radiofrequency ablation on:
[Wikipedia]
[Google]
[Amazon]
Radiofrequency ablation (RFA), also called fulguration, is a medical procedure in which part of the
 RFA may be performed to treat tumors in the lung, liver, kidney, and bone, as well as other body organs less commonly. Once the diagnosis of tumor is confirmed, a needle-like RFA probe is placed inside the tumor. The radiofrequency waves passing through the probe increase the temperature within tumor tissue, which results in destruction of the tumor. RFA can be used with small tumors, whether these arose within the organ (primary tumors) or spread to the organ (
RFA may be performed to treat tumors in the lung, liver, kidney, and bone, as well as other body organs less commonly. Once the diagnosis of tumor is confirmed, a needle-like RFA probe is placed inside the tumor. The radiofrequency waves passing through the probe increase the temperature within tumor tissue, which results in destruction of the tumor. RFA can be used with small tumors, whether these arose within the organ (primary tumors) or spread to the organ (
 Radiofrequency energy is used in heart tissue or normal parts to destroy abnormal electrical pathways that are contributing to a
Radiofrequency energy is used in heart tissue or normal parts to destroy abnormal electrical pathways that are contributing to a
electrical conduction system of the heart
The cardiac conduction system (CCS, also called the electrical conduction system of the heart) transmits the Cardiac action potential, signals generated by the sinoatrial node – the heart's Cardiac pacemaker, pacemaker, to cause the heart musc ...
, tumor
A neoplasm () is a type of abnormal and excessive growth of tissue. The process that occurs to form or produce a neoplasm is called neoplasia. The growth of a neoplasm is uncoordinated with that of the normal surrounding tissue, and persists ...
, sensory nerve
A sensory nerve, or afferent nerve, is a nerve that contains exclusively afferent nerve fibers. Nerves containing also motor fibers are called mixed nerve, mixed. Afferent nerve fibers in a sensory nerve carry sensory system, sensory information ...
s or a dysfunctional tissue is ablated using the heat generated from medium frequency
Medium frequency (MF) is the International Telecommunication Union, ITU designation for Radio frequency, radio frequencies (RF) in the range of 300 kilohertz (kHz) to 3 megahertz (MHz). Part of this band is the medium wave (MW) A ...
alternating current
Alternating current (AC) is an electric current that periodically reverses direction and changes its magnitude continuously with time, in contrast to direct current (DC), which flows only in one direction. Alternating current is the form in w ...
(in the range of 350–500 kHz). RFA is generally conducted in the outpatient
A patient is any recipient of health care services that are performed by healthcare professionals. The patient is most often ill or injured and in need of treatment by a physician, nurse, optometrist, dentist, veterinarian, or other healt ...
setting, using either a local anesthetic
A local anesthetic (LA) is a medication that causes absence of all sensation (including pain) in a specific body part without loss of consciousness, providing local anesthesia, as opposed to a general anesthetic, which eliminates all sensati ...
or twilight anesthesia. When it is delivered via catheter
In medicine, a catheter ( ) is a thin tubing (material), tube made from medical grade materials serving a broad range of functions. Catheters are medical devices that can be inserted in the body to treat diseases or perform a surgical procedure. ...
, it is called radiofrequency catheter ablation.
Two advantages of radio frequency
Radio frequency (RF) is the oscillation rate of an alternating electric current or voltage or of a magnetic, electric or electromagnetic field or mechanical system in the frequency range from around to around . This is roughly between the u ...
current (over previously used low frequency AC or pulses of DC) are that it does not directly stimulate nerves or heart muscle, and therefore can often be used without the need for general anesthesia
General anaesthesia (UK) or general anesthesia (US) is medically induced loss of consciousness that renders a patient unarousable even by painful stimuli. It is achieved through medications, which can be injected or inhaled, often with an analgesi ...
, and that it is specific for treating the desired tissue without significant collateral damage. Due to this, RFA is an alternative for eligible patients who have comorbidities or do not want to undergo surgery.
