical procedure
Surgery ''cheirourgikē'' (composed of χείρ, "hand", and ἔργον, "work"), via la, chirurgiae, meaning "hand work". is a medical specialty that uses operative manual and instrumental techniques on a person to investigate or treat a pa ...
in which one or both testicle
A testicle or testis (plural testes) is the male reproductive gland or gonad in all bilaterians, including humans. It is homologous to the female ovary. The functions of the testes are to produce both sperm and androgens, primarily testoste ...
s are removed. The surgery is performed as treatment for testicular cancer
Testicular cancer is cancer that develops in the testicles, a part of the male reproductive system. Symptoms may include a lump in the testicle, or swelling or pain in the scrotum. Treatment may result in infertility.
Risk factors include a ...
, as part of surgery for transgender women, as management for advanced prostate cancer
Prostate cancer is cancer of the prostate. Prostate cancer is the second most common cancerous tumor worldwide and is the fifth leading cause of cancer-related mortality among men. The prostate is a gland in the male reproductive system that su ...
, and to remove damaged testes after testicular torsion
Testicular torsion occurs when the spermatic cord (from which the testicle is suspended) twists, cutting off the blood supply to the testicle. The most common symptom in children is sudden, severe testicular pain. The testicle may be higher than ...
. Less frequently, orchiectomy may be performed following a trauma, or due to wasting away of the testis or testes.
Procedure
Simple orchiectomy
A simple orchiectomy is commonly performed as part ofgender reassignment surgery
Gender-affirming surgery (GAS) is a surgical procedure, or series of procedures, that alters a transgender or transsexual person's physical appearance and sexual characteristics to resemble those associated with their identified gender, and all ...
for transgender women
A trans woman or a transgender woman is a woman who was assigned male at birth. Trans women have a female gender identity, may experience gender dysphoria, and may transition; this process commonly includes hormone replacement therapy and so ...
, or as palliative treatment
Palliative care (derived from the Latin root , or 'to cloak') is an interdisciplinary medical caregiving approach aimed at optimizing quality of life and mitigating suffering among people with serious, complex, and often terminal illnesses. Wit ...
