hemolysis on:
[Wikipedia]
[Google]
[Amazon]

 Hemolysis or haemolysis (), also known by several other names, is the rupturing (
Hemolysis or haemolysis (), also known by several other names, is the rupturing (
 ''
''
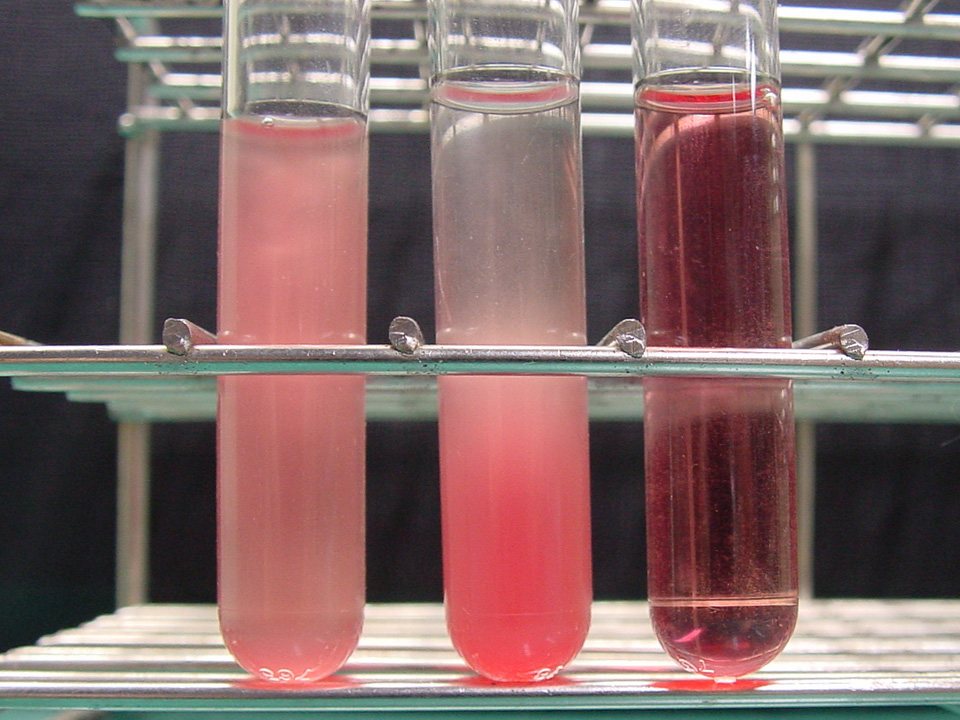
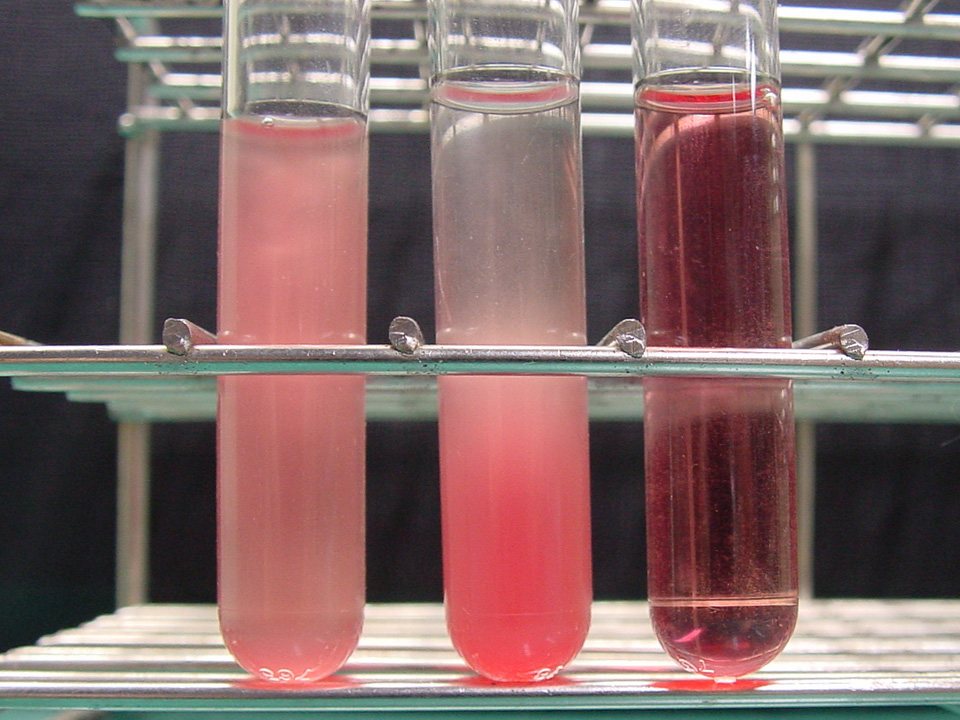
 Visualizing the physical appearance of hemolysis in cultured blood samples may be used as a tool to determine the species of various
Visualizing the physical appearance of hemolysis in cultured blood samples may be used as a tool to determine the species of various
Effects of Hemolysis on Clinical Specimens
{{Authority control Hematology

 Hemolysis or haemolysis (), also known by several other names, is the rupturing (
Hemolysis or haemolysis (), also known by several other names, is the rupturing (lysis
Lysis ( ; from Greek 'loosening') is the breaking down of the membrane of a cell, often by viral, enzymic, or osmotic (that is, "lytic" ) mechanisms that compromise its integrity. A fluid containing the contents of lysed cells is called a ...
