Blood Transfusion on:
[Wikipedia]
[Google]
[Amazon]
Blood transfusion is the process of transferring


 Historically, red blood cell transfusion was considered when the hemoglobin level fell below 100g/L or
Historically, red blood cell transfusion was considered when the hemoglobin level fell below 100g/L or
 Before a blood transfusion is given, there are many steps taken to ensure quality of the blood products, compatibility, and safety to the recipient. In 2012, a national blood policy was in place in 70% of countries and 69% of countries had specific legislation that covers the safety and quality of blood transfusion.
Before a blood transfusion is given, there are many steps taken to ensure quality of the blood products, compatibility, and safety to the recipient. In 2012, a national blood policy was in place in 70% of countries and 69% of countries had specific legislation that covers the safety and quality of blood transfusion.
 Donated blood is usually subjected to processing after it is collected, to make it suitable for use in specific patient populations. Collected blood is then separated into blood components by centrifugation:
Donated blood is usually subjected to processing after it is collected, to make it suitable for use in specific patient populations. Collected blood is then separated into blood components by centrifugation:
 Before a recipient receives a transfusion, compatibility testing between donor and recipient blood must be done. The first step before a transfusion is given is to type and screen the recipient's blood. Typing of recipient's blood determines the ABO and Rh status. The sample is then screened for any alloantibodies that may react with donor blood.Blood Processing.
Before a recipient receives a transfusion, compatibility testing between donor and recipient blood must be done. The first step before a transfusion is given is to type and screen the recipient's blood. Typing of recipient's blood determines the ABO and Rh status. The sample is then screened for any alloantibodies that may react with donor blood.Blood Processing.
http://library.med.utah.edu/WebPath/TUTORIAL/BLDBANK/BBPROC.html
Accessed on: December 15, 2006. It takes about 45 minutes to complete (depending on the method used). The blood bank scientist also checks for special requirements of the patient (e.g. need for washed, irradiated or CMV negative blood) and the history of the patient to see if they have previously identified antibodies and any other serological anomalies. A positive screen warrants an antibody panel/investigation to determine if it is clinically significant. An antibody panel consists of commercially prepared group O red cell suspensions from donors that have been phenotyped for antigens that correspond to commonly encountered and clinically significant alloantibodies. Donor cells may have homozygous (e.g. K+k+), heterozygous (K+k-) expression or no expression of various antigens (K−k−). The phenotypes of all the donor cells being tested are shown in a chart. The patient's serum is tested against the various donor cells. Based on the reactions of the patient's serum against the donor cells, a pattern will emerge to confirm the presence of one or more antibodies. Not all antibodies are clinically significant (i.e. cause transfusion reactions, HDN, etc.). Once the patient has developed a clinically significant antibody it is vital that the patient receive antigen-negative red blood cells to prevent future transfusion reactions. A direct antiglobulin test ( Coombs test) is also performed as part of the antibody investigation.
If there is no antibody present, an immediate spin crossmatch or computer-assisted crossmatch is performed where the recipient serum and donor rbc are incubated. In the immediate spin method, two drops of patient serum are tested against a drop of 3–5% suspension of donor cells in a test tube and spun in a serofuge. Agglutination or hemolysis (i.e., positive Coombs test) in the test tube is a positive reaction and the unit should not be transfused.
If an antibody is suspected, potential donor units must first be screened for the corresponding antigen by phenotyping them. Antigen negative units are then tested against the patient plasma using an antiglobulin/indirect crossmatch technique at 37 degrees Celsius to enhance reactivity and make the test easier to read.
In urgent cases where crossmatching cannot be completed, and the risk of dropping hemoglobin outweighs the risk of transfusing uncrossmatched blood, O-negative blood is used, followed by crossmatch as soon as possible. O-negative is also used for children and women of childbearing age. It is preferable for the laboratory to obtain a pre-transfusion sample in these cases so a type and screen can be performed to determine the actual blood group of the patient and to check for alloantibodies.
A positive screen warrants an antibody panel/investigation to determine if it is clinically significant. An antibody panel consists of commercially prepared group O red cell suspensions from donors that have been phenotyped for antigens that correspond to commonly encountered and clinically significant alloantibodies. Donor cells may have homozygous (e.g. K+k+), heterozygous (K+k-) expression or no expression of various antigens (K−k−). The phenotypes of all the donor cells being tested are shown in a chart. The patient's serum is tested against the various donor cells. Based on the reactions of the patient's serum against the donor cells, a pattern will emerge to confirm the presence of one or more antibodies. Not all antibodies are clinically significant (i.e. cause transfusion reactions, HDN, etc.). Once the patient has developed a clinically significant antibody it is vital that the patient receive antigen-negative red blood cells to prevent future transfusion reactions. A direct antiglobulin test ( Coombs test) is also performed as part of the antibody investigation.
If there is no antibody present, an immediate spin crossmatch or computer-assisted crossmatch is performed where the recipient serum and donor rbc are incubated. In the immediate spin method, two drops of patient serum are tested against a drop of 3–5% suspension of donor cells in a test tube and spun in a serofuge. Agglutination or hemolysis (i.e., positive Coombs test) in the test tube is a positive reaction and the unit should not be transfused.
If an antibody is suspected, potential donor units must first be screened for the corresponding antigen by phenotyping them. Antigen negative units are then tested against the patient plasma using an antiglobulin/indirect crossmatch technique at 37 degrees Celsius to enhance reactivity and make the test easier to read.
In urgent cases where crossmatching cannot be completed, and the risk of dropping hemoglobin outweighs the risk of transfusing uncrossmatched blood, O-negative blood is used, followed by crossmatch as soon as possible. O-negative is also used for children and women of childbearing age. It is preferable for the laboratory to obtain a pre-transfusion sample in these cases so a type and screen can be performed to determine the actual blood group of the patient and to check for alloantibodies.
 Working at the Royal Society in the 1660s, the physician Richard Lower began examining the effects of changes in blood volume on circulatory function and developed methods for cross-circulatory study in animals, obviating clotting by closed arteriovenous connections. The new instruments he was able to devise enabled him to perform the first reliably documented successful transfusion of blood in front of his distinguished colleagues from the Royal Society.
According to Lower's account, "...towards the end of February 1665 selected one dog of medium size, opened its jugular vein, and drew off blood, until its strength was nearly gone. Then, to make up for the great loss of this dog by the blood of a second, I introduced blood from the cervical artery of a fairly large mastiff, which had been fastened alongside the first, until this latter animal showed ... it was overfilled ... by the inflowing blood." After he "sewed up the jugular veins", the animal recovered "with no sign of discomfort or of displeasure".
Lower had performed the first blood transfusion between animals. He was then "requested by the Honorable obertBoyle ... to acquaint the Royal Society with the procedure for the whole experiment", which he did in December 1665 in the Society's '' Philosophical Transactions''.
The first blood transfusion from animal to human was administered by Dr. Jean-Baptiste Denys, eminent physician to King Louis XIV of France, on June 15, 1667. He transfused the blood of a sheep into a 15-year-old boy, who survived the transfusion. Denys performed another transfusion into a labourer, who also survived. Both instances were likely due to the small amount of blood that was actually transfused into these people. This allowed them to withstand the allergic reaction.
Denys's third patient to undergo a blood transfusion was Swedish Baron Gustaf Bonde. He received two transfusions. After the second transfusion Bonde died. In the winter of 1667, Denys performed several transfusions on Antoine Mauroy with calf's blood. On the third account Mauroy died.
Six months later in London, Lower performed the first human transfusion of animal blood in Britain, where he "superintended the introduction in patient'sarm at various times of some ounces of sheep's blood at a meeting of the Royal Society, and without any inconvenience to him." The recipient was Arthur Coga, "the subject of a harmless form of insanity." Sheep's blood was used because of speculation about the value of blood exchange between species; it had been suggested that blood from a gentle lamb might quiet the tempestuous spirit of an agitated person and that the shy might be made outgoing by blood from more sociable creatures. Coga received 20 shillings () to participate in the experiment.
Lower went on to pioneer new devices for the precise control of blood flow and the transfusion of blood; his designs were substantially the same as modern syringes and
Working at the Royal Society in the 1660s, the physician Richard Lower began examining the effects of changes in blood volume on circulatory function and developed methods for cross-circulatory study in animals, obviating clotting by closed arteriovenous connections. The new instruments he was able to devise enabled him to perform the first reliably documented successful transfusion of blood in front of his distinguished colleagues from the Royal Society.
According to Lower's account, "...towards the end of February 1665 selected one dog of medium size, opened its jugular vein, and drew off blood, until its strength was nearly gone. Then, to make up for the great loss of this dog by the blood of a second, I introduced blood from the cervical artery of a fairly large mastiff, which had been fastened alongside the first, until this latter animal showed ... it was overfilled ... by the inflowing blood." After he "sewed up the jugular veins", the animal recovered "with no sign of discomfort or of displeasure".
Lower had performed the first blood transfusion between animals. He was then "requested by the Honorable obertBoyle ... to acquaint the Royal Society with the procedure for the whole experiment", which he did in December 1665 in the Society's '' Philosophical Transactions''.
The first blood transfusion from animal to human was administered by Dr. Jean-Baptiste Denys, eminent physician to King Louis XIV of France, on June 15, 1667. He transfused the blood of a sheep into a 15-year-old boy, who survived the transfusion. Denys performed another transfusion into a labourer, who also survived. Both instances were likely due to the small amount of blood that was actually transfused into these people. This allowed them to withstand the allergic reaction.
Denys's third patient to undergo a blood transfusion was Swedish Baron Gustaf Bonde. He received two transfusions. After the second transfusion Bonde died. In the winter of 1667, Denys performed several transfusions on Antoine Mauroy with calf's blood. On the third account Mauroy died.
Six months later in London, Lower performed the first human transfusion of animal blood in Britain, where he "superintended the introduction in patient'sarm at various times of some ounces of sheep's blood at a meeting of the Royal Society, and without any inconvenience to him." The recipient was Arthur Coga, "the subject of a harmless form of insanity." Sheep's blood was used because of speculation about the value of blood exchange between species; it had been suggested that blood from a gentle lamb might quiet the tempestuous spirit of an agitated person and that the shy might be made outgoing by blood from more sociable creatures. Coga received 20 shillings () to participate in the experiment.