for advanced cases of prostate cancer
Prostate cancer is cancer of the prostate. Prostate cancer is the second most common cancerous tumor worldwide and is the fifth leading cause of cancer-related mortality among men. The prostate is a gland in the male reproductive system that su ...
. A simple orchiectomy may also be required in the event of testicular torsion
Testicular torsion occurs when the spermatic cord (from which the testicle is suspended) twists, cutting off the blood supply to the testicle. The most common symptom in children is sudden, severe testicular pain. The testicle may be higher than ...
.
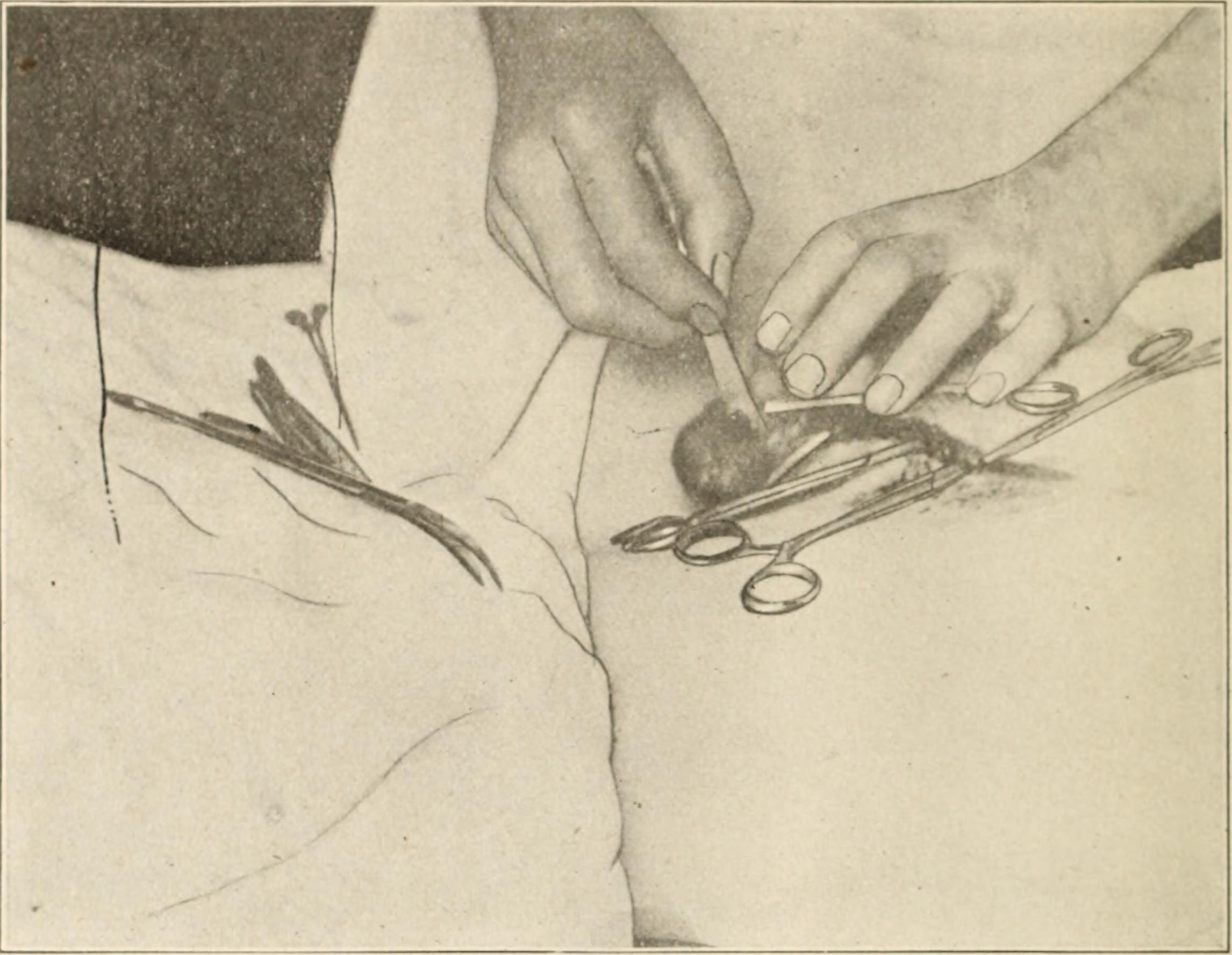
For the procedure, the person lies flat on an operating table with the penis
A penis (plural ''penises'' or ''penes'' () is the primary sexual organ that male animals use to inseminate females (or hermaphrodites) during copulation. Such organs occur in many animals, both vertebrate and invertebrate, but males d ...
taped against the abdomen
The abdomen (colloquially called the belly, tummy, midriff, tucky or stomach) is the part of the body between the thorax (chest) and pelvis, in humans and in other vertebrates. The abdomen is the front part of the abdominal segment of the to ...
. The nurse shaves a small area for the incision. After anesthetic has been administered, the surgeon makes an incision in the midpoint of the scrotum
The scrotum or scrotal sac is an anatomical male reproductive structure located at the base of the penis that consists of a suspended dual-chambered sac of skin and smooth muscle. It is present in most terrestrial male mammals. The scrotum co ...
and cuts through the underlying tissue. The surgeon removes the testicles and parts of the spermatic cord
The spermatic cord is the cord-like structure in males formed by the vas deferens (''ductus deferens'') and surrounding tissue that runs from the deep inguinal ring down to each testicle. Its serosal covering, the tunica vaginalis, is an exten ...
through the incision. The incision is closed with two layers of sutures and is covered with a surgical dressing. If desired, prosthetic testicle A prosthetic testicle is an artificial replacement for a testicle lost through surgery or injury. Consisting of a plastic ovoid manufactured from silicone rubber Silicone rubber is an elastomer (rubber-like material) composed of silicone—it ...
s can be inserted before the incision is closed to present an outward appearance of a pre-surgical scrotum.