) of red blood cell
Red blood cells (RBCs), referred to as erythrocytes (, with -''cyte'' translated as 'cell' in modern usage) in academia and medical publishing, also known as red cells, erythroid cells, and rarely haematids, are the most common type of blood cel ...
s (erythrocytes) and the release of their contents (cytoplasm
The cytoplasm describes all the material within a eukaryotic or prokaryotic cell, enclosed by the cell membrane, including the organelles and excluding the nucleus in eukaryotic cells. The material inside the nucleus of a eukaryotic cell a ...
) into surrounding fluid (e.g. blood plasma
Blood plasma is a light Amber (color), amber-colored liquid component of blood in which blood cells are absent, but which contains Blood protein, proteins and other constituents of whole blood in Suspension (chemistry), suspension. It makes up ...
). Hemolysis may occur in vivo
Studies that are ''in vivo'' (Latin for "within the living"; often not italicized in English) are those in which the effects of various biological entities are tested on whole, living organisms or cells, usually animals, including humans, an ...
or in vitro
''In vitro'' (meaning ''in glass'', or ''in the glass'') Research, studies are performed with Cell (biology), cells or biological molecules outside their normal biological context. Colloquially called "test-tube experiments", these studies in ...
.
One cause of hemolysis is the action of hemolysins, toxins that are produced by certain pathogenic bacteria
Pathogenic bacteria are bacteria that can cause disease. This article focuses on the bacteria that are pathogenic to humans. Most species of bacteria are harmless and many are Probiotic, beneficial but others can cause infectious diseases. The nu ...
or fungi
A fungus (: fungi , , , or ; or funguses) is any member of the group of eukaryotic organisms that includes microorganisms such as yeasts and mold (fungus), molds, as well as the more familiar mushrooms. These organisms are classified as one ...
. Another cause is intense physical exercise. Hemolysins damage the red blood cell's cytoplasmic membrane