Documented benefits have led to RFA becoming widely used during the 21st century. RFA procedures are performed under image guidance (such as X-ray screening, CT scan
A computed tomography scan (CT scan), formerly called computed axial tomography scan (CAT scan), is a medical imaging technique used to obtain detailed internal images of the body. The personnel that perform CT scans are called radiographers or ...
or ultrasound
Ultrasound is sound with frequency, frequencies greater than 20 Hertz, kilohertz. This frequency is the approximate upper audible hearing range, limit of human hearing in healthy young adults. The physical principles of acoustic waves apply ...
) by an interventional pain specialist (such as an anesthesiologist), interventional radiologist, otolaryngologists, a gastrointestinal or surgical endoscopist, or a cardiac electrophysiologist, a subspecialty of cardiologists.
Tumors
 RFA may be performed to treat tumors in the lung, liver, kidney, and bone, as well as other body organs less commonly. Once the diagnosis of tumor is confirmed, a needle-like RFA probe is placed inside the tumor. The radiofrequency waves passing through the probe increase the temperature within tumor tissue, which results in destruction of the tumor. RFA can be used with small tumors, whether these arose within the organ (primary tumors) or spread to the organ (
RFA may be performed to treat tumors in the lung, liver, kidney, and bone, as well as other body organs less commonly. Once the diagnosis of tumor is confirmed, a needle-like RFA probe is placed inside the tumor. The radiofrequency waves passing through the probe increase the temperature within tumor tissue, which results in destruction of the tumor. RFA can be used with small tumors, whether these arose within the organ (primary tumors) or spread to the organ (metastases
Metastasis is a pathogenic agent's spreading from an initial or primary site to a different or secondary site within the host's body; the term is typically used when referring to metastasis by a cancerous tumor. The newly pathological sites, ...
). The suitability of RFA for a particular tumor depends on multiple factors.
RFA can usually be administered as an outpatient procedure, though may at times require a brief hospital stay. RFA may be combined with locally delivered chemotherapy to treat hepatocellular carcinoma (primary liver cancer). A method currently in phase III trials uses the low-level heat (hyperthermia) created by the RFA probe to trigger release of concentrated chemotherapeutic drugs from heat-sensitive liposomes in the margins around the ablated tissue as a treatment for hepatocellular carcinoma
Hepatocellular carcinoma (HCC) is the most common type of primary liver cancer in adults and is currently the most common cause of death in people with cirrhosis. HCC is the third leading cause of cancer-related deaths worldwide.
HCC most common ...
(HCC).
Radiofrequency ablation is also used in pancreatic cancer and bile duct cancer.
RFA has become increasingly important in the care of benign bone tumors, most notably osteoid osteomas. Since the procedure was first introduced for the treatment of osteoid osteomas in the 1990s, it has been shown in numerous studies to be less invasive and expensive, to result in less bone destruction and to have equivalent safety and efficacy to surgical techniques, with 66 to 95% of people reporting freedom from symptoms. While initial success rates with RFA are high, symptom recurrence after RFA treatment has been reported, with some studies demonstrating a recurrence rate similar to that of surgical treatment. RFA is also increasingly used in the palliative treatment of painful metastatic bone disease in people who are not eligible or do not respond to traditional therapies ( i.e. radiation therapy
Radiation therapy or radiotherapy (RT, RTx, or XRT) is a therapy, treatment using ionizing radiation, generally provided as part of treatment of cancer, cancer therapy to either kill or control the growth of malignancy, malignant cell (biology), ...
, chemotherapy
Chemotherapy (often abbreviated chemo, sometimes CTX and CTx) is the type of cancer treatment that uses one or more anti-cancer drugs (list of chemotherapeutic agents, chemotherapeutic agents or alkylating agents) in a standard chemotherapy re ...
, palliative surgery, bisphosphonate
Bisphosphonates are a class of drugs that prevent the loss of bone density, used to treat osteoporosis and similar diseases. They are the most commonly prescribed to treat osteoporosis.
Evidence shows that they reduce the risk of fracture in ...
s or analgesic medications).