Subcapsular orchiectomy
A subcapsular orchiectomy is also commonly performed for treatment of prostate cancer. The operation is similar to that of a simple orchiectomy, with the exception that the glandular tissue that surrounds each testicle is removed rather than the entire testis itself. This type of orchiectomy is performed to remove testosterone-producing glandular tissue while maintaining the appearance of an ordinary scrotum.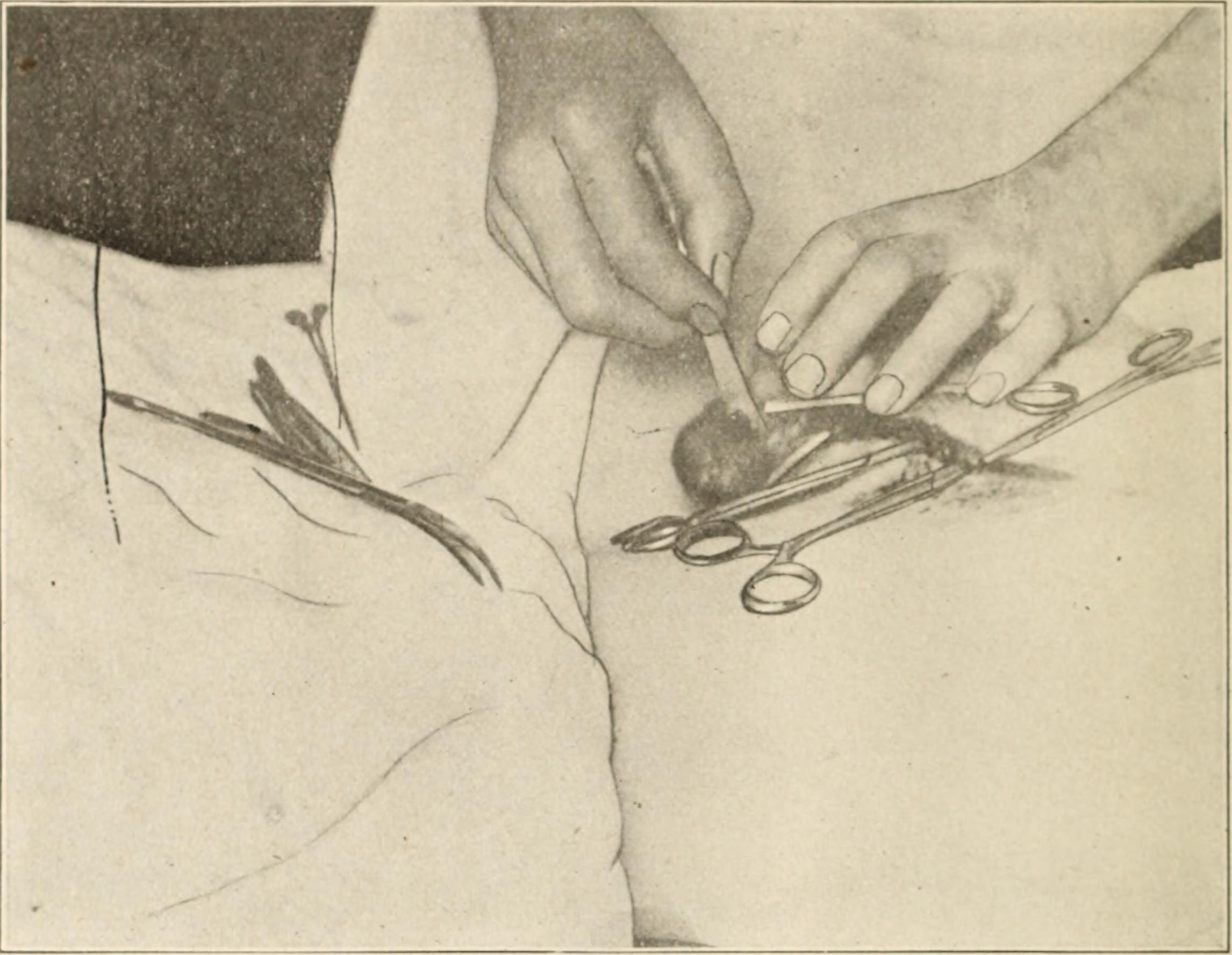
Inguinal orchiectomy
Inguinal orchiectomy (named from the Latin ''inguen'' for "groin", and also called radical orchiectomy) is performed when an onset oftesticular cancer
Testicular cancer is cancer that develops in the testicles, a part of the male reproductive system. Symptoms may include a lump in the testicle, or swelling or pain in the scrotum. Treatment may result in infertility.
Risk factors include a ...
is suspected, in order to prevent a possible spread of cancer from the spermatic cord into the lymph nodes near the kidneys.
An inguinal orchiectomy can be either unilateral (one testicle) or bilateral (both testicles). The surgeon makes an incision in the groin area (in contrast to an incision in the scrotum, as is done in both simple and subcapsular orchiectomies). The entire spermatic cord
The spermatic cord is the cord-like structure in males formed by the vas deferens (''ductus deferens'') and surrounding tissue that runs from the deep inguinal ring down to each testicle. Its serosal covering, the tunica vaginalis, is an exten ...
is removed, as well as the testicle(s). A long, non-absorbable suture may be left in the stump of the spermatic cord in case later surgery is deemed necessary. After the cord and testicle(s) have been removed, the surgeon washes the area with saline solution and closes the layers of tissues and skin with sutures. The wound is then covered with sterile gauze and bandaged.
