hypertensive nephropathy on:
[Wikipedia]
[Google]
[Amazon]
Hypertensive kidney disease is a medical condition referring to damage to the
 "Hypertensive" refers to high blood pressure and "nephropathy" means damage to the kidney; hence this condition is where chronic high blood pressure causes damages to kidney tissue; this includes the small blood vessels, glomeruli, kidney tubules and interstitial tissues. The tissue hardens and thickens which is known as nephrosclerosis. The narrowing of the blood vessels means less blood is going to the tissue and so less oxygen is reaching the tissue resulting in tissue death (ischemia).
Risk factors for HN include poorly controlled, moderate-to-severe hypertension, older age, other kidney disorders, and Afro-Caribbean background, whose exact cause is unclear, as it may be due to either genetic susceptibility or poor health management among people of Afro-Caribbean descent.
"Hypertensive" refers to high blood pressure and "nephropathy" means damage to the kidney; hence this condition is where chronic high blood pressure causes damages to kidney tissue; this includes the small blood vessels, glomeruli, kidney tubules and interstitial tissues. The tissue hardens and thickens which is known as nephrosclerosis. The narrowing of the blood vessels means less blood is going to the tissue and so less oxygen is reaching the tissue resulting in tissue death (ischemia).
Risk factors for HN include poorly controlled, moderate-to-severe hypertension, older age, other kidney disorders, and Afro-Caribbean background, whose exact cause is unclear, as it may be due to either genetic susceptibility or poor health management among people of Afro-Caribbean descent.
File:Histopathology of hypertensive glomerular lesion of hypertensive nephropathy.jpg, Light micrograph showing hypertensive glomerular lesion of hypertensive nephropathy: global glomerular collapse and filling of Bowman's space with a lightly staining collagenous material.
File:Histopathology of secondary segmental glomerular sclerosis of hypertensive nephropathy.jpg, Light micrograph of glomerulus showing secondary segmental sclerosis of hypertensive nephropathy.
File:Histopathology of arcuate artery nephrosclerosis, annotated.jpg, Histopathology of arcuate artery nephrosclerosis, seen as a thickened intima with an onion skin-like architecture. It is presumably a manifestation of hypertensive kidney disease.