The cell membrane (also known as the plasma membrane or cytoplasmic membrane, and historically referred to as the plasmalemma) is a biological membrane that separates and protects the cytoplasm, interior of a Cell (biology), cell from the extrac ...
, causing lysis and eventually cell death.
Etymology
From hemo- + -lysis, fromAncient Greek
Ancient Greek (, ; ) includes the forms of the Greek language used in ancient Greece and the classical antiquity, ancient world from around 1500 BC to 300 BC. It is often roughly divided into the following periods: Mycenaean Greek (), Greek ...
(, 'blood') + , 'loosening').
Inside the body
Hemolysis inside the body can be caused by a large number of medical conditions, including some parasites (''e.g.'', ''Plasmodium
''Plasmodium'' is a genus of unicellular eukaryotes that are obligate parasites of vertebrates and insects. The life cycles of ''Plasmodium'' species involve development in a Hematophagy, blood-feeding insect host (biology), host which then inj ...
''), some autoimmune disorders (''e.g.'', autoimmune haemolytic anaemia, drug-induced hemolytic anemia
Hemolytic anemia or haemolytic anaemia is a form of anemia due to hemolysis, the abnormal breakdown of red blood cells (RBCs), either in the blood vessels (intravascular hemolysis) or elsewhere in the human body (extravascular). This most commonl ...
, atypical hemolytic uremic syndrome (aHUS)), some genetic disorders (''e.g.'', Sickle-cell disease
Sickle cell disease (SCD), also simply called sickle cell, is a group of inherited haemoglobin-related blood disorders. The most common type is known as sickle cell anemia. Sickle cell anemia results in an abnormality in the oxygen-carrying ...
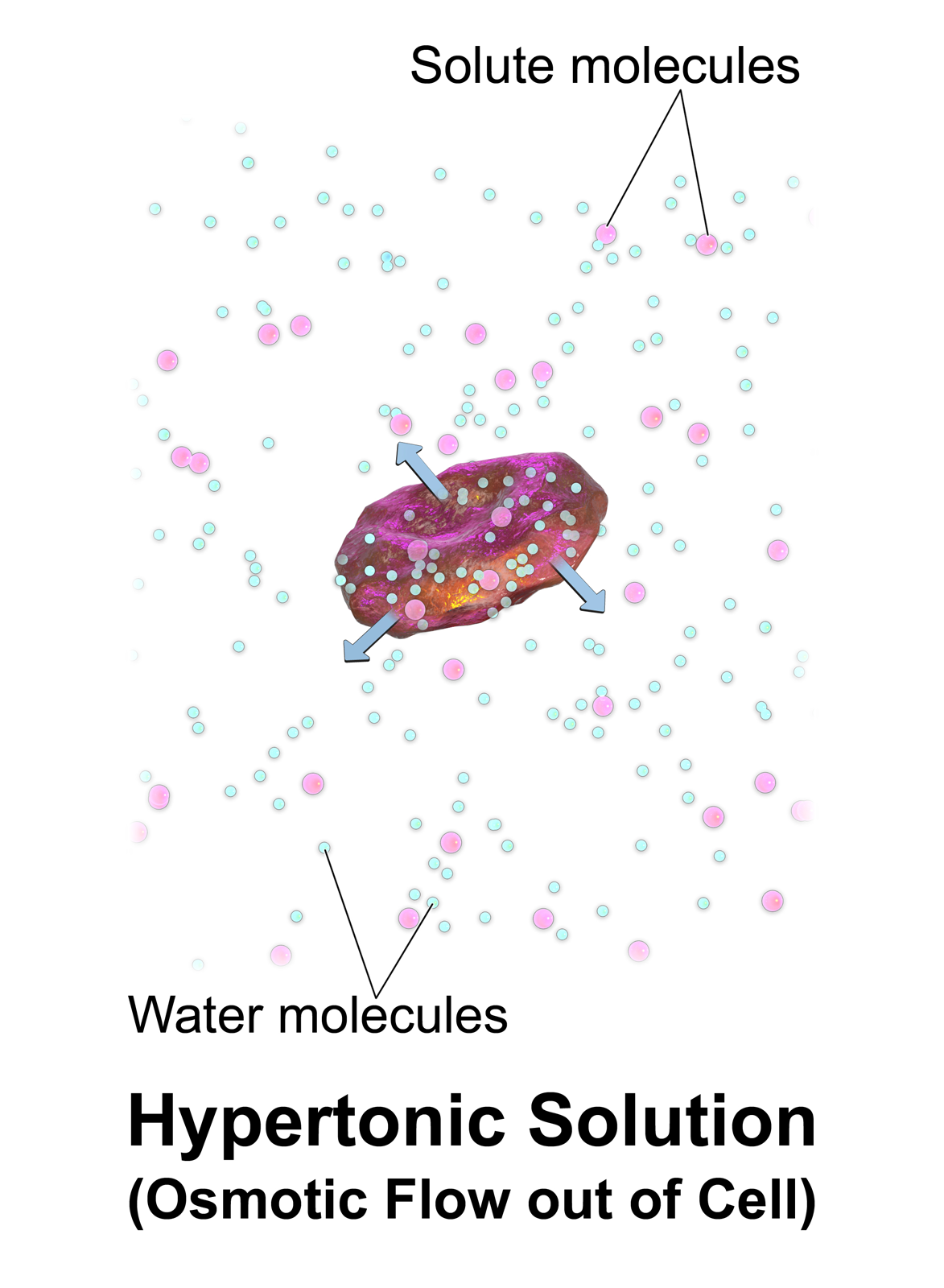
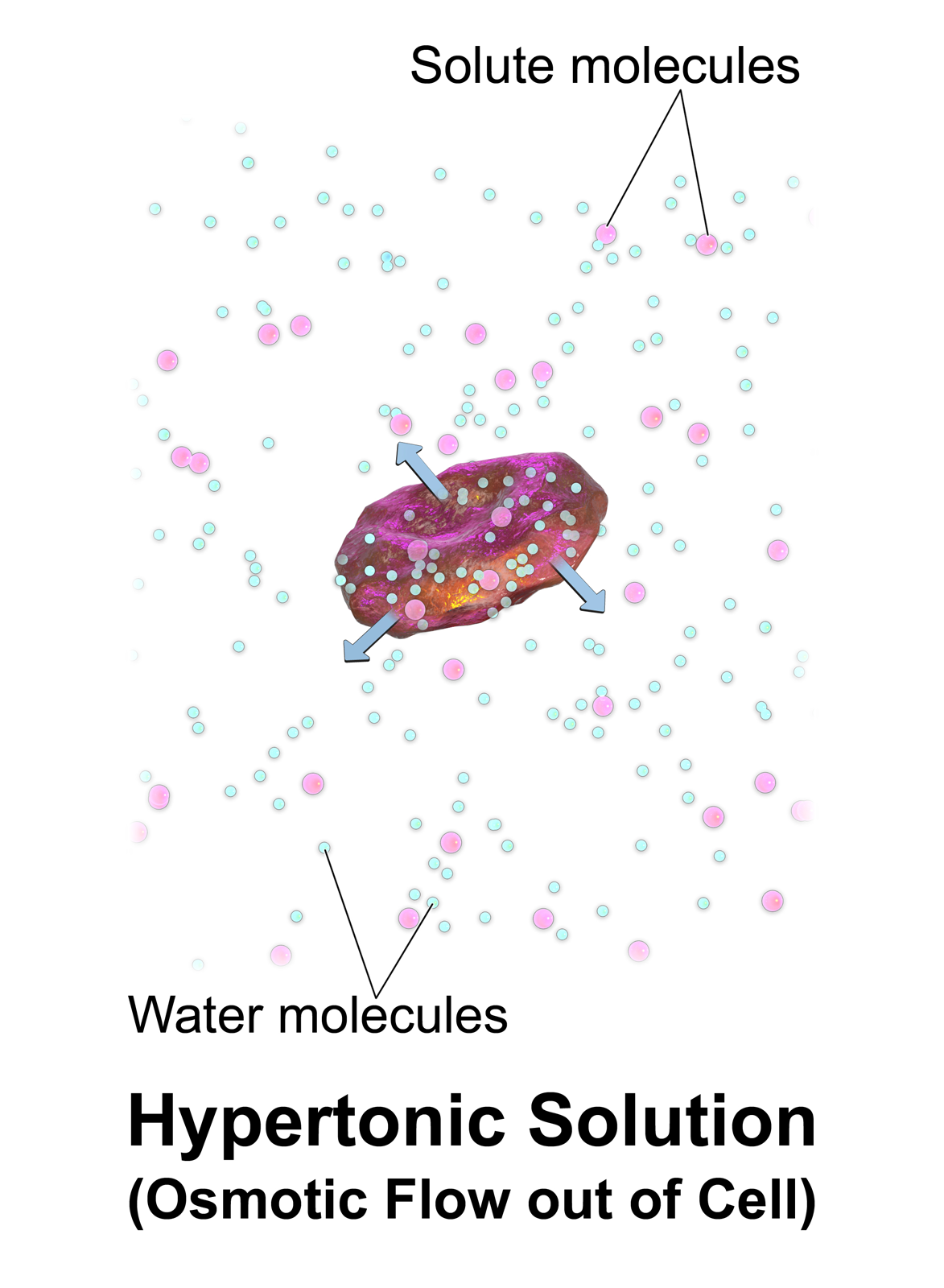
or G6PD deficiency), or blood with too low a solute concentration (hypotonic
In chemical biology, tonicity is a measure of the effective osmotic pressure gradient; the water potential of two solutions separated by a partially-permeable cell membrane. Tonicity depends on the relative concentration of selective memb ...