Lower went on to pioneer new devices for the precise control of blood flow and the transfusion of blood; his designs were substantially the same as modern syringes and
 The science of blood transfusion dates to the first decade of the 20th century, with the discovery of distinct
The science of blood transfusion dates to the first decade of the 20th century, with the discovery of distinct
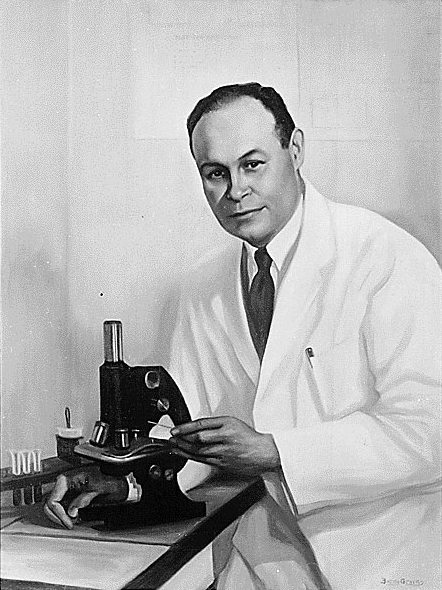
James Blundell, pioneer of blood transfusion
' British Journal of Hospital Medicine, August 2007, Vol 68, No 8. He made a substantial amount of money from this endeavour, roughly $2 million ($50 million real dollars). In 1840, at St George's Hospital Medical School in London, Samuel Armstrong Lane, aided by Blundell, performed the first successful whole blood transfusion to treat haemophilia. However, early transfusions were risky and many resulted in the death of the patient. By the late 19th century, blood transfusion was regarded as a risky and dubious procedure, and was largely shunned by the medical establishment. Work to emulate James Blundell continued in Edinburgh. In 1845 the Edinburgh Journal described the successful transfusion of blood to a woman with severe uterine bleeding. Subsequent transfusions were successful with patients of Professor James Young Simpson after whom the
 Only in 1901, when the Austrian Karl Landsteiner discovered three human
Only in 1901, when the Austrian Karl Landsteiner discovered three human
 While the first transfusions had to be made directly from donor to receiver before coagulation, it was discovered that by adding anticoagulant and
While the first transfusions had to be made directly from donor to receiver before coagulation, it was discovered that by adding anticoagulant and
''Toronto Star''. July 9, 2016. Katie Daubs Robertson published his findings in the '' British Medical Journal'' in 1916 and, with the help of a few like-minded individuals (including the eminent physician
Robertson published his findings in the '' British Medical Journal'' in 1916 and, with the help of a few like-minded individuals (including the eminent physician
 The secretary of the British Red Cross, Percy Oliver, established the world's first blood-donor service in 1921. In that year, Oliver was contacted by
The secretary of the British Red Cross, Percy Oliver, established the world's first blood-donor service in 1921. In that year, Oliver was contacted by  Frederic Durán-Jordà established one of the earliest blood banks during the
Frederic Durán-Jordà established one of the earliest blood banks during the
 The resulting dried plasma package came in two tin cans containing 400 mL bottles. One bottle contained enough
The resulting dried plasma package came in two tin cans containing 400 mL bottles. One bottle contained enough
Milk as a Substitute for Blood Transfusion
, historical account,
Transfusion Evidence Library
searchable source of evidence for transfusion medicine.
British Blood Transfusion Society
(BBTS)
International Society of Blood Transfusion
(ISBT)
''Blood Groups and Red Cell Antigens''
Free online book at
''Handbook of Transfusion Medicine''
Free book published in the UK 5th edition
American Association of Blood Banks Clinical Practice Guidelines
Australian National Blood Authority Patient Blood Management Guidelines
* ttps://www.nice.org.uk/guidance/ng24 National Institute for Health and Care Excellence Blood Transfusion GuidanceUK Guidance for transfusion.
Canadian Blood Transfusion Guidelines
German Medical Association Guidelines (English)
published 2014.
Blood Transfusion Leaflets
(NHS Blood and Transplant)
Blood Transfusion Leaflets
(Welsh Blood Service)
Blood Transfusion Information
(Scotland)
Blood Transfusion Information
(Australia)
(American Cancer Society) {{Authority control Transfusion medicine Hematology Blood
blood product
A blood product is any therapeutic substance prepared from human blood. This includes whole blood; blood components; and plasma derivatives. Whole blood is not commonly used in transfusion medicine. Blood components include: red blood cell conc ...
s into a person's circulation intravenously. Transfusions are used for various medical conditions to replace lost components of the blood. Early transfusions used whole blood
Whole blood (WB) is human blood from a standard blood donation. It is used in the treatment of massive bleeding, in exchange transfusion, and when people donate blood to themselves. One unit of whole blood (~517 mls) brings up hemoglobin level ...
, but modern medical practice commonly uses only components of the blood, such as red blood cells, white blood cells, plasma, clotting factors
Coagulation, also known as clotting, is the process by which blood changes from a liquid to a gel, forming a blood clot. It potentially results in hemostasis, the cessation of blood loss from a damaged vessel, followed by repair. The mechanism o ...
and platelets.
Red blood cells (RBC) contain hemoglobin, and supply the cells of the body with oxygen
Oxygen is the chemical element with the symbol O and atomic number 8. It is a member of the chalcogen group in the periodic table, a highly reactive nonmetal, and an oxidizing agent that readily forms oxides with most elements as ...
. White blood cells are not commonly used during transfusion, but they are part of the immune system, and also fight infections. Plasma is the "yellowish" liquid part of blood, which acts as a buffer, and contains proteins and important substances needed for the body's overall health. Platelets are involved in blood clotting, preventing the body from bleeding. Before these components were known, doctors believed that blood was homogeneous. Because of this scientific misunderstanding, many patients died because of incompatible blood transferred to them.
Medical uses
Red cell transfusion


 Historically, red blood cell transfusion was considered when the hemoglobin level fell below 100g/L or
Historically, red blood cell transfusion was considered when the hemoglobin level fell below 100g/L or hematocrit
The hematocrit () (Ht or HCT), also known by several other names, is the volume percentage (vol%) of red blood cells (RBCs) in blood, measured as part of a blood test. The measurement depends on the number and size of red blood cells. It is norm ...
fell below 30%. Because each unit of blood given carries risks, a trigger level lower than that, at 70 to 80g/L, is now usually used, as it has been shown to have better patient outcomes. The administration of a single unit of blood is the standard for hospitalized people who are not bleeding, with this treatment followed with re-assessment and consideration of symptoms and hemoglobin concentration. Patients with poor oxygen saturation
Oxygen saturation (symbol SO2) is a relative measure of the concentration of oxygen that is dissolved or carried in a given medium as a proportion of the maximal concentration that can be dissolved in that medium at the given temperature. It ca ...
may need more blood. The advisory caution to use blood transfusion only with more severe anemia is in part due to evidence that outcomes are worsened if larger amounts are given. One may consider transfusion for people with symptoms of cardiovascular disease such as chest pain or shortness of breath. In cases where patients have low levels of hemoglobin due to iron deficiency, but are cardiovascularly stable, parenteral iron
Iron supplements, also known as iron salts and iron pills, are a number of iron formulations used to treat and prevent iron deficiency including iron deficiency anemia. For prevention they are only recommended in those with poor absorption, ...
is a preferred option based on both efficacy and safety. Other blood products are given where appropriate, e.g., to treat clotting deficiencies.
Procedure
 Before a blood transfusion is given, there are many steps taken to ensure quality of the blood products, compatibility, and safety to the recipient. In 2012, a national blood policy was in place in 70% of countries and 69% of countries had specific legislation that covers the safety and quality of blood transfusion.
Before a blood transfusion is given, there are many steps taken to ensure quality of the blood products, compatibility, and safety to the recipient. In 2012, a national blood policy was in place in 70% of countries and 69% of countries had specific legislation that covers the safety and quality of blood transfusion.
Blood donation
Blood transfusions use as sources of blood either one's own (autologous
Autotransplantation is the transplantation of organs, tissues, or even particular proteins from one part of the body to another in the same person ('' auto-'' meaning "self" in Greek).
The autologous tissue (also called autogenous, autogenei ...
transfusion), or someone else's (allogeneic
Allotransplant (''allo-'' meaning "other" in Greek) is the transplantation of cells, tissues, or organs to a recipient from a genetically non-identical donor of the same species. The transplant is called an allograft, allogeneic transplant, o ...
or homologous transfusion). The latter is much more common than the former. Using another's blood must first start with donation of blood. Blood is most commonly donated as whole blood
Whole blood (WB) is human blood from a standard blood donation. It is used in the treatment of massive bleeding, in exchange transfusion, and when people donate blood to themselves. One unit of whole blood (~517 mls) brings up hemoglobin level ...
obtained intravenously and mixed with an anticoagulant. In developed countries, donations are usually anonymous to the recipient, but products in a blood bank
A blood bank is a center where blood gathered as a result of blood donation is stored and preserved for later use in blood transfusion. The term "blood bank" typically refers to a department of a hospital usually within a Clinical Pathology laborat ...
are always individually traceable through the whole cycle of donation, testing, separation into components, storage, and administration to the recipient. This enables management and investigation of any suspected transfusion related disease transmission or transfusion reaction. In developing countries, the donor is sometimes specifically recruited by or for the recipient, typically a family member, and the donation occurs immediately before the transfusion.
It is unclear whether applying alcohol swab alone or alcohol swab followed by antiseptic is able to reduce contamination of donor's blood.
Processing and testing
red blood cell
Red blood cells (RBCs), also referred to as red cells, red blood corpuscles (in humans or other animals not having nucleus in red blood cells), haematids, erythroid cells or erythrocytes (from Greek ''erythros'' for "red" and ''kytos'' for "holl ...
s, plasma, platelet
Platelets, also called thrombocytes (from Greek θρόμβος, "clot" and κύτος, "cell"), are a component of blood whose function (along with the coagulation factors) is to react to bleeding from blood vessel injury by clumping, thereby i ...
s, albumin protein
Proteins are large biomolecules and macromolecules that comprise one or more long chains of amino acid residues. Proteins perform a vast array of functions within organisms, including catalysing metabolic reactions, DNA replication, res ...
, clotting factor concentrates, cryoprecipitate, fibrinogen
Fibrinogen (factor I) is a glycoprotein complex, produced in the liver, that circulates in the blood of all vertebrates. During tissue and vascular injury, it is converted enzymatically by thrombin to fibrin and then to a fibrin-based blood cl ...
concentrate, and immunoglobulins ( antibodies). Red cells, plasma and platelets can also be donated individually via a more complex process called apheresis
Apheresis ( ἀφαίρεσις (''aphairesis'', "a taking away")) is a medical technology in which the blood of a person is passed through an apparatus that separates out one particular constituent and returns the remainder to the circulation ...