File:Histopathology of renal interstitial fibrosis of hypertensive nephropathy.jpg, Light micrograph showing signs of hypertensive nephropathy: interstitial fibrosis, tubular atrophy with thickened tubular basement membranes, and fibrous intimal thickening of a small artery (arrow).
Malignant nephrosclerosis is where hypertensive nephrosclerosis occurs in presence of
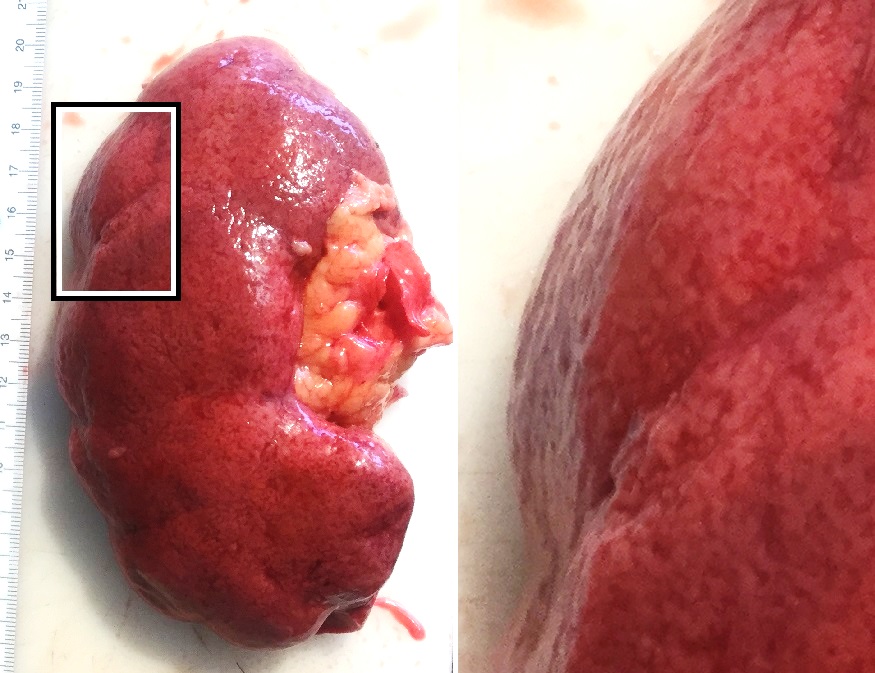
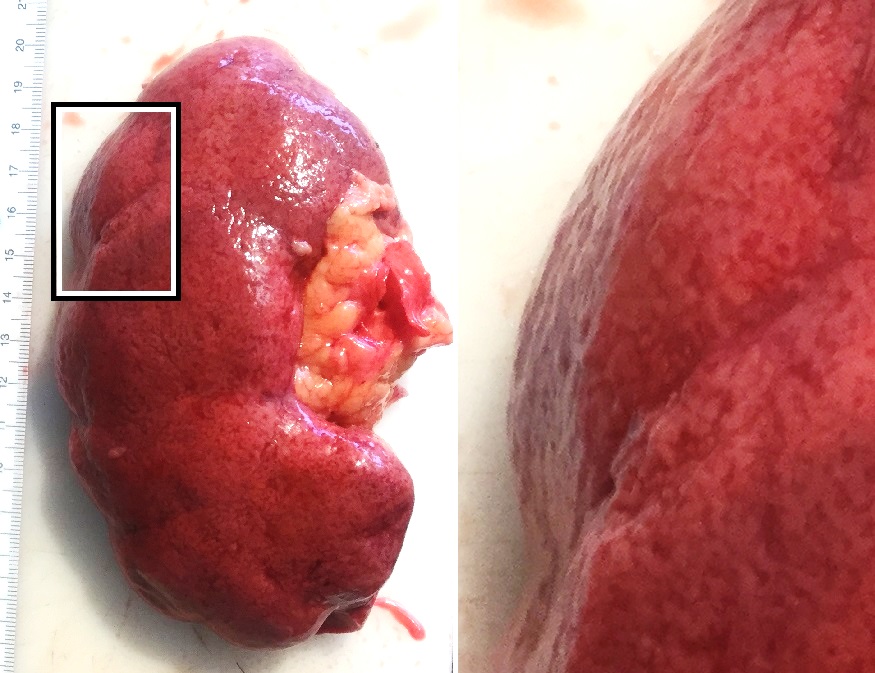
kidney
In humans, the kidneys are two reddish-brown bean-shaped blood-filtering organ (anatomy), organs that are a multilobar, multipapillary form of mammalian kidneys, usually without signs of external lobulation. They are located on the left and rig ...
due to chronic high blood pressure
Hypertension, also known as high blood pressure, is a long-term medical condition in which the blood pressure in the arteries is persistently elevated. High blood pressure usually does not cause symptoms itself. It is, however, a major ri ...
. It manifests as hypertensive nephrosclerosis (sclerosis referring to the stiffening of renal components). It should be distinguished from renovascular hypertension
Renovascular hypertension is a condition in which high blood pressure is caused by the kidneys' hormonal response to narrowing of the renal arteries, arteries supplying the kidneys. When functioning properly this hormonal axis regulates blood pres ...
, which is a form of secondary hypertension
Secondary hypertension (or, less commonly, inessential hypertension) is a type of hypertension which has a specific and identifiable underlying primary cause. It is much less common than essential hypertension, affecting only 5-10% of hypertens ...
, and thus has opposite direction of causation.
Signs and symptoms
Signs and symptoms ofchronic kidney disease
Chronic kidney disease (CKD) is a type of long-term kidney disease, defined by the sustained presence of abnormal kidney function and/or abnormal kidney structure. To meet criteria for CKD, the abnormalities must be present for at least three mo ...
, including loss of appetite, nausea
Nausea is a diffuse sensation of unease and discomfort, sometimes perceived as an urge to vomit. It can be a debilitating symptom if prolonged and has been described as placing discomfort on the chest, abdomen, or back of the throat.
Over 30 d ...
, vomiting
Vomiting (also known as emesis, puking and throwing up) is the forceful expulsion of the contents of one's stomach through the mouth and sometimes the nose.
Vomiting can be the result of ailments like food poisoning, gastroenteritis, pre ...