to cells).
Hemolysis can lead to hemoglobinemia due to hemoglobin
Hemoglobin (haemoglobin, Hb or Hgb) is a protein containing iron that facilitates the transportation of oxygen in red blood cells. Almost all vertebrates contain hemoglobin, with the sole exception of the fish family Channichthyidae. Hemoglobin ...
released into the blood plasma
Blood plasma is a light Amber (color), amber-colored liquid component of blood in which blood cells are absent, but which contains Blood protein, proteins and other constituents of whole blood in Suspension (chemistry), suspension. It makes up ...
, which plays a significant role in the pathogenesis
In pathology, pathogenesis is the process by which a disease or disorder develops. It can include factors which contribute not only to the onset of the disease or disorder, but also to its progression and maintenance. The word comes .
Descript ...
of sepsis
Sepsis is a potentially life-threatening condition that arises when the body's response to infection causes injury to its own tissues and organs.
This initial stage of sepsis is followed by suppression of the immune system. Common signs and s ...
and can lead to increased risk of infection due to its inhibitory effects on the innate immune system
The innate immune system or nonspecific immune system is one of the two main immunity strategies in vertebrates (the other being the adaptive immune system). The innate immune system is an alternate defense strategy and is the dominant immune s ...
.
Parasitic hemolysis
Because the feeding process of the ''Plasmodium
''Plasmodium'' is a genus of unicellular eukaryotes that are obligate parasites of vertebrates and insects. The life cycles of ''Plasmodium'' species involve development in a Hematophagy, blood-feeding insect host (biology), host which then inj ...
'' parasites damages red blood cells, malaria
Malaria is a Mosquito-borne disease, mosquito-borne infectious disease that affects vertebrates and ''Anopheles'' mosquitoes. Human malaria causes Signs and symptoms, symptoms that typically include fever, Fatigue (medical), fatigue, vomitin ...
is sometimes called "parasitic hemolysis" in medical literature.
HELLP, pre-eclampsia, or eclampsia
:See HELLP syndrome,Pre-eclampsia
Pre-eclampsia is a multi-system disorder specific to pregnancy, characterized by the new onset of hypertension, high blood pressure and often a significant amount of proteinuria, protein in the urine or by the new onset of high blood pressure a ...
, and Eclampsia
Eclampsia is the onset of seizures (convulsions) in a pregnant woman with pre-eclampsia. Pre-eclampsia is a hypertensive disorder of pregnancy that presents with three main features: new onset of high blood pressure, large amounts of proteinuria ...
Hemolytic disease of the newborn
Hemolytic disease of the newborn is an autoimmune disease resulting from the mother's antibodies crossing the placenta to the fetus. This most often occurs when the mother has previously been exposed to blood antigens present on the fetus but foreign to her, through either a blood transfusion or a previous pregnancy.Hemolytic anemia
Because ''in vivo'' hemolysis destroys red blood cells, in uncontrolled, chronic or severe cases it can lead tohemolytic anemia
Hemolytic anemia or haemolytic anaemia is a form of anemia due to hemolysis, the abnormal breakdown of red blood cells (RBCs), either in the blood vessels (intravascular hemolysis) or elsewhere in the human body (extravascular). This most commonl ...
.
Hemolytic crisis
A hemolytic crisis, or hyperhemolytic crisis, is characterized by an accelerated rate of red blood cell destruction leading toanemia
Anemia (also spelt anaemia in British English) is a blood disorder in which the blood has a reduced ability to carry oxygen. This can be due to a lower than normal number of red blood cells, a reduction in the amount of hemoglobin availabl ...
, jaundice
Jaundice, also known as icterus, is a yellowish or, less frequently, greenish pigmentation of the skin and sclera due to high bilirubin levels. Jaundice in adults is typically a sign indicating the presence of underlying diseases involving ...
, and reticulocytosis. Hemolytic crises are a major concern with sickle-cell disease
Sickle cell disease (SCD), also simply called sickle cell, is a group of inherited haemoglobin-related blood disorders. The most common type is known as sickle cell anemia. Sickle cell anemia results in an abnormality in the oxygen-carrying ...
and G6PD deficiency.
Toxic agent ingestion or poisoning
''Paxillus involutus
''Paxillus involutus'', also known as the brown roll-rim or the common roll-rim, is a species of basidiomycete fungus. Although it has lamella (mycology), gills, it is more closely related to the pored boletes than to typical gilled mushroom ...
'' ingestion can cause hemolysis.