Partial orchiectomy
Partial orchiectomy is an option for individuals with testicular masses that want to preserve their testes and their function. During surgery, the testis is exposed in a similar way to inguinal orchiectomy. Once the testis is exposed and the spermatic cord is clamped, there is a current debate as to whether surgeons should deliver cold ischaemia which means submitting the organ, in this case the testis, into a cold/freezing environment. Whether or not it is submerged and frozen, the next step is to cut thetunica vaginalis
The tunica vaginalis is the pouch of serous membrane that covers the testes. It is derived from the vaginal process of the peritoneum, which in the fetus precedes the descent of the testes from the abdomen into the scrotum.
After its descent, ...
and an ultrasound is used to find the tumor. After, the tumor is scraped away from the testis in a process called enucleation. Following enucleation, biopsies are taken of the tissues surrounding the testicle where the mass once was. Afterwards, each layer or tunica of the testis is sutured up and the testis is placed back in the scrotum. The skin layers are also closed up with sutures.
Pre-operative considerations
Guidelines state that fertility counseling should be offered to all patients undergoing inguinal orchiectomy, as there is a risk of reduced fertility or infertility. Testicular germ cell tumors (TGCT) accounts for 95% of cases of testicular cancer in young men. TGCT is associated with abnormal semen parameters. Because testicular cancer is commonly diagnosed in young, fertile men, it is critical that these individuals be educated on preserving their semen through freezing (cryopreservation
Cryo-preservation or cryo-conservation is a process where organisms, organelles, cells, tissues, extracellular matrix, organs, or any other biological constructs susceptible to damage caused by unregulated chemical kinetics are preserved by co ...
) and complete a fertility assessment prior to surgery. In addition, testicular prosthesis placement counseling and education is encouraged to be given before an individual undergoes orchiectomy or before inguinal exploration with possibility of orchiectomy. This is an elective surgery which can be done at the time of orchiectomy. Testicular prosthesic placement has known psychological benefits (see below). Although risks for complications with prosthesis is low, individuals should also be informed of the possibility of infection, rotation, and replacement of prosthesis.
Post-operative care
Following orchiectomy, those who have undergone the procedure are advised to avoid bathing, swimming, and heavy lifting for at least one month. If an individual had previously been taking hormone and/or hormone-blocking medications, modifications to their medication would be needed after the procedure. Any androgen-blocking medications, such asspironolactone
Spironolactone, sold under the brand name Aldactone among others, is a medication that is primarily used to treat fluid build-up due to heart failure, liver scarring, or kidney disease. It is also used in the treatment of high blood press ...
or cyproterone, are stopped, and estrogen hormones can be resumed at the doctor's discretion. Post-operative pain management includes icing the surgical site, wearing supportive underwear, and the use of pain relief medications (analgesic
An analgesic drug, also called simply an analgesic (American English), analgaesic (British English), pain reliever, or painkiller, is any member of the group of drugs used to achieve relief from pain (that is, analgesia or pain management). It ...
s) such as acetaminophen or ibuprofen; for more severe pain, narcotic analgesics
Opioids are substances that act on opioid receptors to produce morphine-like effects. Medically they are primarily used for pain relief, including anesthesia. Other medical uses include suppression of diarrhea, replacement therapy for opioid use ...
may be needed. A follow-up appointment to monitor recovery and healing is routine.
Risks and complications
Risks and complications should be discussed with an individual pre-operatively. Risks and complications for inguinal orchiectomy include scrotal hematoma (accumulation of blood in the scrotum), infection, post-operative pain (60% initially, 1.8% 1 year after), phantom testis syndrome (pain in the kidney as a result from trauma from the testicle), reduced fertility, and with the more rare complications being inguinal hernia, ilioinguinal nerve injury, tumor spillage, and hypogonadism.Effects
Unilateral orchiectomy results in decreased sperm count but does not reduce testosterone levels. Bilateral orchiectomy causes infertility and greatly reduced testosterone levels. This can lead to side effects including loss of sexual interest,erectile dysfunction
Erectile dysfunction (ED), also called impotence, is the type of sexual dysfunction in which the penis fails to become or stay erect during sexual activity. It is the most common sexual problem in men.Cunningham GR, Rosen RC. Overview of ma ...