, itch
An itch (also known as pruritus) is a sensation that causes a strong desire or reflex to scratch. Itches have resisted many attempts to be classified as any one type of sensory experience. Itches have many similarities to pain, and while both ...
ing, sleepiness or confusion, weight loss, and an unpleasant taste in the mouth, may develop.
Causes
 "Hypertensive" refers to high blood pressure and "nephropathy" means damage to the kidney; hence this condition is where chronic high blood pressure causes damages to kidney tissue; this includes the small blood vessels, glomeruli, kidney tubules and interstitial tissues. The tissue hardens and thickens which is known as nephrosclerosis. The narrowing of the blood vessels means less blood is going to the tissue and so less oxygen is reaching the tissue resulting in tissue death (ischemia).
Risk factors for HN include poorly controlled, moderate-to-severe hypertension, older age, other kidney disorders, and Afro-Caribbean background, whose exact cause is unclear, as it may be due to either genetic susceptibility or poor health management among people of Afro-Caribbean descent.
"Hypertensive" refers to high blood pressure and "nephropathy" means damage to the kidney; hence this condition is where chronic high blood pressure causes damages to kidney tissue; this includes the small blood vessels, glomeruli, kidney tubules and interstitial tissues. The tissue hardens and thickens which is known as nephrosclerosis. The narrowing of the blood vessels means less blood is going to the tissue and so less oxygen is reaching the tissue resulting in tissue death (ischemia).
Risk factors for HN include poorly controlled, moderate-to-severe hypertension, older age, other kidney disorders, and Afro-Caribbean background, whose exact cause is unclear, as it may be due to either genetic susceptibility or poor health management among people of Afro-Caribbean descent.
Mechanism
In the kidneys, as a result of ''benign arterial hypertension'',hyaline
A hyaline substance is one with a glassy appearance. The word is derived from , and .
Histopathology
Hyaline cartilage is named after its glassy appearance on fresh gross pathology. On light microscopy of H&E stained slides, the extracellula ...
(pink, amorphous, homogeneous material) accumulates in the walls of small arteries and arterioles, producing the thickening of their walls and the narrowing of the arterial openings, a process known as arteriolosclerosis. The resulting inadequate blood flow produces tubular atrophy, interstitial fibrosis, and glomerular alterations (smaller glomeruli with different degrees of hyalinization – from mild to sclerosis of glomeruli) and scarring around the glomeruli (periglomerular fibrosis). In advanced stages, kidney failure
Kidney failure, also known as renal failure or end-stage renal disease (ESRD), is a medical condition in which the kidneys can no longer adequately filter waste products from the blood, functioning at less than 15% of normal levels. Kidney fa ...
will occur. Functional nephrons have dilated tubules, often with hyaline casts in the opening of the tubules. Additional complications often associated with hypertensive nephropathy include glomerular damage resulting in protein
Proteins are large biomolecules and macromolecules that comprise one or more long chains of amino acid residue (biochemistry), residues. Proteins perform a vast array of functions within organisms, including Enzyme catalysis, catalysing metab ...
and blood in the urine
Hematuria or haematuria is defined as the presence of blood or red blood cells in the urine. "Gross hematuria" occurs when urine appears red, brown, or tea-colored due to the presence of blood. Hematuria may also be subtle and only detectable with ...
.
Hypertensive nephropathy refers to kidney failure that can be attributed to a history of hypertension It is a chronic condition and it is a serious risk factor for the development of end-stage kidney disease (ESKD). However, despite the well-known association between hypertension and chronic kidney disease, the underlying mechanism remains unclear. The two proposed mechanisms of HN's pathophysiology both centre around how the glomerulus, a network of dense capillaries that carries out the kidney filtration process, is affected; with one theory identifying glomerular ischemia as the main contributor to HN and the other identifying glomerular hypertension and glomerular hyperfiltration at the centre of HN's pathogenesis.
Glomerular ischemia
High blood pressure in the long term can damage theendothelium
The endothelium (: endothelia) is a single layer of squamous endothelial cells that line the interior surface of blood vessels and lymphatic vessels. The endothelium forms an interface between circulating blood or lymph in the lumen and the r ...