Cardiology
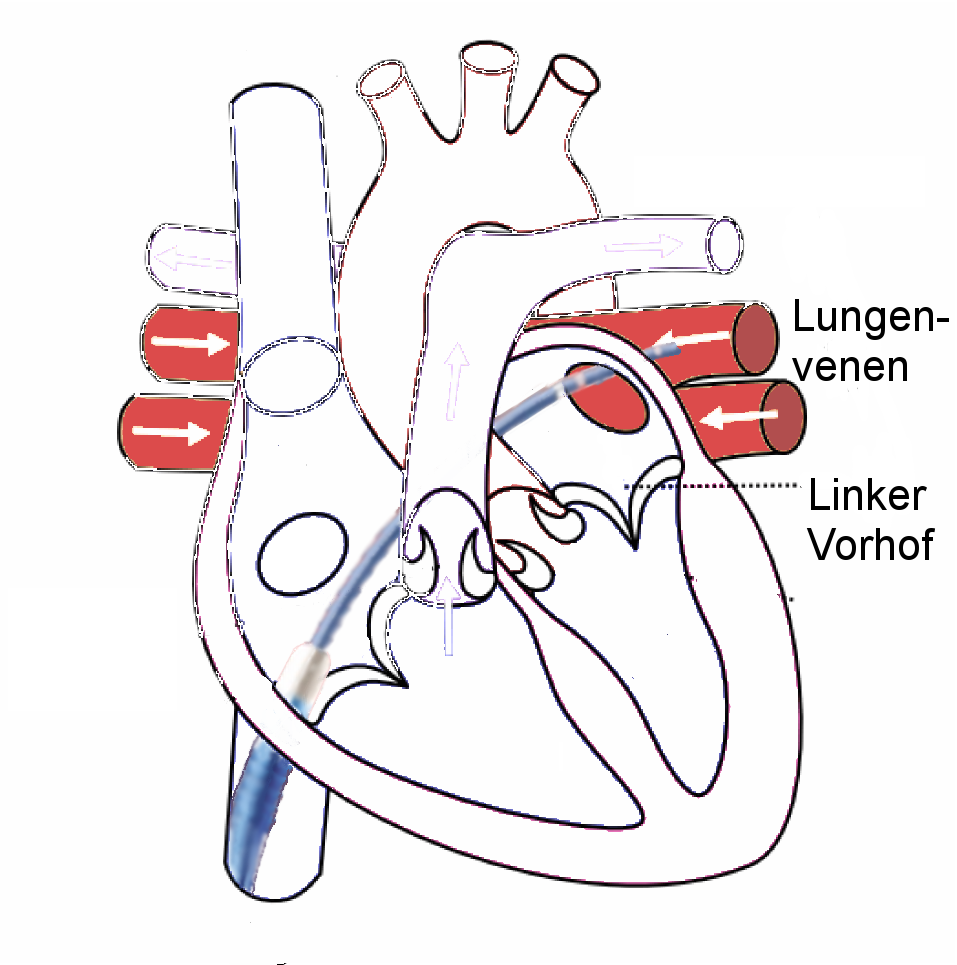
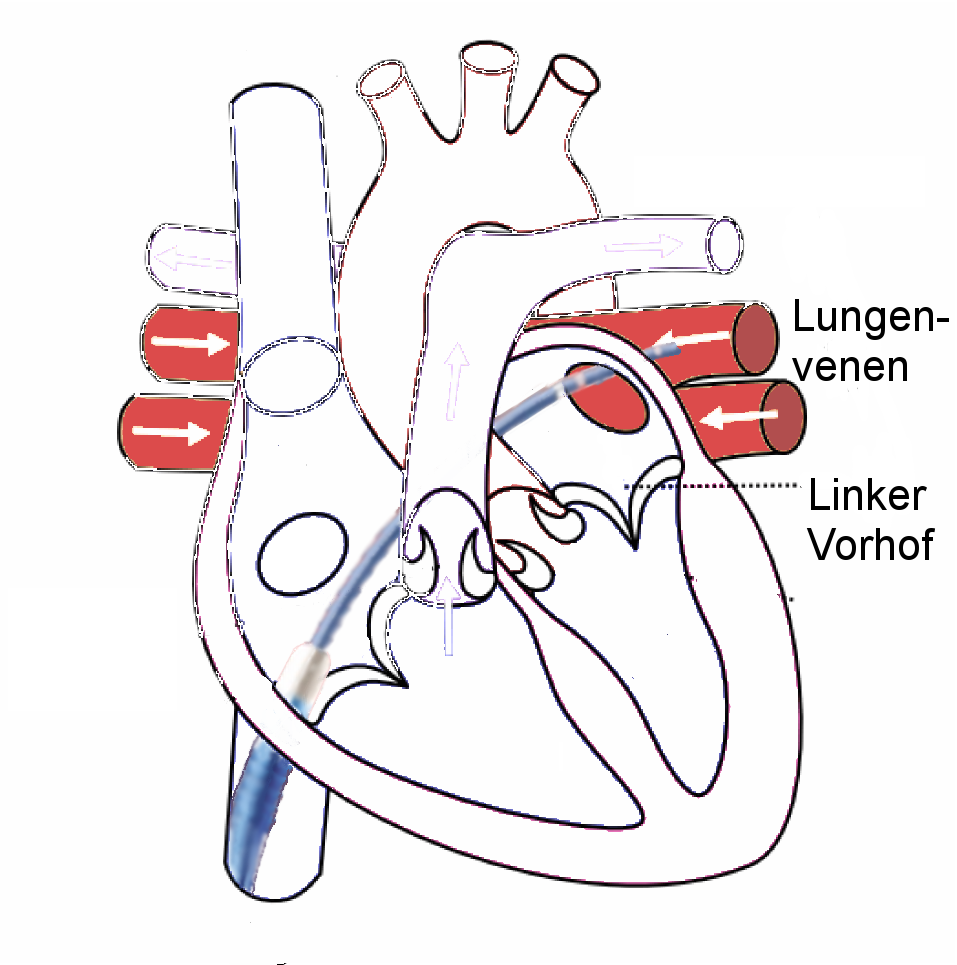 Radiofrequency energy is used in heart tissue or normal parts to destroy abnormal electrical pathways that are contributing to a
Radiofrequency energy is used in heart tissue or normal parts to destroy abnormal electrical pathways that are contributing to a cardiac arrhythmia
Arrhythmias, also known as cardiac arrhythmias, are irregularities in the heartbeat, including when it is too fast or too slow. Essentially, this is anything but normal sinus rhythm. A resting heart rate that is too fast – above 100 beat ...
. It is used in recurrent atrial flutter
Atrial flutter (AFL) is a common abnormal heart rhythm that starts in the atrial chambers of the heart. When it first occurs, it is usually associated with a fast heart rate and is classified as a type of supraventricular tachycardia (SVT). ...
(Afl), atrial fibrillation
Atrial fibrillation (AF, AFib or A-fib) is an Heart arrhythmia, abnormal heart rhythm (arrhythmia) characterized by fibrillation, rapid and irregular beating of the Atrium (heart), atrial chambers of the heart. It often begins as short periods ...
(AF), supraventricular tachycardia
Supraventricular tachycardia (SVT) is an umbrella term for fast heart rhythms arising from the upper part of the heart. This is in contrast to the other group of fast heart rhythms – ventricular tachycardia, which start within the lower cham ...
(SVT), atrial tachycardia
Atrial tachycardia is a type of heart rhythm problem in which the heart's electrical impulse comes from an ectopic pacemaker (that is, an abnormally located cardiac pacemaker) in the upper chambers ( atria) of the heart, rather than from the sin ...
, Multifocal Atrial Tachycardia (MAT) and some types of ventricular arrhythmia. The energy-emitting probe (electrode) is at the tip of a catheter which is placed into the heart, usually through a vein. This catheter is called the ablator. The practitioner first "maps" an area of the heart to locate the abnormal electrical activity (electrophysiology study
A cardiac electrophysiology study (EP test or EP study) is a Invasiveness of surgical procedures, minimally invasive procedure using catheters introduced through a vein or artery to record electrical activity from within the heart. This electric ...