, hot flashes, breast enlargement (''gynecomastia
Gynecomastia (also spelled gynaecomastia) is the abnormal non-cancerous enlargement of one or both breasts in males due to the growth of breast tissue as a result of a hormone imbalance between estrogens and androgens. Updated by Brent Wisse ( ...
''), weight gain, loss of muscle mass, and osteoporosis
Osteoporosis is a systemic skeletal disorder characterized by low bone mass, micro-architectural deterioration of bone tissue leading to bone fragility, and consequent increase in fracture risk. It is the most common reason for a broken bone a ...
. It has been discovered that some individuals with a history of prostate cancer who had bilateral orchiectomy had effects on their new bone production, resulting in increased risk of bone fractures due to testosterone deficiency after the procedure.
Bilateral orchiectomy also reduces the use of exogenous medications for transgender women; the reduction in testosterone eliminates the need for testosterone-blocking medications and can contribute to feminizing features such as breast enlargement.
Psychosocial effects
The loss of one or both testicles from orchiectomy can have severe implications in a male's identity and self-image surrounding masculinity, such that it can lead to an individual having thoughts of hopelessness, inadequacy, and loss. Among testicular cancer survivors who have lost a testicle, there are feelings of shame and loss, which are more evident in young and single men than older and non-single men. As many as one third of individuals who will undergo orchiectomy are not offered the option of having a testicular prosthesis. Data shows that simply offering testicular prosthesis to individuals undergoing orchioectomy is psychologically beneficial. While some individuals do not mind losing a testicle, studies have shown that there is a change in body image in testicular cancer survivors who have undergone orchiectomy and an improvement in body image in 50-60% of individuals who undergo testicular prosthesis placement. One year after testicular prosthesis placement, there are reports of increase in self-esteem and psychological well-being during sexual activity in a study that followed up on post-orchiectomy individuals including adolescents. On the other hand, there is a current debate whether children undergoing orchiectomy should be offered testicular prosthesis to be inserted at the time of orchiectomy procedure.Medical uses
Orchiectomy as a gender reassignment procedure
Bilateral simple orchiectomy is one option forgender reassignment surgery
Gender-affirming surgery (GAS) is a surgical procedure, or series of procedures, that alters a transgender or transsexual person's physical appearance and sexual characteristics to resemble those associated with their identified gender, and all ...
for transgender women. It may be performed as a standalone procedure or at the same time as a vaginoplasty
Vaginoplasty is any surgical procedure that results in the construction or reconstruction of the vagina. It is a type of genitoplasty. Pelvic organ prolapse is often treated with one or more surgeries to repair the vagina. Sometimes a vaginopl ...
. Bilateral orchiectomy is considered first before undergoing vaginoplasty. Vaginoplasty can still be administered after undergoing bilateral orchiectomy, as the orchiectomy preserves the penoscrotal skin that can later be transformed into a skin flap. Additionally, it is an option for those who are unable to undergo vaginoplasty due to the risk of complications.
In addition to alleviating gender dysphoria
Gender dysphoria (GD) is the distress a person experiences due to a mismatch between their gender identitytheir personal sense of their own genderand their sex assigned at birth. The diagnostic label gender identity disorder (GID) was used unti ...
, the procedure allows trans women to stop taking testosterone-blocking medications, which may cause unwanted side effects. Some common testosterone-blocking medications that most use before undergoing orchiectomy are spironolactone
Spironolactone, sold under the brand name Aldactone among others, is a medication that is primarily used to treat fluid build-up due to heart failure, liver scarring, or kidney disease. It is also used in the treatment of high blood press ...
and cyproterone. Common side effects caused by spironolactone are drowsiness, confusion, headache, fatigue, nausea/vomiting, gastritis
Gastritis is inflammation of the lining of the stomach. It may occur as a short episode or may be of a long duration. There may be no symptoms but, when symptoms are present, the most common is upper abdominal pain (see dyspepsia). Other possi ...
, polyuria
Polyuria () is excessive or an abnormally large production or passage of urine (greater than 2.5 L or 3 L over 24 hours in adults). Increased production and passage of urine may also be termed diuresis. Polyuria often appears in conjunction wi ...