, commonly known as the blood vessel lining. This leads to a build-up of plaques and they can be deposited in the renal arteries causing stenosis and ischemic kidney disease. In this situation, the kidney supplied blood by the narrowed renal artery suffers from inadequate blood flow, which in turn causes the size of the kidneys to decrease. Other consequences include arterial stiffening, which involves a gradual breakdown of elastic fibers and intima (the innermost layer of a blood vessel) thickening.
Glomerular hypertension and glomerular hyperfiltration
An alternative mechanism of hypertensive nephropathy is prolonged glomerular hypertension and hence glomerular hyperfiltration. These can occur simultaneously but not necessarily. The idea is that hypertension results in sclerosis of the glomeruli which ultimately means reduced kidney function. As a compensatory mechanism, the unaffected nephrons (specifically, the preglomerular arterioles) vasodilate to increase blood flow to the kidney perfusion and increase glomerular filtration across undamaged glomeruli.Diagnosis
Diagnosis of HN is made from clinical history and biochemical investigations. Chronic hypertension with progressive kidney disease progresses over a long period of time. Damage to the glomeruli allows proteins that are usually too large to pass into thenephron
The nephron is the minute or microscopic structural and functional unit of the kidney. It is composed of a renal corpuscle and a renal tubule. The renal corpuscle consists of a tuft of capillaries called a glomerulus and a cup-shaped structu ...
to be filtered. This leads to an elevated concentration of albumin in the urine (albuminuria). This albuminuria usually does not cause symptoms but can be indicative of many kidney disorders. Protein in the urine (proteinuria) is best identified from a 24-hour urine collection.
Bilateral renal artery stenosis should always be considered as a differential diagnosis for the presentation of HN. Kidney disease with this etiology can potentially be reversed following vascular intervention.
Histology
In benign nephrosclerosis, the changes occurring are gradual and progressive, however, there can be sufficient kidney reserve capacity to maintain adequate kidney function for many years. The large renal arteries exhibit intimal thickening, medial hypertrophy, duplication of the elastic layer. The changes in small arterioles include hyaline arteriolosclerosis (deposition ofhyaline
A hyaline substance is one with a glassy appearance. The word is derived from , and .
Histopathology
Hyaline cartilage is named after its glassy appearance on fresh gross pathology. On light microscopy of H&E stained slides, the extracellula ...
, collagenous material), which causes glomerular collapse (wrinkling and thickening of capillary basement membranes and collapse of capillary lumen) and solidification (glomeruli exhibit sclerosis and increase in mesangial matrix). The degree of scarring correlates with the degree of glomerular filtration deficit.
malignant hypertension
A hypertensive emergency is very high blood pressure with potentially life-threatening symptoms and signs of acute damage to one or more organ systems (especially brain, eyes, heart, aorta, or kidneys). It is different from a hypertensive urgenc ...
(when DBP > 130mmHg). Vessels feature intimal thickening, fibrinoid necrosis, red blood cell fragmentation, extravasation, thrombosis
Thrombosis () is the formation of a Thrombus, blood clot inside a blood vessel, obstructing the flow of blood through the circulatory system. When a blood vessel (a vein or an artery) is injured, the body uses platelets (thrombocytes) and fib ...
. These changes create an exaggerated layered appearance (onion skinning).
Urine test
Microalbuminuria (moderate increase in the levels of urinary albumin) is a non-specific finding in patients with vascular disease that is associated with increased risk of cardiovascular events. The majority of patients with benign nephrosclerosis haveproteinuria
Proteinuria is the presence of excess proteins in the urine. In healthy persons, urine contains very little protein, less than 150 mg/day; an excess is suggestive of illness. Excess protein in the urine often causes the urine to become fo ...
in the range from 0.5 to 1 g/ 24hr. In the case of glomerular damage occurring in HN, hematuria
Hematuria or haematuria is defined as the presence of blood or red blood cells in the urine. "Gross hematuria" occurs when urine appears red, brown, or tea-colored due to the presence of blood. Hematuria may also be subtle and only detectable with ...
can occur as well.