.
* The World Health Organization
The World Health Organization (WHO) is a specialized agency of the United Nations responsible for international public health. The WHO Constitution states its main objective as "the attainment by all peoples of the highest possible level of ...
(WHO) recommends that all donated blood be tested for transfusion-transmissible infections. These include HIV
The human immunodeficiency viruses (HIV) are two species of ''Lentivirus'' (a subgroup of retrovirus) that infect humans. Over time, they cause acquired immunodeficiency syndrome (AIDS), a condition in which progressive failure of the immune ...
, hepatitis B
Hepatitis B is an infectious disease caused by the '' Hepatitis B virus'' (HBV) that affects the liver; it is a type of viral hepatitis. It can cause both acute and chronic infection.
Many people have no symptoms during an initial infection. ...
, hepatitis C, '' Treponema pallidum'' ( syphilis) and, where relevant, other infections that pose a risk to the safety of the blood supply, such as '' Trypanosoma cruzi'' ( Chagas disease) and '' Plasmodium'' species (malaria
Malaria is a mosquito-borne infectious disease that affects humans and other animals. Malaria causes symptoms that typically include fever, tiredness, vomiting, and headaches. In severe cases, it can cause jaundice, seizures, coma, or death. S ...
). According to the WHO, 25 countries are not able to screen all donated blood for one or more of: HIV
The human immunodeficiency viruses (HIV) are two species of ''Lentivirus'' (a subgroup of retrovirus) that infect humans. Over time, they cause acquired immunodeficiency syndrome (AIDS), a condition in which progressive failure of the immune ...
, hepatitis B, hepatitis C, or syphilis. One of the main reasons for this is because testing kits are not always available. However the prevalence of transfusion-transmitted infections is much higher in low income countries compared to middle and high income countries.
* All donated blood should also be tested for the ABO blood group system
The ABO blood group system is used to denote the presence of one, both, or neither of the A and B antigens on erythrocytes. For human blood transfusions, it is the most important of the 43 different blood type (or group) classification system ...
and Rh blood group system to ensure that the patient is receiving compatible blood.
* In addition, in some countries platelet products are also tested for bacterial infections due to its higher inclination for contamination due to storage at room temperature. Presence of cytomegalovirus (CMV) may also be tested because of the risk to certain immunocompromised recipients if given, such as those with organ transplant or HIV. However, not all blood is tested for CMV because only a certain amount of CMV-negative blood needs to be available to supply patient needs. Other than positivity for CMV, any products tested positive for infections are not used.
* Leukocyte reduction is the removal of white blood cells by filtration. Leukoreduced blood products are less likely to cause HLA alloimmunization
Alloimmunity (sometimes called isoimmunity) is an immune response to nonself antigens from members of the same species, which are called alloantigens or isoantigens. Two major types of alloantigens are blood group antigens and histocompatibility ...
(development of antibodies against specific blood types), febrile non-hemolytic transfusion reaction, cytomegalovirus infection, and platelet-transfusion refractoriness.
* Pathogen Reduction treatment that involves, for example, the addition of riboflavin with subsequent exposure to UV light has been shown to be effective in inactivating pathogens (viruses, bacteria, parasites and white blood cells) in blood products. By inactivating white blood cells in donated blood products, riboflavin and UV light treatment can also replace gamma-irradiation as a method to prevent graft-versus-host disease ( TA-GvHD).
Compatibility testing
 Before a recipient receives a transfusion, compatibility testing between donor and recipient blood must be done. The first step before a transfusion is given is to type and screen the recipient's blood. Typing of recipient's blood determines the ABO and Rh status. The sample is then screened for any alloantibodies that may react with donor blood.Blood Processing.
Before a recipient receives a transfusion, compatibility testing between donor and recipient blood must be done. The first step before a transfusion is given is to type and screen the recipient's blood. Typing of recipient's blood determines the ABO and Rh status. The sample is then screened for any alloantibodies that may react with donor blood.Blood Processing. University of Utah
The University of Utah (U of U, UofU, or simply The U) is a public research university in Salt Lake City, Utah. It is the flagship institution of the Utah System of Higher Education. The university was established in 1850 as the University of De ...
. Available athttp://library.med.utah.edu/WebPath/TUTORIAL/BLDBANK/BBPROC.html
Accessed on: December 15, 2006. It takes about 45 minutes to complete (depending on the method used). The blood bank scientist also checks for special requirements of the patient (e.g. need for washed, irradiated or CMV negative blood) and the history of the patient to see if they have previously identified antibodies and any other serological anomalies.
 A positive screen warrants an antibody panel/investigation to determine if it is clinically significant. An antibody panel consists of commercially prepared group O red cell suspensions from donors that have been phenotyped for antigens that correspond to commonly encountered and clinically significant alloantibodies. Donor cells may have homozygous (e.g. K+k+), heterozygous (K+k-) expression or no expression of various antigens (K−k−). The phenotypes of all the donor cells being tested are shown in a chart. The patient's serum is tested against the various donor cells. Based on the reactions of the patient's serum against the donor cells, a pattern will emerge to confirm the presence of one or more antibodies. Not all antibodies are clinically significant (i.e. cause transfusion reactions, HDN, etc.). Once the patient has developed a clinically significant antibody it is vital that the patient receive antigen-negative red blood cells to prevent future transfusion reactions. A direct antiglobulin test ( Coombs test) is also performed as part of the antibody investigation.
If there is no antibody present, an immediate spin crossmatch or computer-assisted crossmatch is performed where the recipient serum and donor rbc are incubated. In the immediate spin method, two drops of patient serum are tested against a drop of 3–5% suspension of donor cells in a test tube and spun in a serofuge. Agglutination or hemolysis (i.e., positive Coombs test) in the test tube is a positive reaction and the unit should not be transfused.
If an antibody is suspected, potential donor units must first be screened for the corresponding antigen by phenotyping them. Antigen negative units are then tested against the patient plasma using an antiglobulin/indirect crossmatch technique at 37 degrees Celsius to enhance reactivity and make the test easier to read.
In urgent cases where crossmatching cannot be completed, and the risk of dropping hemoglobin outweighs the risk of transfusing uncrossmatched blood, O-negative blood is used, followed by crossmatch as soon as possible. O-negative is also used for children and women of childbearing age. It is preferable for the laboratory to obtain a pre-transfusion sample in these cases so a type and screen can be performed to determine the actual blood group of the patient and to check for alloantibodies.
A positive screen warrants an antibody panel/investigation to determine if it is clinically significant. An antibody panel consists of commercially prepared group O red cell suspensions from donors that have been phenotyped for antigens that correspond to commonly encountered and clinically significant alloantibodies. Donor cells may have homozygous (e.g. K+k+), heterozygous (K+k-) expression or no expression of various antigens (K−k−). The phenotypes of all the donor cells being tested are shown in a chart. The patient's serum is tested against the various donor cells. Based on the reactions of the patient's serum against the donor cells, a pattern will emerge to confirm the presence of one or more antibodies. Not all antibodies are clinically significant (i.e. cause transfusion reactions, HDN, etc.). Once the patient has developed a clinically significant antibody it is vital that the patient receive antigen-negative red blood cells to prevent future transfusion reactions. A direct antiglobulin test ( Coombs test) is also performed as part of the antibody investigation.
If there is no antibody present, an immediate spin crossmatch or computer-assisted crossmatch is performed where the recipient serum and donor rbc are incubated. In the immediate spin method, two drops of patient serum are tested against a drop of 3–5% suspension of donor cells in a test tube and spun in a serofuge. Agglutination or hemolysis (i.e., positive Coombs test) in the test tube is a positive reaction and the unit should not be transfused.
If an antibody is suspected, potential donor units must first be screened for the corresponding antigen by phenotyping them. Antigen negative units are then tested against the patient plasma using an antiglobulin/indirect crossmatch technique at 37 degrees Celsius to enhance reactivity and make the test easier to read.
In urgent cases where crossmatching cannot be completed, and the risk of dropping hemoglobin outweighs the risk of transfusing uncrossmatched blood, O-negative blood is used, followed by crossmatch as soon as possible. O-negative is also used for children and women of childbearing age. It is preferable for the laboratory to obtain a pre-transfusion sample in these cases so a type and screen can be performed to determine the actual blood group of the patient and to check for alloantibodies.
Compatibility of ABO and Rh system for Red Cell (Erythrocyte) Transfusion
This chart shows possible matches in blood transfusion between donor and receiver using ABO and Rh system.Adverse effects
In the same way that the safety of pharmaceutical products is overseen by pharmacovigilance, the safety of blood and blood products is overseen by haemovigilance. This is defined by the World Health Organization (WHO) as a system "...to identify and prevent occurrence or recurrence of transfusion related unwanted events, to increase the safety, efficacy and efficiency of blood transfusion, covering all activities of the transfusion chain from donor to recipient." The system should include monitoring, identification, reporting, investigation and analysis of adverse events near-misses and reactions related to transfusion and manufacturing. In the UK this data is collected by an independent organisation called SHOT (Serious Hazards Of Transfusion). Transfusions of blood products are associated with several complications, many of which can be grouped as immunological or infectious. There is controversy on potential quality degradation during storage.Immunologic reaction
* Acute hemolytic reactions are defined according to Serious Hazards of Transfusion (SHOT) as "fever and other symptoms/signs of haemolysis within 24 hours of transfusion; confirmed by one or more of the following: a fall of Hb, rise in lactate dehydrogenase (LDH), positive direct antiglobulin test (DAT), positive crossmatch" This is due to destruction of donor red blood cells by preformed recipient antibodies. Most often this occurs because of clerical errors or improper ABO blood typing and crossmatching resulting in a mismatch in ABO blood type between the donor and the recipient. Symptoms include fever, chills, chest pain, back pain, hemorrhage, increased heart rate, shortness of breath, and rapid drop in blood pressure. When suspected, transfusion should be stopped immediately, and blood sent for tests to evaluate for presence of hemolysis. Treatment is supportive. Kidney injury may occur because of the effects of the hemolytic reaction (pigment nephropathy). The severity of the transfusion reaction is depended upon amount of donor's antigen transfused, nature of the donor's antigens, the nature and the amount of recipient antibodies. * Delayed hemolytic reactions occur more than 24 hours after a transfusion. They usually occur within 28 days of a transfusion. They can be due to either a low level of antibodies present prior to the start of the transfusion, which are not detectable on pre-transfusion testing; or development of a new antibody against an antigen in the transfused blood. Therefore, delayed haemolytic reaction does not manifest until after 24 hours when enough antibodies are available to cause a reaction. The red blood cells are removed by macrophages from the blood circulation into liver and spleen to be destroyed, which leads to extravascular haemolysis. This process usually mediated by anti-Rh and anti-Kidd antibodies. However, this type of transfusion reaction is less severe when compared to acute haemolytic transfusion reaction. * Febrile nonhemolytic reactions are, along with allergic transfusion reactions, the most common type of blood transfusion reaction and occur because of the release of inflammatory chemical signals released by white blood cells in stored donor blood or attack on donor's white blood cells by recipient's antibodies. This type of reaction occurs in about 7% of transfusions. Fever is generally short lived and is treated withantipyretic
An antipyretic (, from ''anti-'' 'against' and ' 'feverish') is a substance that reduces fever. Antipyretics cause the hypothalamus to override a prostaglandin-induced increase in temperature. The body then works to lower the temperature, which r ...
s, and transfusions may be finished as long as an acute hemolytic reaction is excluded. This is a reason for the now-widespread use of leukoreduction – the filtration of donor white cells from red cell product units.