Space hemolysis
Spaceflight can cause hemolysis.Intrinsic causes
Hemolysis may result from intrinsic defects in the red blood cell itself: * Defects of red blood cell membrane production (as inhereditary spherocytosis
Hereditary spherocytosis (HS) is a congenital hemolytic disorder wherein a genetic genetic mutation, mutation coding for a structural membrane protein phenotype causes the red blood cells to be sphere-shaped (spherocytosis), rather than the norma ...
and hereditary elliptocytosis
Hereditary elliptocytosis, also known as ovalocytosis, is an inherited blood disorder in which an abnormally large number of the person's red blood cells are elliptical rather than the typical biconcave disc shape. Such morphologically distinctiv ...
)
* Defects in hemoglobin production (as in thalassemia
Thalassemias are a group of Genetic disorder, inherited blood disorders that manifest as the production of reduced hemoglobin. Symptoms depend on the type of thalassemia and can vary from none to severe, including death. Often there is mild to ...
, sickle-cell disease
Sickle cell disease (SCD), also simply called sickle cell, is a group of inherited haemoglobin-related blood disorders. The most common type is known as sickle cell anemia. Sickle cell anemia results in an abnormality in the oxygen-carrying ...
and congenital dyserythropoietic anemia
Congenital dyserythropoietic anemia (CDA) is a rare blood disorder, similar to the thalassemias. CDA is one of many types of anemia, characterized by ineffective erythropoiesis, and resulting from a decrease in the number of red blood cells (RBCs) ...
)
* Defective red cell metabolism (as in glucose-6-phosphate dehydrogenase deficiency
Glucose-6-phosphate dehydrogenase deficiency (G6PDD), also known as favism, is the most common enzyme deficiency anemia worldwide. It is an inborn error of metabolism that predisposes to red blood cell breakdown. Most of the time, those who ar ...
and pyruvate kinase deficiency
Pyruvate kinase deficiency is an inherited metabolic disorder of the enzyme pyruvate kinase which affects the survival of red blood cells. Both autosomal dominant and recessive inheritance have been observed with the disorder; classically, and mo ...
)
* Paroxysmal nocturnal hemoglobinuria (PNH), sometimes referred to as Marchiafava-Micheli syndrome, is a rare, acquired, potentially life-threatening disease of the blood characterized by complement-induced intravascular hemolytic anemia.
Extrinsic causes
Extrinsic hemolysis is caused by the red blood cell's environment: * Immune-mediated causes could include transient factors as in '' Mycoplasma pneumoniae'' infection (cold agglutinin disease
Cold agglutinin disease (CAD) is a rare autoimmune disease characterized by the presence of high concentrations of circulating cold sensitive antibodies, usually IgM and autoantibodies that are also active at temperatures below , directed again ...
) or permanent factors as in autoimmune disease
An autoimmune disease is a condition that results from an anomalous response of the adaptive immune system, wherein it mistakenly targets and attacks healthy, functioning parts of the body as if they were foreign organisms. It is estimated tha ...
s like autoimmune hemolytic anemia
Autoimmune hemolytic anemia (AIHA) occurs when a person's immune system produces antibodies directed against their own red blood cells (RBCs). These antibodies attach to red cells, causing them to break down ( lyse), and reducing the number of ox ...
(itself more common in diseases such as systemic lupus erythematosus
Lupus, formally called systemic lupus erythematosus (SLE), is an autoimmune disease in which the body's immune system mistakenly attacks healthy tissue in many parts of the body. Symptoms vary among people and may be mild to severe. Common ...
, rheumatoid arthritis
Rheumatoid arthritis (RA) is a long-term autoimmune disorder that primarily affects synovial joint, joints. It typically results in warm, swollen, and painful joints. Pain and stiffness often worsen following rest. Most commonly, the wrist and h ...
, Hodgkin's lymphoma
Hodgkin lymphoma (HL) is a type of lymphoma in which cancer originates from a specific type of white blood cell called lymphocytes, where multinucleated Reed–Sternberg cells (RS cells) are present in the lymph nodes. The condition was named a ...
, and chronic lymphocytic leukemia
Chronic lymphocytic leukemia (CLL) is a type of cancer that affects the blood and bone marrow. In CLL, the bone marrow makes too many lymphocytes, which are a type of white blood cell. In patients with CLL, B cell lymphocytes can begin to colle ...
).
* Spur cell hemolytic anemia
* Any of the causes of hypersplenism
Splenomegaly is an enlargement of the spleen. The spleen usually lies in the left upper quadrant (LUQ) of the human abdomen. Splenomegaly is one of the four cardinal signs of ''hypersplenism'' which include: some reduction in number of circulatin ...
(increased activity of the spleen), such as portal hypertension
Portal hypertension is defined as increased portal venous pressure, with a hepatic venous pressure gradient greater than 5 mmHg. Normal portal pressure is 1–4 mmHg; clinically insignificant portal hypertension is present at portal pressures 5� ...
.
* Acquired hemolytic anemia is also encountered in burn
A burn is an injury to skin, or other tissues, caused by heat, electricity, chemicals, friction, or ionizing radiation (such as sunburn, caused by ultraviolet radiation). Most burns are due to heat from hot fluids (called scalding), soli ...
s and as a result of certain infections (e.g. malaria
Malaria is a Mosquito-borne disease, mosquito-borne infectious disease that affects vertebrates and ''Anopheles'' mosquitoes. Human malaria causes Signs and symptoms, symptoms that typically include fever, Fatigue (medical), fatigue, vomitin ...