Definitive diagnosis
The definitive diagnosis of HN requires morphological examination. Common histological features can be identified in the renal and glomerular vasculature. Glomerulosclerosis is often present, either focally or globally, which is characterized by hardening of the vessel walls. Also, luminal narrowing of the arteries and arterioles of the kidney system. However, this type of procedure is likely to be preceded by a provisional diagnosis based on laboratory investigations.Future diagnostic approaches
Increasing access to, and use of, genome profiling may provide opportunity for diagnosis based on presentation and genetic risk factors, by identifying ApoL1 gene variants on chromosome 22.Management
The aim of the medical treatment is to slow the progression ofchronic kidney disease
Chronic kidney disease (CKD) is a type of long-term kidney disease, defined by the sustained presence of abnormal kidney function and/or abnormal kidney structure. To meet criteria for CKD, the abnormalities must be present for at least three mo ...
by reducing blood pressure and albumin
Albumin is a family of globular proteins, the most common of which are the serum albumins. All of the proteins of the albumin family are water- soluble, moderately soluble in concentrated salt solutions, and experience heat denaturation. Alb ...
levels. The current published guidelines define ideal BP of <130/80 mmHg for patients with hypertensive nephropathy; studies show that anything higher or lower than this can increase cardiovascular risk. According to the African American Study of Kidney Disease (AASK) trial, after an additional 5 years follow-up upon completion of the 10-year trial, up to 65% of the cohort had progressive nephropathy despite having controlled the mean systolic BP level <135 mmHg.
ACE inhibitors
Angiotensin-converting-enzyme inhibitors (ACE inhibitors) are a class of medication used primarily for the treatment of hypertension, high blood pressure and heart failure. This class of medicine works by causing relaxation of blood vessels as ...
, angiotensin receptor blockers
Angiotensin II receptor blockers (ARBs), formally angiotensin II receptor type 1 (AT1) antagonists, also known as angiotensin receptor blockers, angiotensin II receptor antagonists, or AT1 receptor antagonists, are a group of pharmaceuticals tha ...
, direct renin inhibitors and aldosterone antagonists, are pharmacological treatments that can be used to lower BP to target levels; hence reducing neuropathy and proteinuria
Proteinuria is the presence of excess proteins in the urine. In healthy persons, urine contains very little protein, less than 150 mg/day; an excess is suggestive of illness. Excess protein in the urine often causes the urine to become fo ...
progression. The management plan should be individualized based on the condition of the patients including comorbidities and previous medical history.
In addition, there are lifestyle changes that can be made. Weight reduction, exercise, reducing salt intake can be done to manage hypertensive nephropathy.
Prognosis
According to the United States Renal Data System (USRDS), hypertensive nephropathy accounts for more than one-third of patients on hemodialysis and the annual mortality rate for patients on hemodialysis is 23.3%. Haemodialysis is recommended for patients who progress to end-stage kidney disease (ESKD) and hypertensive nephropathy is the second most common cause of ESKD after diabetes. Patient prognosis is dependent on numerous factors including age, ethnicity, blood pressure and glomerular filtration rate. Changes in lifestyle factors, such as reduced salt intake and increased physical activity have been shown to improve outcomes but are insufficient without pharmacological treatment.Epidemiology
The incidence of hypertensive nephropathy varies around the world. For instance, it accounts for as many as 25% and 17% of patients starting dialysis for end-stage kidney disease in Italy and France respectively. Contrastingly, Japan and China report only 6 and 7% respectively. Since the year 2000, nephropathy caused by hypertension has increased in incidence by 8.7% In reality, these figures may be even higher, as hypertension is not always reported as the specific cause of kidney disease. It has been recognized that the incidence of hypertensive nephropathy varies with ethnicity. Compared to Caucasians, African Americans in the USA are much more likely to develop hypertensive nephropathy. Of those who do, the proportion who then go on to develop end-stagekidney failure
Kidney failure, also known as renal failure or end-stage renal disease (ESRD), is a medical condition in which the kidneys can no longer adequately filter waste products from the blood, functioning at less than 15% of normal levels. Kidney fa ...
is 3.5 times higher than in the Caucasian population. In addition to this, African Americans tend to develop hypertensive nephropathy at a younger age than Caucasians (45 to 65, compared to >65).
See also
*Nephropathy
Kidney disease, or renal disease, technically referred to as nephropathy, is damage to or disease of a kidney
In humans, the kidneys are two reddish-brown bean-shaped blood-filtering organ (anatomy), organs that are a multilobar, multipap ...
References
Further reading
* *External links
{{Urologic disease Kidney diseases Hypertension