* Allergic transfusion reaction An allergic transfusion reaction is when a blood transfusion results in allergic reaction. It is among the most common transfusion reactions to occur. Reported rates depend on the degree of active surveillance versus passing reporting to the blood ...
s are caused by IgE anti-allergen antibodies. When antibodies are bound to its antigens, histamine is released from mast cell
A mast cell (also known as a mastocyte or a labrocyte) is a resident cell of connective tissue that contains many granules rich in histamine and heparin. Specifically, it is a type of granulocyte derived from the myeloid stem cell that is a par ...
s and basophil
Basophils are a type of white blood cell. Basophils are the least common type of granulocyte, representing about 0.5% to 1% of circulating white blood cells. However, they are the largest type of granulocyte. They are responsible for inflammator ...
s. Either IgE antibodies from the donor's or recipient's side can cause the allergic reaction. It is more common in patients who have allergic conditions such as hay fever. Patient may feel itchy or having hives but the symptoms are usually mild and can be controlled by stopping the transfusion and giving antihistamines.
* Anaphylactic reactions are rare life-threatening allergic conditions caused by IgA anti-plasma protein antibodies. For patients who have selective immunoglobulin A deficiency, the reaction is presumed to be caused by IgA antibodies in the donor's plasma. The patient may present with symptoms of fever, wheezing, coughing, shortness of breath, and circulatory shock. Urgent treatment with epinephrine is needed.
* Post-transfusion purpura is an extremely rare complication that occurs after blood product transfusion and is associated with the presence of antibodies in the patient's blood directed against both the donor's and recipient's platelets HPA (human platelet antigen). Recipients who lack this protein develop sensitization to this protein from prior transfusions or previous pregnancies, can develop thrombocytopenia, bleeding into the skin, and can display purplish discolouration of skin which is known as purpura. Intravenous immunoglobulin (IVIG) is treatment of choice.
* Transfusion-related acute lung injury (TRALI) is a syndrome that is similar to acute respiratory distress syndrome (ARDS), which develops during or within 6 hours of transfusion of a plasma-containing blood product. Fever, hypotension, shortness of breath, and tachycardia often occurs in this type of reaction. For a definitive diagnosis to be made, symptoms must occur within 6 hours of transfusion, hypoxemia must be present, there must be radiographic evidence of bilateral infiltrates and there must be no evidence of left atrial hypertension (fluid overload). It occurs in 15% of the transfused patient with mortality rate of 5 to 10%. Recipient risk factors includes: end-stage liver disease, sepsis, haematological malignancies, sepsis, and ventilated patients. Antibodies to human neutrophil antigens (HNA) and human leukocyte antigens (HLA) have been associated with this type of transfusion reaction. Donor's antibodies interacting with antigen positive recipient tissue result in release of inflammatory cytokines, resulting in pulmonary capillary leakage. The treatment is supportive.
* Transfusion associated circulatory overload (TACO) is a common, yet underdiagnosed, reaction to blood product transfusion consisting of the new onset or exacerbation of three of the following within 6 hours of cessation of transfusion: acute respiratory distress, elevated brain natriuretic peptide (BNP), elevated central venous pressure (CVP), evidence of left heart failure, evidence of positive fluid balance, and/or radiographic evidence of pulmonary edema.
* Transfusion-associated graft versus host disease
Transfusion-associated graft-versus-host disease (TA-GvHD) is a rare complication of blood transfusion, in which the immunologically competent donor T lymphocytes mount an immune response against the recipient's lymphoid tissue. These donor lympho ...
frequently occurs in immunodeficient patients where recipient's body failed to eliminate donor's T cells. Instead, donor's T cells attack the recipient's cells. It occurs one week after transfusion. Fever, rash, diarrhoea are often associated with this type of transfusion reaction. Mortality rate is high, with 89.7% of the patients dead after 24 days. Immunosuppressive treatment is the most common way of treatment. Irradiation and leukoreduction of blood products is necessary for high risk patients to prevent T cells from attacking recipient cells.
Infection
The use of greater amount of red blood cells is associated with a high risk of infections. In those who were given red blood only with significant anemia infection rates were 12% while in those who were given red blood at milder levels of anemia infection rates were 17%. On rare occasions, blood products are contaminated with bacteria. This can result in a life-threatening infection known as transfusion-transmitted bacterial infection. The risk of severe bacterial infection is estimated, , at about 1 in 50,000 platelet transfusions, and 1 in 500,000 red blood cell transfusions. Blood product contamination, while rare, is still more common than actual infection. The reason platelets are more often contaminated than other blood products is that they are stored at room temperature for short periods of time. Contamination is also more common with longer duration of storage, especially if that means more than 5 days. Sources of contaminants include the donor's blood, donor's skin, phlebotomist's skin, and containers. Contaminating organisms vary greatly, and include skin flora, gut flora, and environmental organisms. There are many strategies in place at blood donation centers and laboratories to reduce the risk of contamination. A definite diagnosis of transfusion-transmitted bacterial infection includes the identification of a positive culture in the recipient (without an alternative diagnosis) as well as the identification of the same organism in the donor blood. Since the advent of HIV testing of donor blood in the mid/later 1980s, ex. 1985's ELISA, the transmission of HIV during transfusion has dropped dramatically. Prior testing of donor blood only included testing for antibodies to HIV. However, because of latent infection (the "window period" in which an individual is infectious, but has not had time to develop antibodies) many cases of HIV seropositive blood were missed. The development of a nucleic acid test for the HIV-1 RNA has dramatically lowered the rate of donor blood seropositivity to about 1 in 3 million units. As transmittance of HIV does not necessarily mean HIV infection, the latter could still occur at an even lower rate. The transmission of hepatitis C via transfusion currently stands at a rate of about 1 in 2 million units. As with HIV, this low rate has been attributed to the ability to screen for both antibodies as well as viral RNA nucleic acid testing in donor blood. Other rare transmissible infections includehepatitis B
Hepatitis B is an infectious disease caused by the '' Hepatitis B virus'' (HBV) that affects the liver; it is a type of viral hepatitis. It can cause both acute and chronic infection.
Many people have no symptoms during an initial infection. ...
, syphilis, Chagas disease, cytomegalovirus infections (in immunocompromised recipients), HTLV
The human T-lymphotropic virus, human T-cell lymphotropic virus, or human T-cell leukemia-lymphoma virus (HTLV) family of viruses are a group of human retroviruses that are known to cause a type of cancer called adult T-cell leukemia/lymphoma an ...
, and Babesia.
Comparison table
Inefficacy
Transfusion inefficacy or insufficient efficacy of a given unit(s) of blood product, while not itself a "complication" ''per se'', can nonetheless indirectly lead to complications – in addition to causing a transfusion to fully or partly fail to achieve its clinical purpose. This can be especially significant for certain patient groups such as critical-care or neonatals. For red blood cells (RBC), by far the most commonly transfused product, poor transfusion efficacy can result from units damaged by the so-called storage lesion – a range of biochemical and biomechanical changes that occur during storage. With red cells, this can decrease viability and ability for tissue oxygenation. Although some of the biochemical changes are reversible after the blood is transfused, the biomechanical changes are less so, and rejuvenation products are not yet able to adequately reverse this phenomenon. There has been controversy about whether a given product unit's age is a factor in transfusion efficacy, specifically about whether "older" blood directly or indirectly increases risks of complications. Studies have not been consistent on answering this question, with some showing that older blood is indeed less effective but with others showing no such difference; these developments are being closely followed by hospitalblood bank
A blood bank is a center where blood gathered as a result of blood donation is stored and preserved for later use in blood transfusion. The term "blood bank" typically refers to a department of a hospital usually within a Clinical Pathology laborat ...
ers – who are the physicians, typically pathologists, who collect and manage inventories of transfusable blood units.
Certain regulatory measures are in place to minimize RBC storage lesion – including a maximum shelf life (currently 42 days), a maximum auto-hemolysis threshold (currently 1% in the US, 0.8% in Europe), and a minimum level of post-transfusion RBC survival ''in vivo'' (currently 75% after 24 hours). However, all of these criteria are applied in a universal manner that does not account for differences among units of product. For example, testing for the post-transfusion RBC survival ''in vivo'' is done on a sample of healthy volunteers, and then compliance is presumed for all RBC units based on universal (GMP) processing standards (RBC survival by itself does not guarantee efficacy, but it is a necessary prerequisite for cell function, and hence serves as a regulatory proxy). Opinions vary as to the "best" way to determine transfusion efficacy in a patient ''in vivo''. In general, there are not yet any ''in vitro'' tests to assess quality or predict efficacy for specific units of RBC blood product prior to their transfusion, though there is exploration of potentially relevant tests based on RBC membrane properties such as erythrocyte deformability and erythrocyte fragility (mechanical).
Physicians have adopted a so-called "restrictive protocol" – whereby transfusion is held to a minimum – in part because of the noted uncertainties surrounding storage lesion, in addition to the very high direct and indirect costs of transfusions. However, the restrictive protocol is not an option with some especially vulnerable patients who may require the best possible efforts to rapidly restore tissue oxygenation.
Although transfusions of platelets are far less numerous (relative to RBC), platelet storage lesion and resulting efficacy loss is also a concern.