) before the responsible tissue is eliminated. Radiofrequency ablation technique can be used in AF, either to block the atrioventricular node
The atrioventricular node (AV node, or Aschoff-Tawara node) electrically connects the heart's atria and ventricles to coordinate beating in the top of the heart; it is part of the electrical conduction system of the heart. The AV node lies at the ...
after implantation of a pacemaker or to block conduction within the left atrium
The atrium (; : atria) is one of the two upper chambers in the heart that receives blood from the circulatory system. The blood in the atria is pumped into the heart ventricles through the atrioventricular mitral and tricuspid heart valves.
...
, especially around the pulmonary veins
The pulmonary veins are the veins that transfer oxygenated blood from the lungs to the heart. The largest pulmonary veins are the four ''main pulmonary veins'', two from each lung that drain into the left atrium of the heart. The pulmonary ve ...
. Radiofrequency ablation for AF can be unipolar (one electrode) or bipolar (two electrodes). Although bipolar can be more successful, it is technically more difficult, resulting in unipolar being used more often. But bipolar is more effective in preventing recurrent atrial arrhythmias.
Ablation is now the standard treatment for SVT and typical atrial flutter, In some conditions, especially forms of intra-nodal re-entry (the most common type of SVT), also called atrioventricular nodal reentrant tachycardia or AVNRT, ablation can also be accomplished by cryoablation (tissue freezing using a coolant which flows through the catheter) which avoids the risk of complete heart block – a potential complication of radiofrequency ablation in this condition. Recurrence rates with cryoablation are higher, though. Microwave ablation, where tissue is ablated by the microwave energy "cooking" the adjacent tissue, and ultrasonic ablation, creating a heating effect by mechanical vibration, or laser ablation have also been developed but are not in widespread use.
Renal sympathetic denervation
A new indication for the use of radiofrequency technology has made news in the last few years.Hypertension
Hypertension, also known as high blood pressure, is a Chronic condition, long-term Disease, medical condition in which the blood pressure in the artery, arteries is persistently elevated. High blood pressure usually does not cause symptoms i ...
is a very common condition, with about 1 billion people over the world, nearly 75 million in the US alone. Complications of inadequately controlled hypertension are many and have both individual and global impact. Treatment options include medications, diet, exercise, weight reduction and meditation. Inhibition of the neural impulses that are believed to cause or worsen hypertension has been tried for a few decades. Surgical sympathectomy has helped but not without significant side effects. Therefore, the introduction of non-surgical means of renal denervation using a radiofrequency ablation catheter was enthusiastically welcomed. Although the initial use of radiofrequency-generated heat to ablate nerve endings in the renal arteries to aid in management of 'resistant hypertension' were encouraging, the most recent phase 3 studying looking at catheter-based renal denervation for the treatment of resistant hypertension failed to show any significant reduction in systolic blood pressure.
Aesthetics dermatology
Radiofrequency
Radio frequency (RF) is the oscillation rate of an alternating electric current or voltage or of a magnetic, electric or electromagnetic field or mechanical system in the frequency range from around to around . This is roughly between the upper ...
ablation is a dermatosurgical procedure by using various forms of alternating current. Types of radiofrequency are electrosection, electrocoagulation, electrodessication and fulguration. The use of radiofrequency ablation has obtained importance as it can be used to treat most of the skin lesions with minimal side effects and complications.
Varicose veins
Radiofrequency ablation is a minimally invasive procedure used in the treatment of varicose veins. It is an alternative to the traditional stripping operation. Under ultrasound guidance, a radiofrequency catheter is inserted into the abnormal vein and the vessel treated with radio-energy, resulting in closure of the involved vein. Radiofrequency ablation is used to treat thegreat saphenous vein
The great saphenous vein (GSV; ) or long saphenous vein is a large, subcutaneous, superficial vein of the human leg, leg. It is the longest vein in the body, running along the length of the lower limb, returning blood from the foot, human leg, le ...