, polydipsia
Polydipsia is excessive thirst or excess drinking.Porth, C. M. (1990). ''Pathophysiology: Concepts of altered health states''. Philadelphia: J.B. Lippincott Company. The word derives from the Greek () "very thirsty", which is derived from (, " ...
, and electrolyte imbalance (hyperkalemia
Hyperkalemia is an elevated level of potassium (K+) in the blood. Normal potassium levels are between 3.5 and 5.0mmol/L (3.5 and 5.0mEq/L) with levels above 5.5mmol/L defined as hyperkalemia. Typically hyperkalemia does not cause symptoms. Occa ...
). Cyproterone can cause side effects such as fatigue, low mood, and fulminant hepatitis
Hepatitis is inflammation of the liver tissue. Some people or animals with hepatitis have no symptoms, whereas others develop yellow discoloration of the skin and whites of the eyes (jaundice), poor appetite, vomiting, tiredness, abdominal pai ...
. Orchiectomy allows individuals to stop taking these medications and avoid these adverse effects. It is also an alternative for trans women who have contraindications to antiandrogens and is a minimally invasive procedure to eliminate testosterone levels.
Pre-operative evaluation
= World Professional Association for Transgender Health (WPATH) criteria
= Criteria from the World Professional Association for Transgender Health (WPATH) are used as a framework to guide health care professionals in approving or denying an orchiectomy. When a transgender individual wants to complete an orchiectomy, they are in a state of gender incongruence and they must meet the criteria before having the procedure done. The criteria are as follows: "(i) persistent, documented gender dysphoria, (ii) capacity to make informed decisions and consent to treatment, (iii) well-controlled medical or mental health comorbidities, and (iv) the use of hormone therapy for 12 months." Additionally, persons wishing to go through with the procedure are required to obtain referrals from two independent qualified mental health professionals. This referral should include "the individual's demographic information, psychosocial assessment results, duration of the therapeutic relationship, type of evaluation and therapy performed, if the criteria for surgery have been met and if informed consent has been obtained from the patient."Other medical considerations
An individual seeking to undergo orchiectomy is evaluated by a healthcare provider to ensure that the procedure is safe. Many candidates for orchiectomy are on estrogen therapy before the operation, which increases risk of intraoperativevenous thromboembolism
Venous thrombosis is blockage of a vein caused by a thrombus (blood clot). A common form of venous thrombosis is deep vein thrombosis (DVT), when a blood clot forms in the deep veins. If a thrombus breaks off (embolizes) and flows to the lungs to ...
(VTE); thus, the provider must take this risk into account and determine whether prophylaxis
Preventive healthcare, or prophylaxis, consists of measures taken for the purposes of disease prevention.Hugh R. Leavell and E. Gurney Clark as "the science and art of preventing disease, prolonging life, and promoting physical and mental hea ...
(prevention) is necessary. Current smokers, individuals with limited mobility, individuals older than the age of 40, and individuals who have a medical history of thrombolytic disorder are at higher risk of developing VTE. For these high-risk populations, the use of sequential compression devices during the operation is recommended to prevent VTE complications.
Orchiectomy as diagnosis and treatment for testicular cancer
Testicular cancer most commonly occurs in males ages 15 to 34. In 2017, there were 8,850 new cases and 410 deaths in the United States. The American Urological Association (AUA) and European Association of Urology (EAU) 2019 guidelines recommend imaging with testicular ultrasound in any individual suspected of having testicular cancer following a physical examination. The ultrasound aids in differentiating diagnoses so that the individual may avoid the need of the surgical approach of inguinal orchiectomy. Inguinal orchiectomy is the gold standard treatment approach for those with confirmed malignancy of testicular cancer. Thus, it is imperative to diagnose the individual as having benign tumor vs. malignant tumor. Benign tumors are cancerous masses typically outside the testicle or surrounding it (extratesticular), whereas the malignant tumors typically lie within/inside the testicle (intratesticular). An orchiectomy is used not only as a treatment option, but also as a diagnostic tool for testicular cancer. Before an orchiectomy is deemed necessary, liver function tests, tumor markers, and various blood panels are taken to confirm the presence of testicular cancer. Tumor markers that may be checked include beta human chorionic gonadotropin,lactate dehydrogenase
Lactate dehydrogenase (LDH or LD) is an enzyme found in nearly all living cells. LDH catalyzes the conversion of lactate to pyruvate and back, as it converts NAD+ to NADH and back. A dehydrogenase is an enzyme that transfers a hydride from one ...