).
* Lead poisoning
Lead poisoning, also known as plumbism and saturnism, is a type of metal poisoning caused by lead in the body. Symptoms may include abdominal pain, constipation, headaches, irritability, memory problems, infertility, numbness and paresthesia, t ...
or poisoning by arsine
Arsine (IUPAC name: arsane) is an inorganic compound with the formula As H3. This flammable, pyrophoric, and highly toxic pnictogen hydride gas is one of the simplest compounds of arsenic. Despite its lethality, it finds some applications in th ...
or stibine causes non-immune hemolytic anemia.
* Runners can develop hemolytic anemia due to " footstrike hemolysis", the destruction of red blood cells in feet at foot impact.
* Low-grade hemolytic anemia occurs in 70% of prosthetic heart valve recipients, and severe hemolytic anemia occurs in 3%.
Intravascular hemolysis
Intravascular hemolysis describes hemolysis that happens mainly inside thevasculature
In vertebrates, the circulatory system is a system of organs that includes the heart, blood vessels, and blood which is circulated throughout the body. It includes the cardiovascular system, or vascular system, that consists of the heart an ...
. As a result, the contents of the red blood cell are released into the general circulation, leading to hemoglobinemia and increasing the risk of ensuing hyperbilirubinemia.
Intravascular hemolysis may occur when red blood cells are targeted by autoantibodies
An autoantibody is an antibody (a type of protein) produced by the immune system that is directed against one or more of the individual's own proteins. Many autoimmune diseases (notably lupus erythematosus) are associated with such antibodies.
Pr ...
, leading to complement fixation, or by damage by parasites such as ''Babesia
''Babesia'', also called ''Nuttallia'', is an apicomplexan parasite that infects red blood cells and is transmitted by ticks. Originally discovered by Romanian bacteriologist Victor Babeș in 1888; over 100 species of ''Babesia'' have since ...
''. Additionally, thrombotic microangiopathy (TMA) can result in hemolysis of red blood cells. TMA is frequently observed in aHUS patients where clots form in the small vessels of the kidney resulting in damaged red blood cells as they attempt to pass through the restricted vessels.
Extravascular hemolysis
Extravascular hemolysis refers to hemolysis taking place in theliver
The liver is a major metabolic organ (anatomy), organ exclusively found in vertebrates, which performs many essential biological Function (biology), functions such as detoxification of the organism, and the Protein biosynthesis, synthesis of var ...
, spleen
The spleen (, from Ancient Greek '' σπλήν'', splḗn) is an organ (biology), organ found in almost all vertebrates. Similar in structure to a large lymph node, it acts primarily as a blood filter.
The spleen plays important roles in reg ...
, bone marrow
Bone marrow is a semi-solid biological tissue, tissue found within the Spongy bone, spongy (also known as cancellous) portions of bones. In birds and mammals, bone marrow is the primary site of new blood cell production (or haematopoiesis). It i ...
, and lymph nodes
A lymph node, or lymph gland, is a kidney-shaped Organ (anatomy), organ of the lymphatic system and the adaptive immune system. A large number of lymph nodes are linked throughout the body by the lymphatic vessels. They are major sites of lymphoc ...
. In this case little hemoglobin escapes into blood plasma
Blood plasma is a light Amber (color), amber-colored liquid component of blood in which blood cells are absent, but which contains Blood protein, proteins and other constituents of whole blood in Suspension (chemistry), suspension. It makes up ...
. The macrophages
Macrophages (; abbreviated MPhi, φ, MΦ or MP) are a type of white blood cell of the innate immune system that engulf and digest pathogens, such as cancer cells, microbes, cellular debris and foreign substances, which do not have proteins that ...
of the reticuloendothelial system
In anatomy the term reticuloendothelial system (abbreviated RES), often associated nowadays with the mononuclear phagocyte system (MPS), was employed by the beginning of the 20th century to denote a system of specialised cells that effectively cl ...
in these organs engulf and destroy structurally-defective red blood cells, or those with antibodies attached, and release unconjugated bilirubin into the blood plasma circulation. Typically, the spleen destroys mildly abnormal red blood cells or those coated with IgG-type antibodies, while severely abnormal red blood cells or those coated with IgM-type antibodies are destroyed in the circulation or in the liver.
If extravascular hemolysis is extensive, hemosiderin
Hemosiderin image of a kidney viewed under a microscope. The brown areas represent hemosiderin
Hemosiderin or haemosiderin is an iron-storage complex that is composed of partially digested ferritin and lysosomes. The breakdown of heme gives ri ...
can be deposited in the spleen, bone marrow, kidney, liver, and other organs, resulting in hemosiderosis.
Outside the body
 ''
''In vitro
''In vitro'' (meaning ''in glass'', or ''in the glass'') Research, studies are performed with Cell (biology), cells or biological molecules outside their normal biological context. Colloquially called "test-tube experiments", these studies in ...
'' hemolysis can be caused by improper technique during collection of blood specimens, by the effects of mechanical processing of blood, or by bacterial action in cultured blood specimens.