, the small saphenous vein
The small saphenous vein (also short saphenous vein or lesser saphenous vein) is a relatively large superficial vein of the posterior leg.
Structure
The origin of the small saphenous vein (SSV) is where the dorsal vein from the fifth digit (smal ...
, and the perforator vein
Perforator veins are so called because they perforate the deep fascia of muscles, to connect the superficial veins to the deep veins where they drain.
Perforator veins play an essential role in maintaining normal blood draining. They have venous ...
s. The latter are connecting veins that transport blood from the superficial veins to the deep veins. Branch varicose veins are then usually treated with other minimally invasive procedures, such as ambulatory phlebectomy, sclerotherapy
Sclerotherapy (the word reflects the Greek ''skleros'', meaning ''hard'')
is a procedure used to treat blood vessel malformations ( vascular malformations) and also malformations of the lymphatic system. A medication is injected into the vessels ...
, or foam sclerotherapy. Currently, the VNUS ClosureRFS stylet is the only device specifically cleared by FDA for endovenous ablation of perforator veins.
The possibility of skin burn during the procedure is very small, because the large volumes (500 cc) of dilute Lidocaine (0.1%) tumescent anesthesia injected along the entire vein prior to the application of radiofrequency provide a heat sink that absorbs the heat created by the device. Early studies have shown a high success rate with low rates of complications.
Obstructive sleep apnea
RFA was first studied inobstructive sleep apnea
Obstructive sleep apnea (OSA) is the most common sleep-related breathing disorder and is characterized by recurrent episodes of complete or partial airway obstruction, obstruction of the respiratory tract#Upper respiratory tract, upper airway lea ...
(OSA) in a pig model. RFA has been recognized as a somnoplasty treatment option in selected situations by the American Academy of Otolaryngology but was not endorsed for general use in the American College of Physicians guidelines.
The clinical application of RFA in obstructive sleep apnea is reviewed in that main article, including controversies and potential advantages in selected medical situations.
Unlike other electrosurgical devices, RFA allows very specific treatment targeting of the desired tissue with a precise line of demarcation that avoids collateral damage, which is crucial in the head and neck region due to its high density of major nerves and blood vessels. RFA also does not require high temperatures. However, overheating from misapplication of RFA can cause harmful effects such as coagulation on the surface of the electrode, boiling within tissue that can leave "a gaping hole", tears, or even charring.
Pain management
Back
RFA, or rhizotomy, was developed by Nikolai Bogduk to treat chronic pain arising from thefacet joint
The facet joints (also zygapophysial joints, zygapophyseal, apophyseal, or Z-joints) are a set of synovial joint, synovial, plane joints between the articular processes of two adjacent vertebrae. There are two facet joints in each functional s ...
s in the lower (lumbar
In tetrapod anatomy, lumbar is an adjective that means of or pertaining to the abdominal segment of the torso, between the diaphragm (anatomy), diaphragm and the sacrum.
Naming and location
The lumbar region is sometimes referred to as the lowe ...
) back. Radiofrequency waves are used to produce heat on specifically identified nerves surrounding the facet joints called the lumbar medial branches of the dorsal ramus of the spinal nerves. By generating heat around the nerve, the nerve is ablated, thus destroying its ability to transmit signals to the brain.
The nerves to be ablated are identified through injections of local anesthesia (such as lidocaine
Lidocaine, also known as lignocaine and sold under the brand name Xylocaine among others, is a local anesthetic of the amino amide type. It is also used to treat ventricular tachycardia and ventricular fibrillation. When used for local anae ...
) around the medial branches prior to the RFA procedure to first confirm the diagnosis. If the local anesthesia
Local anesthesia is any technique to induce the absence of sense, sensation in a specific part of the body, generally for the aim of inducing local analgesia, i.e. local insensitivity to pain, although other local senses may be affected as well. ...
injections provide temporary pain relief, the injection is repeated a second time to confirm the diagnosis. Then RFA is performed on the nerve(s) that responded well to the injections.