, and alpha fetoprotein
Alpha-fetoprotein (AFP, α-fetoprotein; also sometimes called alpha-1-fetoprotein, alpha-fetoglobulin, or alpha fetal protein) is a protein that in humans is encoded by the ''AFP'' gene. The ''AFP'' gene is located on the ''q'' arm of chromosome ...
. These markers are rechecked after orchiectomy to stage the testicular cancer. Imaging, including chest radiograph
A chest radiograph, called a chest X-ray (CXR), or chest film, is a projection radiograph of the chest used to diagnose conditions affecting the chest, its contents, and nearby structures. Chest radiographs are the most common film taken in med ...
y and an abdominal/pelvic CT (computed tomography) are also performed after orchiectomy to evaluate for metastasis
Metastasis is a pathogenic agent's spread from an initial or primary site to a different or secondary site within the host's body; the term is typically used when referring to metastasis by a cancerous tumor. The newly pathological sites, the ...
. An inguinal orchiectomy is the primary treatment for any cancerous tumor that is found in the testicles; however, in cases where tumors are small, testis- or testes-sparing surgery may be performed instead.
Partial orchiectomy, also known as testis-sparing surgery, is another treatment option for smaller testicular masses which is becoming widely popular in recent years. This treatment option is an alternative to remove testicular cancer masses which are <20mm, have a high probability of being benign, and with negative serum tumor markers. Its benefits include preserving fertility and normal hormone function.
About half of testicular cancer germ cell tumors are seminoma
A seminoma is a germ cell tumor of the testicle or, more rarely, the mediastinum or other extra-gonadal locations. It is a malignant neoplasm and is one of the most treatable and curable cancers, with a survival rate above 95% if discovered in ...
s. Individuals with seminomas are 80-85% likely to have a stage 1 diagnosis and the individual must undergo surveillance every 3–6 months in the first year following their orchiectomy, with an abdominal/pelvic CT at 3,6 and 12 months. Additional treatment such as chemotherapy may be given if they have risk factors for a relapse. Men with stage 1 seminoma after orchiectomy have been shown to be free from a relapse for five years following orchiectomy.
Orchiectomy as a complication of testicular torsion
Among children and adolescents diagnosed withtesticular torsion
Testicular torsion occurs when the spermatic cord (from which the testicle is suspended) twists, cutting off the blood supply to the testicle. The most common symptom in children is sudden, severe testicular pain. The testicle may be higher than ...
, the orchiectomy rate is as high as 42%. Though the goal during surgery is to correct the twist of the spermatic cord, orchiectomy is performed if the testicle is examined during the surgery to have dead tissue (necrosis
Necrosis () is a form of cell injury which results in the premature death of cells in living tissue by autolysis. Necrosis is caused by factors external to the cell or tissue, such as infection, or trauma which result in the unregulated diges ...
) and suspected to no longer be a functioning testicle (no fertility). Delays in diagnosis and treatment increase the risk of orchiectomy, with diagnosis in the first four to eight hours of symptoms being critical to prevent permanent ischemic damage, decreased fertility, and need for orchiectomy.
Orchiectomy for prostate cancer
Prostate cancer, if non-metastatic, is commonly treated with radical prostatectomy or radiation therapy. Less often, orchiectomy is used to treat prostate cancer. Prostate cancer grows in the presence of testosterone. When testosterone is present, " it is metabolized and converted into dihydrotestosterone (DHT) which stimulates the growth of prostate cells. This leads to normal prostate growth in adolescents but contributes to abnormal cell growth in older men." Reducing the amount of testosterone in a person is one way in which prostate cancer is treated. If the prostate cancer is in fact metastatic, then orchiectomy may be used "...to abolish the stimulation of cancer cells by inhibiting testicular testosterone production and thereby reducing androgen levels in the blood: so-called androgen deprivation therapy (ADT)." Castration or orchiectomy is a suitable option for androgen deprivation therapy, and it should be used if a very quick reduction in testosterone levels is needed. However, in recent years, orchiectomy is not commonly used since medical castration is a viable option. Medical castration means that drugs or medications are used to suppress the production of androgens such as testosterone. Some examples of medications used in medical castration include, euprolide, goserelin (Zoladex), buserelin, and triptorelin (Trelstar). Some of the side effects of these medications include but are not limited to "Reduced sexual desire and libido, Impotence, reduced size of testes and penis, hot flashes, growth of breast tissue (gynaecomastia) and pain across the breasts, thinning of the bones or osteoporosis and risk of fracture, anemia, loss of muscle mass, weight gain, fatigue and memory problems, and depression."Orchiectomy for pediatric testis tumors
Until the mid-1980s, pediatric testis tumors were managed in accordance with adult guidelines where the standard therapy was radical inguinal orchiectomy. It was later discovered that this procedure was being overused in the pediatric population, particularly those in pre-puberty, because it was assumed that the tumor was malignant. It was discovered that the majority of the pediatric tumor registries over reported malignant tumors and had biased reporting. It has now been found that most tumors are benign lesions and the majority are cases ofteratoma
A teratoma is a tumor made up of several different types of tissue, such as hair, muscle, teeth, or bone. Teratomata typically form in the ovary, testicle, or coccyx.