Other
* A known relationship between intra-operative blood transfusion and cancer recurrence has been established in colorectal cancer. In lung cancer intra-operative blood transfusion has been associated with earlier recurrence of cancer, worse survival rates and poorer outcomes after lung resection. Also studies shown to us, failure of the immune system caused by blood transfusion can be categorized as one of the main factors leading to more than 10 differentcancer
Cancer is a group of diseases involving abnormal cell growth with the potential to invade or spread to other parts of the body. These contrast with benign tumors, which do not spread. Possible signs and symptoms include a lump, abnormal b ...
types that are fully associated with blood transfusion and the innate and adaptive immune system. Allogeneic blood transfusion, through five major mechanisms including the lymphocyte-T set, myeloid-derived suppressor cells (MDSCs), tumor-associated macrophages (TAMs), natural killer cells
Natural killer cells, also known as NK cells or large granular lymphocytes (LGL), are a type of cytotoxic lymphocyte critical to the innate immune system that belong to the rapidly expanding family of known innate lymphoid cells (ILC) and represen ...
(NKCs), and dendritic cells
Dendritic cells (DCs) are antigen-presenting cells (also known as ''accessory cells'') of the mammalian immune system. Their main function is to process antigen material and present it on the cell surface to the T cells of the immune system. The ...
(DCs) can help the recipient's defense mechanisms. On the other hand, the role for each of the listed items includes activation of the antitumor CD8+
A cytotoxic T cell (also known as TC, cytotoxic T lymphocyte, CTL, T-killer cell, cytolytic T cell, CD8+ T-cell or killer T cell) is a T lymphocyte (a type of white blood cell) that kills cancer cells, cells that are infected by intracellular pa ...
cytotoxic T lymphocytes
A cytotoxic T cell (also known as TC, cytotoxic T lymphocyte, CTL, T-killer cell, cytolytic T cell, CD8+ T-cell or killer T cell) is a T lymphocyte (a type of white blood cell) that kills cancer cells, cells that are infected by intracellular pa ...
(CD8+/CTL), temporal inactivation of Tregs, inactivation of the STAT3
Signal transducer and activator of transcription 3 (STAT3) is a transcription factor which in humans is encoded by the ''STAT3'' gene. It is a member of the STAT protein family.
Function
STAT3 is a member of the STAT protein family. In respons ...
signaling pathway, the use of bacteria
Bacteria (; singular: bacterium) are ubiquitous, mostly free-living organisms often consisting of one Cell (biology), biological cell. They constitute a large domain (biology), domain of prokaryotic microorganisms. Typically a few micrometr ...
to enhance the antitumor immune response and cellular Immunotherapy
Immunotherapy or biological therapy is the treatment of disease by activating or suppressing the immune system. Immunotherapies designed to elicit or amplify an immune response are classified as ''activation immunotherapies,'' while immunotherap ...
.
* Transfusion-associated volume overload is a common complication simply because blood products have a certain amount of volume. This is especially the case in recipients with underlying cardiac or kidney disease. Red cell transfusions can lead to volume overload when they must be repeated because of insufficient efficacy (see above). Plasma transfusion is especially prone to causing volume overload because large volumes are usually required to give any therapeutic benefit.
* It has been proved that blood transfusion produce worse outcomes after cytoreductive surgery and HIPEC.
* Hypothermia can occur with transfusions with large quantities of blood products which normally are stored at cold temperatures. Core body temperature can go down as low as 32 °C and can produce physiologic disturbances. Prevention should be done with warming the blood to ambient temperature prior to transfusions.
* Transfusions with large amounts of red blood cells, whether due to severe hemorrhaging and/or transfusion inefficacy (see above), can lead to an inclination for bleeding. The mechanism is thought to be due to disseminated intravascular coagulation, along with dilution of recipient platelets and coagulation factors. Close monitoring and transfusions with platelets and plasma is indicated when necessary.
* Metabolic alkalosis can occur with massive blood transfusions because of the breakdown of citrate stored in blood into bicarbonate.
* Hypocalcemia can also occur with massive blood transfusions because of the complex of citrate with serum calcium. Calcium levels below 0.9 mmol/L should be treated.
* Blood doping
Blood doping is a form of doping in which the number of red blood cells in the bloodstream is boosted in order to enhance athletic performance. Because such blood cells carry oxygen from the lungs to the muscles, a higher concentration in the blo ...
is often used by athletes, drug addicts or military personnel for reasons such as to increase physical stamina, to fake a drug detection test or simply to remain active and alert during the duty-times respectively. However a lack of knowledge and insufficient experience can turn a blood transfusion into a sudden death. For example, when individuals run the frozen blood sample directly in their veins this cold blood rapidly reaches the heart, where it disturbs the heart's original pace leading to cardiac arrest and sudden death.
Frequency of use
Globally around 85 million units of red blood cells are transfused in a given year. In the United States, blood transfusions were performed nearly 3 million times during hospitalizations in 2011, making it the most common procedure performed. The rate of hospitalizations with a blood transfusion nearly doubled from 1997, from a rate of 40 stays to 95 stays per 10,000 population. It was the most common procedure performed for patients 45 years of age and older in 2011, and among the top five most common for patients between the ages of 1 and 44 years. According to the ''New York Times'': "Changes in medicine have eliminated the need for millions of blood transfusions, which is good news for patients getting procedures like coronary bypasses and other procedures that once required a lot of blood." And, "Blood bank revenue is falling, and the decline may reach $1.5 billion a year this year 014from a high of $5 billion in 2008." Job losses will reach as high as 12,000 within the next three to five years, roughly a quarter of the total in the industry, according to the Red Cross.History
Beginning withWilliam Harvey
William Harvey (1 April 1578 – 3 June 1657) was an English physician who made influential contributions in anatomy and physiology. He was the first known physician to describe completely, and in detail, the systemic circulation and propert ...
's experiments on the circulation of blood, recorded research into blood transfusion began in the 17th century, with successful experiments in transfusion between animals. However, successive attempts by physicians to transfuse animal blood into humans gave variable, often fatal, results.
Pope Innocent VIII is sometimes said to have been given "the world's first blood transfusion" by his physician Giacomo di San Genesio, who had him drink (by mouth) the blood of three 10-year-old boys. The boys subsequently died. The evidence for this story, however, is unreliable and considered a possible anti-Jewish blood libel.
Early attempts
The Incas The first reported successful blood transfusions were performed by theIncas
The Inca Empire (also known as the Incan Empire and the Inka Empire), called ''Tawantinsuyu'' by its subjects, ( Quechua for the "Realm of the Four Parts", "four parts together" ) was the largest empire in pre-Columbian America. The adm ...
as early as the 1500s. Spanish conquistadors witnessed blood transfusions when they arrived in the sixteenth century. The prevalence of type O blood among Indigenous people of the Andean region meant such procedures would have held less risk than blood transfusion attempts among populations with incompatible blood types, which contributed to the failures of early attempts in Europe.
Animal blood
 Working at the Royal Society in the 1660s, the physician Richard Lower began examining the effects of changes in blood volume on circulatory function and developed methods for cross-circulatory study in animals, obviating clotting by closed arteriovenous connections. The new instruments he was able to devise enabled him to perform the first reliably documented successful transfusion of blood in front of his distinguished colleagues from the Royal Society.
According to Lower's account, "...towards the end of February 1665 selected one dog of medium size, opened its jugular vein, and drew off blood, until its strength was nearly gone. Then, to make up for the great loss of this dog by the blood of a second, I introduced blood from the cervical artery of a fairly large mastiff, which had been fastened alongside the first, until this latter animal showed ... it was overfilled ... by the inflowing blood." After he "sewed up the jugular veins", the animal recovered "with no sign of discomfort or of displeasure".
Lower had performed the first blood transfusion between animals. He was then "requested by the Honorable obertBoyle ... to acquaint the Royal Society with the procedure for the whole experiment", which he did in December 1665 in the Society's '' Philosophical Transactions''.
The first blood transfusion from animal to human was administered by Dr. Jean-Baptiste Denys, eminent physician to King Louis XIV of France, on June 15, 1667. He transfused the blood of a sheep into a 15-year-old boy, who survived the transfusion. Denys performed another transfusion into a labourer, who also survived. Both instances were likely due to the small amount of blood that was actually transfused into these people. This allowed them to withstand the allergic reaction.
Denys's third patient to undergo a blood transfusion was Swedish Baron Gustaf Bonde. He received two transfusions. After the second transfusion Bonde died. In the winter of 1667, Denys performed several transfusions on Antoine Mauroy with calf's blood. On the third account Mauroy died.
Six months later in London, Lower performed the first human transfusion of animal blood in Britain, where he "superintended the introduction in patient'sarm at various times of some ounces of sheep's blood at a meeting of the Royal Society, and without any inconvenience to him." The recipient was Arthur Coga, "the subject of a harmless form of insanity." Sheep's blood was used because of speculation about the value of blood exchange between species; it had been suggested that blood from a gentle lamb might quiet the tempestuous spirit of an agitated person and that the shy might be made outgoing by blood from more sociable creatures. Coga received 20 shillings () to participate in the experiment.
Lower went on to pioneer new devices for the precise control of blood flow and the transfusion of blood; his designs were substantially the same as modern syringes and
Working at the Royal Society in the 1660s, the physician Richard Lower began examining the effects of changes in blood volume on circulatory function and developed methods for cross-circulatory study in animals, obviating clotting by closed arteriovenous connections. The new instruments he was able to devise enabled him to perform the first reliably documented successful transfusion of blood in front of his distinguished colleagues from the Royal Society.
According to Lower's account, "...towards the end of February 1665 selected one dog of medium size, opened its jugular vein, and drew off blood, until its strength was nearly gone. Then, to make up for the great loss of this dog by the blood of a second, I introduced blood from the cervical artery of a fairly large mastiff, which had been fastened alongside the first, until this latter animal showed ... it was overfilled ... by the inflowing blood." After he "sewed up the jugular veins", the animal recovered "with no sign of discomfort or of displeasure".
Lower had performed the first blood transfusion between animals. He was then "requested by the Honorable obertBoyle ... to acquaint the Royal Society with the procedure for the whole experiment", which he did in December 1665 in the Society's '' Philosophical Transactions''.
The first blood transfusion from animal to human was administered by Dr. Jean-Baptiste Denys, eminent physician to King Louis XIV of France, on June 15, 1667. He transfused the blood of a sheep into a 15-year-old boy, who survived the transfusion. Denys performed another transfusion into a labourer, who also survived. Both instances were likely due to the small amount of blood that was actually transfused into these people. This allowed them to withstand the allergic reaction.
Denys's third patient to undergo a blood transfusion was Swedish Baron Gustaf Bonde. He received two transfusions. After the second transfusion Bonde died. In the winter of 1667, Denys performed several transfusions on Antoine Mauroy with calf's blood. On the third account Mauroy died.