RFA is a minimally invasive procedure which can usually be done in day-surgery clinics, going home shortly after completion of the procedure. The person is awake during the procedure, so risks associated with general anesthesia are avoided. Whether for back or knee pain, a drawback for this procedure is that nerves recover function over time, so the pain relief achieved lasts only temporarily (3–15 months) in most people.
Knees
Radiofrequency ablation of sensory nerves in the knee, also called ''genicular neurotomy'' or genicular RFA, is clinically preceded by confirming pain reduction upon anesthetizing the main knee sensory nerves in a test procedure called ''genicular nerve block''. Genicular nerve block is a short (10-30 minutes), outpatient procedure usually performed weeks before genicular RFA. The extent of pain reduction by injecting a local anesthetic, such as bupivacaine, at specific locations of the target genicular nerves, is self-assessed by the person for hours after the procedure, leading to confirmation with the physician of the need for RFA. In the procedure for genicular RFA, a guide cannula is first directed under local anesthesia and imaging (ultrasound
Ultrasound is sound with frequency, frequencies greater than 20 Hertz, kilohertz. This frequency is the approximate upper audible hearing range, limit of human hearing in healthy young adults. The physical principles of acoustic waves apply ...
or fluoroscopy
Fluoroscopy (), informally referred to as "fluoro", is an imaging technique that uses X-rays to obtain real-time moving images of the interior of an object. In its primary application of medical imaging, a fluoroscope () allows a surgeon to see t ...
) to each target genicular nerve, then the radiofrequency electrode is passed through the cannula, and the electrode tip is heated to about for one minute to cauterize a small segment of the nerve. The heat destroys that segment of the nerve, which is prevented from sending pain signals to the brain.
As of 2019, several hundred publications showed promise for substantial, long-term (6 months or longer) reduction of knee pain following genicular RFA.
The US Food and Drug Administration
The United States Food and Drug Administration (FDA or US FDA) is a List of United States federal agencies, federal agency of the United States Department of Health and Human Services, Department of Health and Human Services. The FDA is respo ...
had approved in 2017 a commercial device using cooled RFA, with effects lasting for up to a year of pain relief from knee arthritis. As of 2023, reviews of clinical outcomes indicated that efficacy for reducing knee pain was achieved by ablating three or more branches of the genicular nerve (one of the articular branches of the tibial nerve
The tibial nerve is a branch of the sciatic nerve. The tibial nerve passes through the popliteal fossa to pass below the arch of soleus.
Structure Popliteal fossa
The tibial nerve is the larger terminal branch of the sciatic nerve with root val ...
). Other sources indicate 4-5 genicular nerve targets may be justified for ablation to optimize pain relief, while a 2022 analysis indicated that as many as 10 genicular nerve targets for RFA would produce better long-term relief of knee pain.
Knee pain relief of 50% or more following genicular RFA may last from several months to two years, and can be repeated by the same outpatient procedure when pain recurs.
An anatomical study of cadaver
A cadaver, often known as a corpse, is a Death, dead human body. Cadavers are used by medical students, physicians and other scientists to study anatomy, identify disease sites, determine causes of death, and provide tissue (biology), tissue to ...
knees indicated that ultrasound-guided bony landmarks could be used to effectively target the superior medial geniculate nerve, superior lateral geniculate nerve, and inferior medial geniculate nerve the three nerves commonly targeted for knee RFA with average nerve-to-needle distances of 1.7, 3.2, and 1.8 mm, respectively.
Barrett's esophagus
Radiofrequency ablation has been shown to be a safe and effective treatment forBarrett's esophagus
Barrett's esophagus is a condition in which there is an abnormal ( metaplastic) change in the mucosal cells that line the lower part of the esophagus. The cells change from stratified squamous epithelium to simple columnar epithelium, intersper ...