From specimen collection
Most causes of ''in vitro'' hemolysis are related to specimen collection. Difficult collections, unsecure line connections, contamination, and incorrect needle size, as well as improper tube mixing and incorrectly filled tubes are all frequent causes of hemolysis. ''In vitro'' hemolysis during specimen collection can cause inaccurate laboratory test results by contaminating the surrounding plasma with the contents of hemolyzed red blood cells. For example, the concentration ofpotassium
Potassium is a chemical element; it has Symbol (chemistry), symbol K (from Neo-Latin ) and atomic number19. It is a silvery white metal that is soft enough to easily cut with a knife. Potassium metal reacts rapidly with atmospheric oxygen to ...
inside red blood cells is much higher than in the plasma and so an elevated potassium level is usually found in biochemistry tests of hemolyzed blood.
After the blood collection process, ''in vitro'' hemolysis can still occur in a sample due to external factors, such as prolonged storage, incorrect storage conditions and excessive physical forces by dropping or vigorously mixing the tube.
From mechanical blood processing during surgery
In some surgical procedures (especially some heart operations) where substantial blood loss is expected, machinery is used for intraoperative blood salvage. A centrifuge process takes blood from the patient, washes the red blood cells withnormal saline
Saline (also known as saline solution) is a mixture of sodium chloride (salt) and water. It has a number of uses in medicine including cleaning wounds, removal and storage of contact lenses, and help with dry eyes. By intravenous therapy, inje ...
, and returns them to the patient's blood circulation. Hemolysis may occur if the centrifuge rotates too quickly (generally greater than 500 rpm)—essentially this is hemolysis occurring outside of the body. Increased hemolysis occurs with massive amounts of sudden blood loss, because the process of returning a patient's cells must be done at a correspondingly higher speed to prevent hypotension
Hypotension, also known as low blood pressure, is a cardiovascular condition characterized by abnormally reduced blood pressure. Blood pressure is the force of blood pushing against the walls of the arteries as the heart pumps out blood and is ...
, pH imbalance, and a number of other hemodynamic and blood level factors. Modeling of fluid flows to predict the likelihood of red cell membrane rupture in response to stress is an active area of research.
From bacteria culture
 Visualizing the physical appearance of hemolysis in cultured blood samples may be used as a tool to determine the species of various
Visualizing the physical appearance of hemolysis in cultured blood samples may be used as a tool to determine the species of various Gram-positive bacteria
In bacteriology, gram-positive bacteria are bacteria that give a positive result in the Gram stain test, which is traditionally used to quickly classify bacteria into two broad categories according to their type of cell wall.
The Gram stain ...
infections (''e.g.'', ''Streptococcus
''Streptococcus'' is a genus of gram-positive spherical bacteria that belongs to the family Streptococcaceae, within the order Lactobacillales (lactic acid bacteria), in the phylum Bacillota. Cell division in streptococci occurs along a sing ...
'').
Nomenclature
Hemolysis is sometimes called hematolysis, erythrolysis, or erythrocytolysis. The words ''hemolysis'' () and ''hematolysis'' () both use combining forms conveying the idea of "lysis
Lysis ( ; from Greek 'loosening') is the breaking down of the membrane of a cell, often by viral, enzymic, or osmotic (that is, "lytic" ) mechanisms that compromise its integrity. A fluid containing the contents of lysed cells is called a ...
of blood" ('' hemo-'' or '' hemato-'' + '' -lysis''). The words ''erythrolysis'' () and ''erythrocytolysis'' () both use combining forms conveying the idea of "lysis
Lysis ( ; from Greek 'loosening') is the breaking down of the membrane of a cell, often by viral, enzymic, or osmotic (that is, "lytic" ) mechanisms that compromise its integrity. A fluid containing the contents of lysed cells is called a ...
of erythrocytes" ('' erythro-'' ± '' cyto-'' + '' -lysis'').
Red blood cells (erythrocytes) have a short lifespan (approximately 120 days), and old ( senescent) cells are constantly removed and replaced with new ones via erythropoiesis
Erythropoiesis (from Greek ''erythro'', meaning ''red'' and ''poiesis'', meaning ''to make'') is the process which produces red blood cells (erythrocytes), which is the development from erythropoietic stem cell to mature red blood cell.
It is s ...
. This breakdown/replacement process is called erythrocyte turnover. In this sense, erythrolysis or hemolysis is a normal process that happens continually. However, these terms are usually used to indicate that the lysis is pathological
Pathology is the study of disease. The word ''pathology'' also refers to the study of disease in general, incorporating a wide range of biology research fields and medical practices. However, when used in the context of modern medical treatme ...
.
Complications
Pulmonary hypertension has been gaining recognition as a complication of chronic hereditary and acquired hemolysis. Free hemoglobin released during hemolysis inactivates thevasodilator
Vasodilation, also known as vasorelaxation, is the widening of blood vessels. It results from relaxation of smooth muscle cells within the vessel walls, in particular in the large veins, large arteries, and smaller arterioles. Blood vessel wal ...
nitric oxide (NO). Hemolysis also releases arginase that depletes L-arginine
Arginine is the amino acid with the formula (H2N)(HN)CN(H)(CH2)3CH(NH2)CO2H. The molecule features a guanidino group appended to a standard amino acid framework. At physiological pH, the carboxylic acid is deprotonated (−CO2−) and both the ...
, the substrate needed for NO synthesis. This reduces NO-dependent vasodilation and induces platelet
Platelets or thrombocytes () are a part of blood whose function (along with the coagulation#Coagulation factors, coagulation factors) is to react to bleeding from blood vessel injury by clumping to form a thrombus, blood clot. Platelets have no ...
activation, thrombin
Prothrombin (coagulation factor II) is encoded in the human by the F2-gene. It is proteolytically cleaved during the clotting process by the prothrombinase enzyme complex to form thrombin.