Six months later in London, Lower performed the first human transfusion of animal blood in Britain, where he "superintended the introduction in patient'sarm at various times of some ounces of sheep's blood at a meeting of the Royal Society, and without any inconvenience to him." The recipient was Arthur Coga, "the subject of a harmless form of insanity." Sheep's blood was used because of speculation about the value of blood exchange between species; it had been suggested that blood from a gentle lamb might quiet the tempestuous spirit of an agitated person and that the shy might be made outgoing by blood from more sociable creatures. Coga received 20 shillings () to participate in the experiment.
Lower went on to pioneer new devices for the precise control of blood flow and the transfusion of blood; his designs were substantially the same as modern syringes and catheter
In medicine, a catheter (/ˈkæθətər/) is a thin tubing (material), tube made from medical grade materials serving a broad range of functions. Catheters are medical devices that can be inserted in the body to treat diseases or perform a surgi ...
s. Shortly after, Lower moved to London, where his growing practice soon led him to abandon research.
These early experiments with animal blood provoked a heated controversy in Britain and France. Finally, in 1668, the Royal Society and the French government both banned the procedure. The Vatican
Vatican may refer to:
Vatican City, the city-state ruled by the pope in Rome, including St. Peter's Basilica, Sistine Chapel, Vatican Museum
The Holy See
* The Holy See, the governing body of the Catholic Church and sovereign entity recognized ...
condemned these experiments in 1670. Blood transfusions fell into obscurity for the next 150 years.
Human blood
 The science of blood transfusion dates to the first decade of the 20th century, with the discovery of distinct
The science of blood transfusion dates to the first decade of the 20th century, with the discovery of distinct blood types
Blood is a body fluid in the circulatory system of humans and other vertebrates that delivers necessary substances such as nutrients and oxygen to the cells, and transports metabolic waste products away from those same cells. Blood in the ...
leading to the practice of mixing some blood from the donor and the receiver before the transfusion (an early form of cross-matching
Cross-matching or crossmatching is a test performed before a blood transfusion as part of blood compatibility testing. Normally, this involves adding the recipient's blood plasma to a sample of the donor's red blood cells. If the blood is incom ...
).
In the early 19th century, British obstetrician
Obstetrics is the field of study concentrated on pregnancy, childbirth and the postpartum period. As a medical specialty, obstetrics is combined with gynecology under the discipline known as obstetrics and gynecology (OB/GYN), which is a surgic ...
Dr. James Blundell made efforts to treat hemorrhage by transfusion of human blood using a syringe. In 1818 following experiments with animals, he performed the first successful transfusion of human blood to treat postpartum hemorrhage
Postpartum bleeding or postpartum hemorrhage (PPH) is often defined as the loss of more than 500 ml or 1,000 ml of blood following childbirth. Some have added the requirement that there also be signs or symptoms of low blood volume fo ...
. Blundell used the patient's husband as a donor, and extracted four ounces of blood from his arm to transfuse into his wife. During the years 1825 and 1830, Blundell performed 10 transfusions, five of which were beneficial, and published his results. He also invented a number of instruments for the transfusion of blood.Ellis, H. ''Surgical AnniversariesJames Blundell, pioneer of blood transfusion
' British Journal of Hospital Medicine, August 2007, Vol 68, No 8. He made a substantial amount of money from this endeavour, roughly $2 million ($50 million real dollars). In 1840, at St George's Hospital Medical School in London, Samuel Armstrong Lane, aided by Blundell, performed the first successful whole blood transfusion to treat haemophilia. However, early transfusions were risky and many resulted in the death of the patient. By the late 19th century, blood transfusion was regarded as a risky and dubious procedure, and was largely shunned by the medical establishment. Work to emulate James Blundell continued in Edinburgh. In 1845 the Edinburgh Journal described the successful transfusion of blood to a woman with severe uterine bleeding. Subsequent transfusions were successful with patients of Professor James Young Simpson after whom the
Simpson Memorial Maternity Pavilion
The Edinburgh Royal Maternity and Simpson Memorial Pavilion was a maternity hospital in Lauriston, Edinburgh, Scotland. Its services have now been incorporated into the Royal Infirmary of Edinburgh at Little France.
History
Midwifery in Edinbu ...
in Edinburgh was named.
Various isolated reports of successful transfusions emerged towards the end of the 19th century. The largest series of early successful transfusions took place at the Edinburgh Royal Infirmary between 1885 and 1892. Edinburgh later became the home of the first blood donation and blood transfusion services.
20th century
 Only in 1901, when the Austrian Karl Landsteiner discovered three human
Only in 1901, when the Austrian Karl Landsteiner discovered three human blood groups
The term human blood group systems is defined by the International Society of Blood Transfusion (ISBT) as systems in the human species where cell-surface antigens—in particular, those on blood cells—are "controlled at a single gene locus or by ...
(O, A, and B), did blood transfusion achieve a scientific basis and become safer.
Landsteiner discovered that adverse effects arise from mixing blood from two incompatible individuals. He found that mixing incompatible types triggers an immune response and the red blood-cells clump. The immunological reaction occurs when the receiver of a blood transfusion has antibodies against the donor blood-cells. The destruction of red blood cells releases free hemoglobin into the bloodstream, which can have fatal consequences. Landsteiner's work made it possible to determine blood group and allowed blood transfusions to take place much more safely. For his discovery he won the Nobel Prize in Physiology and Medicine in 1930; many other blood groups have been discovered since.
George Washington Crile
George Washington Crile (November 11, 1864 – January 7, 1943) was an American surgeon. Crile is now formally recognized as the first surgeon to have succeeded in a direct blood transfusion. He contributed to other procedures, such as neck di ...
is credited with performing the first surgery using a direct blood transfusion in 1906 at St. Alexis Hospital in Cleveland while a professor of surgery at Case Western Reserve University.
Jan Janský also discovered the human blood groups; in 1907 he classified blood into four groups: I, II, III, IV. His nomenclature is still used in Russia and in states of the former USSR, in which blood types O, A, B, and AB are respectively designated I, II, III, and IV.
Dr. William Lorenzo Moss's (1876–1957) Moss-blood typing technique of 1910 was widely used until World War II
World War II or the Second World War, often abbreviated as WWII or WW2, was a world war that lasted from 1939 to 1945. It involved the vast majority of the world's countries—including all of the great powers—forming two opposing ...
.
William Stewart Halsted, M.D. (1852–1922), an American surgeon, performed one of the first blood transfusions in the United States. He had been called to see his sister after she had given birth. He found her moribund from blood loss, and in a bold move withdrew his own blood, transfused his blood into his sister, and then operated on her to save her life.
Blood banks in WWI
 While the first transfusions had to be made directly from donor to receiver before coagulation, it was discovered that by adding anticoagulant and
While the first transfusions had to be made directly from donor to receiver before coagulation, it was discovered that by adding anticoagulant and refrigerating
The term refrigeration refers to the process of removing heat from an enclosed space or substance for the purpose of lowering the temperature.International Dictionary of Refrigeration, http://dictionary.iifiir.org/search.phpASHRAE Terminology, ht ...
the blood it was possible to store it for some days, thus opening the way for the development of blood bank
A blood bank is a center where blood gathered as a result of blood donation is stored and preserved for later use in blood transfusion. The term "blood bank" typically refers to a department of a hospital usually within a Clinical Pathology laborat ...
s. John Braxton Hicks was the first to experiment with chemical methods to prevent the coagulation of blood at St Mary's Hospital, London in the late-19th century. His attempts, using phosphate of soda, however, proved unsuccessful.
The Belgian
Belgian may refer to:
* Something of, or related to, Belgium
* Belgians, people from Belgium or of Belgian descent
* Languages of Belgium, languages spoken in Belgium, such as Dutch, French, and German
*Ancient Belgian language, an extinct languag ...
doctor Albert Hustin performed the first non-direct transfusion on March 27, 1914, though this involved a diluted solution of blood. The Argentine doctor Luis Agote used a much less diluted solution in November of the same year. Both used sodium citrate as an anticoagulant.
The First World War
World War I (28 July 1914 11 November 1918), often abbreviated as WWI, was one of the deadliest global conflicts in history. Belligerents included much of Europe, the Russian Empire, the United States, and the Ottoman Empire, with fightin ...
(1914-1918) acted as a catalyst for the rapid development of blood banks and transfusion techniques. Canadian doctor and Lieutenant Lawrence Bruce Robertson became instrumental in persuading the Royal Army Medical Corps to adopt the use of blood transfusion at the Casualty Clearing Stations for the wounded. In October 1915, Robertson performed his first wartime transfusion with a syringe to a patient who had multiple shrapnel wounds. He followed this up with four subsequent transfusions in the following months, and his success was reported to Sir Walter Morley Fletcher
Sir Walter Morley Fletcher, (21 July 1873 – 7 June 1933)- was a British physiologist and administrator. Fletcher graduated from Trinity College, Cambridge
Trinity College is a constituent college of the University of Cambridge. Founded ...
, director of the Medical Research Committee."A Canadian kept blood flowing in WWI. An American got credit"''Toronto Star''. July 9, 2016. Katie Daubs
 Robertson published his findings in the '' British Medical Journal'' in 1916 and, with the help of a few like-minded individuals (including the eminent physician
Robertson published his findings in the '' British Medical Journal'' in 1916 and, with the help of a few like-minded individuals (including the eminent physician Edward William Archibald
Edward William Archibald (August 5, 1872 – December 17, 1945) was a Canadian surgeon. Archibald was born in Montreal, Quebec, and received his initial education in Grenoble, France. Upon returning to Canada, he attended McGill Univers ...
(1872–1945), who introduced the citrate anticoagulant method), was able to persuade the British authorities of the merits of blood transfusion. Robertson went on to establish the first blood-transfusion apparatus at a Casualty Clearing Station on the Western Front in the spring of 1917.
Oswald Hope Robertson
Oswald Hope Robertson (2 June 1886 – 23 March 1966) was an English-born medical scientist who pioneered the idea of blood banks in the "blood depots" he established in 1917 during service in France with the US Army Medical Corps.
__TOC__
Lif ...
, a medical researcher and U.S. Army officer, was attached to the RAMC in 1917, where he became instrumental in establishing the first blood banks in preparation for the anticipated Third Battle of Ypres
The Third Battle of Ypres (german: link=no, Dritte Flandernschlacht; french: link=no, Troisième Bataille des Flandres; nl, Derde Slag om Ieper), also known as the Battle of Passchendaele (), was a campaign of the First World War, fought by t ...