Symptoms
Symptoms may be minimal if the tumor is small. A testicular ter ...
which act benign in pre-puberty pediatric individuals along with other benign tumors that have been reported such as: Sertolic cell tumor, Leydig cell tumor and juvenile granulosa cell tumors. Most malignant tumors found in pre-pubertal individuals are pure yolk sac tumors. There is a difference in pre-pubertal, post-pubertal, and adult testis tumors in their histology and their level of malignancy with malignant tumors being rare in the pre-pubertal pediatric population. There has been a consideration to switch to testes sparing surgery (TSS) such as partial orchiectomy specifically for the pre-puberty pediatric populations who lack signs of malignant tumors. Partial orchiectomy allows the ability to preserve hormone function and the possibility of reproduction in the future. It has also been found to increase the quality of life. In the case that an individual is pediatric (<18 years of age) and is a post-pubertal with a malignant testes tumor, they must follow the adult recommended standard guidelines and proceed with radical inguinal orchiectomy.
Post-pubertal populations
The post-pubertal pediatric population and adults are at higher risk of malignant tumors and usually have a histology of a mixed germ cell tumor. Their first line of treatment is radical orchiectomy; however, they may be candidates for testis-sparing surgery such as partial orchiectomy, if there is a presence of a benign tumor. Although partial orchiectomy is controversial for this group of individuals, it has been found to be a successful procedure for benign masses such as stromal tumors, epidermoid cysts, and fibrous pseudotumors. There is greater use of partial orchiectomy with individuals who have small, benign testicular mass usually < 2 cm which indicate the tumors being benign. There is limited data on the size of tumors of the pediatric population, therefore, size cannot be used as a predictor of a tumor being benign.See also
*List of surgeries by type
Many surgical procedure names can be broken into parts to indicate the meaning. For example, in gastrectomy, "ectomy" is a suffix meaning the removal of a part of the body. "Gastro-" means stomach. Thus, ''gastrectomy'' refers to the surgical remo ...
* Index of oncology articles
* Testicular cancer
Testicular cancer is cancer that develops in the testicles, a part of the male reproductive system. Symptoms may include a lump in the testicle, or swelling or pain in the scrotum. Treatment may result in infertility.
Risk factors include a ...
* Androgen replacement therapy
Androgen replacement therapy (ART), often referred to as testosterone replacement therapy (TRT) or hormone replacement therapy (HRT), is a form of hormone therapy in which androgens, often testosterone, are supplemented or replaced exogenously ...
* Androgen deprivation therapy
Androgen deprivation therapy (ADT), also called androgen suppression therapy, is an antihormone therapy whose main use is in treating prostate cancer. Prostate cancer cells usually require androgen hormones, such as testosterone, to grow. ADT red ...
* Vasectomy
Vasectomy, or vasoligation, is an elective surgical procedure for male sterilization or permanent contraception. During the procedure, the male vasa deferentia are cut and tied or sealed so as to prevent sperm from entering into the urethra and ...
* Oophorectomy
Oophorectomy (; from Greek , , 'egg-bearing' and , , 'a cutting out of'), historically also called ''ovariotomy'' is the surgical removal of an ovary or ovaries. The surgery is also called ovariectomy, but this term is mostly used in reference ...
* Gender reassignment therapy
Sex reassignment therapy or medical transition is the medical aspect of gender transition, that is, modifying one's sex characteristics to better suit one's gender identity. It can consist of hormone therapy to alter secondary sex characteris ...
References
{{Authority control Urologic surgery Surgical oncology Male genital surgery Gender-affirming surgery (male-to-female) Testicle