Thrombin (Factor IIa) (, fibrose, thrombase, throm ...
generation, procoagulant factors and tissue factor
Tissue factor, also called platelet tissue factor or Coagulation factor III, is a protein present in subendothelial tissue and leukocytes which plays a major role in coagulation and, in humans, is encoded by ''F3'' gene. Its role in the blood c ...
activation, contributing to the formation of thrombosis
Thrombosis () is the formation of a Thrombus, blood clot inside a blood vessel, obstructing the flow of blood through the circulatory system. When a blood vessel (a vein or an artery) is injured, the body uses platelets (thrombocytes) and fib ...
. This can lead to esophageal spasm
Esophageal spasm is a disorder of motility of the esophagus.
There are two types of esophageal spasm:
* Diffuse or distal esophageal spasm (DES), where there is uncoordinated esophageal contractions
* Nutcracker esophagus (NE) also known as hyp ...
and dysphagia
Dysphagia is difficulty in swallowing. Although classified under " symptoms and signs" in ICD-10, in some contexts it is classified as a condition in its own right.
It may be a sensation that suggests difficulty in the passage of solids or l ...
, abdominal pain
Abdominal pain, also known as a stomach ache, is a symptom associated with both non-serious and serious medical issues. Since the abdomen contains most of the body's vital organs, it can be an indicator of a wide variety of diseases. Given th ...
, erectile dysfunction
Erectile dysfunction (ED), also referred to as impotence, is a form of sexual dysfunction in males characterized by the persistent or recurring inability to achieve or maintain a Human penis, penile erection with sufficient rigidity and durat ...
, systemic hypertension, decreased organ perfusion, promotion of inflammation
Inflammation (from ) is part of the biological response of body tissues to harmful stimuli, such as pathogens, damaged cells, or irritants. The five cardinal signs are heat, pain, redness, swelling, and loss of function (Latin ''calor'', '' ...
and coagulation
Coagulation, also known as clotting, is the process by which blood changes from a liquid to a gel, forming a thrombus, blood clot. It results in hemostasis, the cessation of blood loss from a damaged vessel, followed by repair. The process of co ...
, and thrombosis
Thrombosis () is the formation of a Thrombus, blood clot inside a blood vessel, obstructing the flow of blood through the circulatory system. When a blood vessel (a vein or an artery) is injured, the body uses platelets (thrombocytes) and fib ...
.
Chronic hemolysis may also lead to endothelial dysfunction
In blood vessel diseases, endothelial dysfunction is an unhealthy state of the the cells that line the blood vessels (endothelium). The main cause of endothelial dysfunction is impaired bioavailability of nitric oxide.
In addition to acting a ...
, heightened endothelin-1-mediated responses and vasculopathy. The release of heme
Heme (American English), or haem (Commonwealth English, both pronounced /Help:IPA/English, hi:m/ ), is a ring-shaped iron-containing molecule that commonly serves as a Ligand (biochemistry), ligand of various proteins, more notably as a Prostheti ...
leads to the production of bilirubin
Bilirubin (BR) (adopted from German, originally bili—bile—plus ruber—red—from Latin) is a red-orange compound that occurs in the normcomponent of the straw-yellow color in urine. Another breakdown product, stercobilin, causes the brown ...
and depletion of plasma proteins, such as albumin
Albumin is a family of globular proteins, the most common of which are the serum albumins. All of the proteins of the albumin family are water- soluble, moderately soluble in concentrated salt solutions, and experience heat denaturation. Alb ...
, haptoglobin, and hemopexin, which may lead to jaundice
Jaundice, also known as icterus, is a yellowish or, less frequently, greenish pigmentation of the skin and sclera due to high bilirubin levels. Jaundice in adults is typically a sign indicating the presence of underlying diseases involving ...
. Material was copied from this source, which is available under a Creative Commons License. It may also lead to increased levels of the heme breakdown product stercobilin
Stercobilin is a tetrapyrrolic bile pigment and is one end-product of heme catabolism. It is the chemical responsible for the brown color of human feces and was originally isolated from feces in 1932. Stercobilin (and related urobilin) can be ...
in the stool.
Splenectomy
A splenectomy is the surgical procedure that partially or completely removes the spleen. The spleen is an important organ in regard to immunological function due to its ability to efficiently destroy encapsulated bacteria. Therefore, removal of ...
of those with hemolytic disorders appears to increase risk of developing pulmonary thrombosis.
Complications may also arise from the increased workload for the kidney as it secretes erythropoietin
Erythropoietin (; EPO), also known as erythropoetin, haematopoietin, or haemopoietin, is a glycoprotein cytokine secreted mainly by the kidneys in response to cellular hypoxia; it stimulates red blood cell production ( erythropoiesis) in th ...
to stimulate the bone marrow
Bone marrow is a semi-solid biological tissue, tissue found within the Spongy bone, spongy (also known as cancellous) portions of bones. In birds and mammals, bone marrow is the primary site of new blood cell production (or haematopoiesis). It i ...
to produce more reticulocyte
In hematology, reticulocytes are immature red blood cells (RBCs). In the process of erythropoiesis (red blood cell formation), reticulocytes develop and mature in the bone marrow and then circulate for about a day in the blood stream before dev ...
s (red blood cell precursors) to compensate for the loss of red blood cells due to hemolysis.
References
External links
Effects of Hemolysis on Clinical Specimens
{{Authority control Hematology