. The balloon-based radiofrequency procedure was invented by Robert A. Ganz, Roger Stern and Brian Zelickson in 1999 (System and Method for Treating Abnormal Tissue in the Human Esophagus). While the person is sedated, a catheter is inserted into the esophagus and radiofrequency energy is delivered to the diseased tissue. This outpatient procedure typically lasts from fifteen to thirty minutes. Two months after the procedure, the physician performs an upper endoscopic examination to assess the esophagus for residual Barrett's esophagus. If any Barrett's esophagus is found, the disease can be treated with a focal RFA device. Between 80 and 90% or greater of people in numerous clinical trials have shown complete eradication of Barrett's esophagus in approximately two to three treatments with a favorable safety profile. The treatment of Barrett's esophagus by RFA is durable for up to 5 years.
Thyroid nodules
Radiofrequency ablation has been used successfully on benign thyroid nodules for decades, most notably in Europe, South America and Korea. In the United States, the FDA approved the use of RFA techniques for thyroid nodules in 2018. Since then, professional guidelines reflect its use as a viable treatment modality for thyroid nodules, and the procedure is increasingly applied.Timeline in the United States
- 2023: the American Thyroid Association issued the position statement "Thyroid ablative procedures provide valid alternative treatment strategies to conventional surgical management for a subset of patients with symptomatic benign thyroid nodules. - 2022: the American Association of Clinical Endocrinologists published an update in Endocrine Practice, stating that the "new image-guided minimally invasive approaches appear safe and effective alternatives when used appropriately and by trained professionals to treat symptomatic or enlarging thyroid masses". - 2018: FDA approved the RFA procedure for treatment of benign thyroid nodules.Procedure
The procedure is similar to a thyroid biopsy, although instead of using a needle to remove cells from the nodule, a probe delivers heat to the interior of the nodule that effectively cauterizes the tissue. Over the course of 3-6 months, the nodule will continue to shrink, typically achieving a 50-80% reduction total size. In order to qualify for an RFA procedure, a person must have a clearly benign thyroid nodule, usually proven by two fine needle aspiration biopsies. As of 2020, RFA is not recommended for the treatment ofmalignant
Malignancy () is the tendency of a medical condition to become progressively worse; the term is most familiar as a characterization of cancer.
A ''malignant'' tumor contrasts with a non-cancerous benign tumor, ''benign'' tumor in that a malig ...
thyroid nodules, although research into this topic is ongoing.
Other uses
RFA is also used in radiofrequency lesioning for vein closure in areas where intrusive surgery is contraindicated by trauma, and in liver resection to control bleeding (hemostasis) and facilitate the transection process. This process has also been used to treat TRAP sequence in multiple gestation pregnancies. This has an acceptable success rate for saving the 'pump' twin in recent studies compared to previous methods including laser photocoagulation. RFA is used to treatuterine fibroids
Uterine fibroids, also known as uterine leiomyomas, fibromyoma or fibroids, are leiomyoma, benign smooth muscle tumors of the uterus, part of the female reproductive system. Most people with fibroids have no symptoms while others may have dysm ...
using the heat energy of radio frequency waves to ablate the fibroid tissue. The Acessa device obtained FDA approval in 2012. The device is inserted via a laparoscopic probe and guided inside the fibroid tissue using an ultrasound probe. The heat shrinks the fibroids. Clinical data on the procedure show an average of 45% shrinkage.
RFA is also used in the treatment of Morton's neuroma where the outcome appears to be more reliable than alcohol injections.
See also
*Interventional radiology
Interventional radiology (IR) is a medical specialty that performs various minimally-invasive procedures using medical imaging guidance, such as Fluoroscopy, x-ray fluoroscopy, CT scan, computed tomography, magnetic resonance imaging, or ultraso ...
* Radio frequency
Radio frequency (RF) is the oscillation rate of an alternating electric current or voltage or of a magnetic, electric or electromagnetic field or mechanical system in the frequency range from around to around . This is roughly between the u ...
* Heart arrhythmia
Arrhythmias, also known as cardiac arrhythmias, are irregularities in the cardiac cycle, heartbeat, including when it is too fast or too slow. Essentially, this is anything but normal sinus rhythm. A resting heart rate that is too fast – ab ...
References
{{DEFAULTSORT:Radiofrequency Ablation Interventional radiology Vascular procedures Surgical oncology Medical terminology es:Ablación (Medicina)#Ablación por radiofrecuencia