. He used sodium citrate as the anticoagulant; blood was extracted from punctures in the vein
Veins are blood vessels in humans and most other animals that carry blood towards the heart. Most veins carry deoxygenated blood from the tissues back to the heart; exceptions are the pulmonary and umbilical veins, both of which carry oxygenat ...
and was stored in bottles at British and American Casualty Clearing Stations along the Front. Robertson also experimented with preserving separated red blood cell
Red blood cells (RBCs), also referred to as red cells, red blood corpuscles (in humans or other animals not having nucleus in red blood cells), haematids, erythroid cells or erythrocytes (from Greek ''erythros'' for "red" and ''kytos'' for "holl ...
s in iced bottles. Geoffrey Keynes, a British surgeon, developed a portable machine that could store blood to enable transfusions to be carried out more easily.
Expansion
 The secretary of the British Red Cross, Percy Oliver, established the world's first blood-donor service in 1921. In that year, Oliver was contacted by
The secretary of the British Red Cross, Percy Oliver, established the world's first blood-donor service in 1921. In that year, Oliver was contacted by King's College Hospital
King's College Hospital is a major teaching hospital and major trauma centre in Denmark Hill, Camberwell in the London Borough of Lambeth, referred to locally and by staff simply as "King's" or abbreviated internally to "KCH". It is managed b ...
, where they were in urgent need of a blood donor.
After providing a donor, Oliver set about organizing a system for the voluntary registration of blood donors at clinics around London, with Sir Geoffrey Keynes appointed as a medical adviser. Volunteers were subjected to a series of physical tests to establish their blood group
A blood type (also known as a blood group) is a classification of blood, based on the presence and absence of antibodies and inherited antigenic substances on the surface of red blood cells (RBCs). These antigens may be proteins, carbohydrates ...
. The London Blood Transfusion Service was free of charge and expanded rapidly in its first few years of operation. By 1925 it was providing services for almost 500 patients; it was incorporated into the structure of the British Red Cross in 1926. Similar systems developed in other cities, including Sheffield
Sheffield is a city in South Yorkshire, England, whose name derives from the River Sheaf which runs through it. The city serves as the administrative centre of the City of Sheffield. It is historically part of the West Riding of Yorkshire a ...
, Manchester
Manchester () is a city in Greater Manchester, England. It had a population of 552,000 in 2021. It is bordered by the Cheshire Plain to the south, the Pennines to the north and east, and the neighbouring city of Salford to the west. The t ...
and Norwich, and the service's work began to attract international attention. France, Germany, Austria, Belgium, Australia and Japan established similar services.
Alexander Bogdanov founded an academic institution devoted to the science of blood transfusion in Moscow
Moscow ( , US chiefly ; rus, links=no, Москва, r=Moskva, p=mɐskˈva, a=Москва.ogg) is the capital and largest city of Russia. The city stands on the Moskva River in Central Russia, with a population estimated at 13.0 millio ...
in 1925. Bogdanov was motivated, at least in part, by a search for eternal youth, and remarked with satisfaction on the improvement of his eyesight, suspension of balding, and other positive symptoms after receiving 11 transfusions of whole blood
Whole blood (WB) is human blood from a standard blood donation. It is used in the treatment of massive bleeding, in exchange transfusion, and when people donate blood to themselves. One unit of whole blood (~517 mls) brings up hemoglobin level ...
. Bogdanov died in 1928 as a result of one of his experiments, when the blood of a student with malaria
Malaria is a mosquito-borne infectious disease that affects humans and other animals. Malaria causes symptoms that typically include fever, tiredness, vomiting, and headaches. In severe cases, it can cause jaundice, seizures, coma, or death. S ...
and tuberculosis
Tuberculosis (TB) is an infectious disease usually caused by '' Mycobacterium tuberculosis'' (MTB) bacteria. Tuberculosis generally affects the lungs, but it can also affect other parts of the body. Most infections show no symptoms, i ...
was given to him in a transfusion. Following Bogdanov's lead, Vladimir Shamov and Sergei Yudin in the USSR pioneered the transfusion of cadaveric blood from recently deceased donors. Yudin performed such a transfusion successfully for the first time on March 23, 1930, and reported his first seven clinical transfusions with cadaveric blood at the Fourth Congress of Ukrainian Surgeons at Kharkiv in September. However, this method was never used widely, even in the Soviet Union. Nevertheless, the Soviet Union was the first to establish a network of facilities to collect and store blood for use in transfusions at hospitals.
 Frederic Durán-Jordà established one of the earliest blood banks during the
Frederic Durán-Jordà established one of the earliest blood banks during the Spanish Civil War
The Spanish Civil War ( es, Guerra Civil Española)) or The Revolution ( es, La Revolución, link=no) among Nationalists, the Fourth Carlist War ( es, Cuarta Guerra Carlista, link=no) among Carlists, and The Rebellion ( es, La Rebelión, link ...
in 1936. Duran joined the Transfusion Service at the Barcelona Hospital at the start of the conflict, but the hospital was soon overwhelmed by the demand for blood and the paucity of available donors. With support from the Department of Health of the Spanish Republican Army, Duran established a blood bank for the use of wounded soldiers and civilians. The 300–400 mL of extracted blood was mixed with 10% citrate solution in a modified Duran Erlenmeyer flask. The blood was stored in a sterile glass enclosed under pressure at 2 °C. During 30 months of work, the Transfusion Service of Barcelona registered almost 30,000 donors, and processed 9,000 liters of blood.
In 1937 Bernard Fantus, director of therapeutics at the Cook County Hospital
The John H. Stroger Jr. Hospital of Cook County (formerly Cook County Hospital) is a public hospital in Chicago, Illinois, United States. It is part of the Cook County Health and Hospital System, along with Provident Hospital of Cook County and ...
in Chicago
(''City in a Garden''); I Will
, image_map =
, map_caption = Interactive Map of Chicago
, coordinates =
, coordinates_footnotes =
, subdivision_type = Country
, subdivision_name ...
, established the first hospital blood-bank in the United States
The United States of America (U.S.A. or USA), commonly known as the United States (U.S. or US) or America, is a country primarily located in North America. It consists of 50 states, a federal district, five major unincorporated territori ...
. In setting up a hospital laboratory that preserved, refrigerated and stored donor blood, Fantus originated the term "blood bank". Within a few years, hospital and community blood-banks were established across the United States.
Frederic Durán-Jordà fled to Britain in 1938 and worked with Dr Janet Vaughan at the Royal Postgraduate Medical School
The Royal Postgraduate Medical School (RPMS) was an independent medical school, based primarily at Hammersmith Hospital in west London. In 1988, the school merged with the Institute of Obstetrics & Gynaecology, and in 1997 became part of Imperial ...
at Hammersmith Hospital to establish a system of national blood banks in London. With the outbreak of war
War is an intense armed conflict between states, governments, societies, or paramilitary groups such as mercenaries, insurgents, and militias. It is generally characterized by extreme violence, destruction, and mortality, using regular o ...
appearing imminent in 1938, the War Office
The War Office was a department of the British Government responsible for the administration of the British Army between 1857 and 1964, when its functions were transferred to the new Ministry of Defence (MoD). This article contains text from ...
created the Army Blood Supply Depot (ABSD) in Bristol, headed by Lionel Whitby and in control of four large blood-depots around the country. British policy through the war was to supply military personnel with blood from centralized depots, in contrast to the approach taken by the Americans and Germans where troops at the front were bled to provide required blood. The British method proved more successful in adequately meeting all requirements, and over 700,000 donors were bled over the course of the war. This system evolved into the National Blood Transfusion Service established in 1946, the first national service to be implemented.
Stories tell of Nazis in Eastern Europe during World War II using captive children as repeated involuntary blood-donors.
Medical advances
A blood-collection program was initiated in the US in 1940 and Edwin Cohn pioneered the process of blood fractionation. He worked out the techniques for isolating the serum albumin fraction of blood plasma, which is essential for maintaining the osmotic pressure in theblood vessel
The blood vessels are the components of the circulatory system that transport blood throughout the human body. These vessels transport blood cells, nutrients, and oxygen to the tissues of the body. They also take waste and carbon dioxide away ...
s, preventing their collapse.
Gordon R. Ward, writing in the correspondence columns of the '' British Medical Journal'', proposed the use of blood plasma as a substitute for whole blood and for transfusion purposes as early as 1918. At the onset of World War II
World War II or the Second World War, often abbreviated as WWII or WW2, was a world war that lasted from 1939 to 1945. It involved the vast majority of the world's countries—including all of the great powers—forming two opposing ...
, liquid plasma was used in Britain. A large project, known as "Blood for Britain", began in August 1940 to collect blood in New York City
New York, often called New York City or NYC, is the most populous city in the United States. With a 2020 population of 8,804,190 distributed over , New York City is also the most densely populated major city in the Un ...
hospitals for the export of plasma to Britain
Britain most often refers to:
* The United Kingdom, a sovereign state in Europe comprising the island of Great Britain, the north-eastern part of the island of Ireland and many smaller islands
* Great Britain, the largest island in the United King ...
. A freeze-dried
Freeze drying, also known as lyophilization or cryodesiccation, is a low temperature dehydration process that involves freezing the product and lowering pressure, removing the ice by sublimation. This is in contrast to dehydration by most conve ...
plasma package was developed by the Surgeons General of the Army and Navy, working with the National Research Council National Research Council may refer to:
* National Research Council (Canada), sponsoring research and development
* National Research Council (Italy), scientific and technological research, Rome
* National Research Council (United States), part of ...
, which reduced breakage and made transportation, packaging, and storage much simpler.
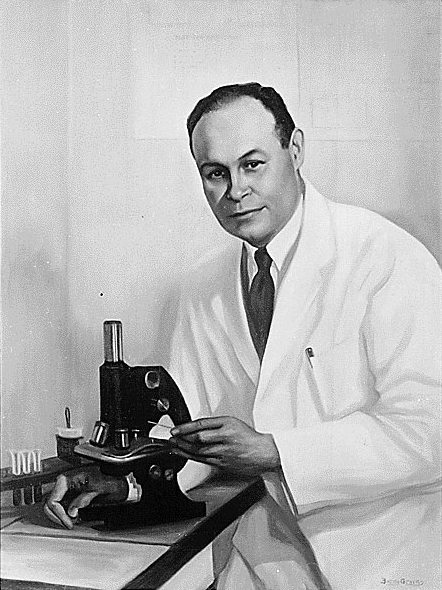 The resulting dried plasma package came in two tin cans containing 400 mL bottles. One bottle contained enough
The resulting dried plasma package came in two tin cans containing 400 mL bottles. One bottle contained enough distilled water
Distilled water is water that has been boiled into vapor and condensed back into liquid in a separate container. Impurities in the original water that do not boil below or near the boiling point of water remain in the original container. Thus, di ...
to reconstitute the dried plasma contained within the other bottle. In about three minutes, the plasma would be ready to use and could stay fresh for around four hours. Dr. Charles R. Drew was appointed medical supervisor, and he was able to transform the test-tube methods into the first successful technique for mass production.
Another important breakthrough came in 1937–40 when Karl Landsteiner (1868–1943), Alex Wiener, Philip Levine, and R.E. Stetson discovered the Rhesus blood group system
The Rh blood group system is a human blood group system. It contains proteins on the surface of red blood cells. After the ABO blood group system, it is the most likely to be involved in transfusion reactions. The Rh blood group system consists ...
, which was found to be the cause of the majority of transfusion reactions up to that time. Three years later, the introduction by J.F. Loutit and Patrick L. Mollison of acid–citrate–dextrose (ACD) solution, which reduced the volume of anticoagulant, permitted transfusions of greater volumes of blood and allowed longer-term storage.
Carl Walter and W.P. Murphy Jr. introduced the plastic bag for blood collection in 1950. Replacing breakable glass
Glass is a non-crystalline, often transparent, amorphous solid that has widespread practical, technological, and decorative use in, for example, window panes, tableware, and optics. Glass is most often formed by rapid cooling ( quenching ...
bottles with durable plastic bags made from PVC allowed for the evolution of a collection system capable of safe and easy preparation of multiple blood components from a single unit of whole blood.
In the field of cancer surgery
Surgical oncology is the branch of surgery applied to oncology; it focuses on the surgical management of tumors, especially cancerous tumors.
As one of several modalities in the management of cancer, the specialty of surgical oncology has evolve ...
, the replacement of massive blood-loss became a major problem. The cardiac-arrest rate was high. In 1963 C. Paul Boyan and William S. Howland discovered that the temperature of the blood and the rate of infusion greatly affected survival rates, and introduced blood warming to surgery.
Further extending the shelf-life of stored blood up to 42 days was an anticoagulant preservative, CPDA-1, introduced in 1979, which increased the blood supply and facilitated resource-sharing among blood banks.
about 15 million units of blood products were transfused per year in the United States. By 2013 the number had declined to about 11 million units, because of the shift towards laparoscopic surgery
Laparoscopy () is an operation performed in the abdomen or pelvis using small incisions (usually 0.5–1.5 cm) with the aid of a camera. The laparoscope aids diagnosis or therapeutic interventions with a few small cuts in the abdomen.Medli ...
and other surgical advances and studies that have shown that many transfusions were unnecessary. For example, the standard of care reduced the amount of blood transfused in one case from 750 to 200 mL.
Special populations
Neonate
To ensure the safety of blood transfusion to pediatric patients, hospitals are taking additional precautions to avoid infection and prefer to use specially tested pediatric blood units that are guaranteed negative for Cytomegalovirus. Most guidelines recommend the provision of CMV-negative blood components and not simply leukoreduced components for newborns or low birthweight infants in whom the immune system is not fully developed. These specific requirements place additional restrictions on blood donors who can donate for neonatal use. Neonatal transfusions typically fall into one of two categories: * "Top-up" transfusions, to replace losses due to investigational losses and correction of anemia. * Exchange (or partial exchange) transfusions are done for removal of bilirubin, removal of antibodies and replacement of red cells (e.g., for anemia secondary to thalassemias and other hemoglobinopathies).Significant blood loss
A ''massive transfusion protocol'' is used when significant blood loss is present such as in major trauma, when more than ten units of blood are needed. Packed red blood cells, fresh frozen plasma, and platelets are generally administered. Typically higher ratios of fresh frozen plasma and platelets are given relative topacked red blood cells
Packed red blood cells, also known as packed cells, are red blood cells that have been separated for blood transfusion. The packed cells are typically used in anemia that is either causing symptoms or when the hemoglobin is less than usually 70� ...
.
Unknown blood type
Because blood type O negative is compatible with anyone, it is often overused and in short supply., which cites * According to the Association for the Advancement of Blood and Biotherapies, the use of this blood should be restricted to persons with O negative blood, as nothing else is compatible with them, and women who might be pregnant and for whom it would be impossible to do blood group testing before giving them emergency treatment. Whenever possible, the AABB recommends that O negative blood be conserved by using blood type testing to identify a less scarce alternative.Religious objections
Jehovah's Witnesses may object to blood transfusions because of their belief that blood is sacred.Research into alternatives
Although there are clinical situations where transfusion with red blood cells is the only clinically appropriate option, clinicians look at whether alternatives are feasible. This can be due to several reasons, such as patient safety, economic burden or scarcity of blood. Guidelines recommend blood transfusions should be reserved for patients with or at risk of cardiovascular instability due to the degree of their anaemia. In these casesparenteral iron
Iron supplements, also known as iron salts and iron pills, are a number of iron formulations used to treat and prevent iron deficiency including iron deficiency anemia. For prevention they are only recommended in those with poor absorption, ...
is recommended.
Thus far, there are no available ''oxygen-carrying'' blood substitutes
A blood substitute (also called artificial blood or blood surrogate) is a substance used to mimic and fulfill some functions of biological blood. It aims to provide an alternative to blood transfusion, which is transferring blood or blood-based ...
, which is the typical objective of a blood (RBC) transfusion; however, there are widely available non-blood ''volume expanders'' for cases where only volume restoration is required. These are helping doctors and surgeons avoid the risks of disease transmission and immune suppression, address the chronic blood donor shortage, and address the concerns of Jehovah's Witnesses and others who have religious objections to receiving transfused blood.
The research in this area is ongoing. A number of blood substitutes have been explored, but thus far they all have serious limitations. Most attempts to find a suitable alternative to blood thus far have concentrated on cell-free hemoglobin solutions. Blood substitutes could make transfusions more readily available in emergency medicine and in pre-hospital EMS care. If successful, such a blood substitute could save many lives, particularly in trauma where massive blood loss results. Hemopure, a hemoglobin-based therapy, is approved for use in South Africa
South Africa, officially the Republic of South Africa (RSA), is the Southern Africa, southernmost country in Africa. It is bounded to the south by of coastline that stretch along the Atlantic Ocean, South Atlantic and Indian Oceans; to the ...
.
Other uses
Minor blood transfusions are used by a minority of nyaope drug addicts in South Africa to economically share the high the drug induces in a practice colloquially known as ''Bluetoothing'', named after the wireless technology of the same name.Veterinary use
Veterinarians also administer transfusions to other animals. Variousspecies
In biology, a species is the basic unit of classification and a taxonomic rank of an organism, as well as a unit of biodiversity. A species is often defined as the largest group of organisms in which any two individuals of the appropriate s ...
require different levels of testing to ensure a compatible match. For example, cat
The cat (''Felis catus'') is a domestic species of small carnivorous mammal. It is the only domesticated species in the family Felidae and is commonly referred to as the domestic cat or house cat to distinguish it from the wild members of ...
s have 3 known blood types, cattle
Cattle (''Bos taurus'') are large, domesticated, cloven-hooved, herbivores. They are a prominent modern member of the subfamily Bovinae and the most widespread species of the genus ''Bos''. Adult females are referred to as cows and adult ma ...
have 11, dog
The dog (''Canis familiaris'' or ''Canis lupus familiaris'') is a domesticated descendant of the wolf. Also called the domestic dog, it is derived from the extinct Pleistocene wolf, and the modern wolf is the dog's nearest living relative. Do ...
s have 13, pigs have 16, and horse
The horse (''Equus ferus caballus'') is a domesticated, one-toed, hoofed mammal. It belongs to the taxonomic family Equidae and is one of two extant subspecies of ''Equus ferus''. The horse has evolved over the past 45 to 55 million yea ...
s have 34. However, in many species (especially horses and dogs), cross matching is not required before the ''first'' transfusion, as antibodies against non-self cell surface antigens are not expressed constitutively – i.e. the animal has to be sensitized before it will mount an immune response against the transfused blood.
The rare and experimental practice of inter-species blood transfusions is a form of xenograft
Xenotransplantation (''xenos-'' from the Greek meaning "foreign" or strange), or heterologous transplant, is the transplantation of living cells, tissues or organs from one species to another. Such cells, tissues or organs are called xenograf ...
.
See also
* Anemia * Arnault Tzanck * Blood transfusion in Sri Lanka * Blood type (non-human) * Xenotransfusion * Young blood transfusion, a pseudoscientific practice involving the transfusion of blood taken from young donors to older recipients that is claimed to have health benefits * AIDSReferences
Further reading
* *Milk as a Substitute for Blood Transfusion
, historical account,
Scientific American
''Scientific American'', informally abbreviated ''SciAm'' or sometimes ''SA'', is an American popular science magazine. Many famous scientists, including Albert Einstein and Nikola Tesla, have contributed articles to it. In print since 1845, it ...
, 13 July 1878, p. 19
External links
Transfusion Evidence Library
searchable source of evidence for transfusion medicine.
Blood transfusion societies
*American Association of Blood Banks
American(s) may refer to:
* American, something of, from, or related to the United States of America, commonly known as the "United States" or "America"
** Americans, citizens and nationals of the United States of America
** American ancestry, pe ...
(AABB)
British Blood Transfusion Society
(BBTS)
International Society of Blood Transfusion
(ISBT)
Books
''Blood Groups and Red Cell Antigens''
Free online book at
NCBI
The National Center for Biotechnology Information (NCBI) is part of the United States National Library of Medicine (NLM), a branch of the National Institutes of Health (NIH). It is approved and funded by the government of the United States. The ...
Bookshelf ID: NBK2261
''Handbook of Transfusion Medicine''
Free book published in the UK 5th edition
Guidelines
American Association of Blood Banks Clinical Practice Guidelines
Australian National Blood Authority Patient Blood Management Guidelines
* ttps://www.nice.org.uk/guidance/ng24 National Institute for Health and Care Excellence Blood Transfusion GuidanceUK Guidance for transfusion.
Canadian Blood Transfusion Guidelines
German Medical Association Guidelines (English)
published 2014.
Patient information
Blood Transfusion Leaflets
(NHS Blood and Transplant)
Blood Transfusion Leaflets
(Welsh Blood Service)
Blood Transfusion Information
(Scotland)
Blood Transfusion Information
(Australia)
(American Cancer Society) {{Authority control Transfusion medicine Hematology Blood