Medical privacy, or health privacy, is the practice of maintaining the
security and confidentiality of
patient
A patient is any recipient of health care services that are performed by Health professional, healthcare professionals. The patient is most often Disease, ill or Major trauma, injured and in need of therapy, treatment by a physician, nurse, op ...
records. It involves both the conversational discretion of
health care providers
A health professional, healthcare professional (HCP), or healthcare worker (sometimes abbreviated as HCW) is a provider of health care treatment and advice based on formal training and experience. The field includes those who work as a nurse, phys ...
and the security of
medical record
The terms medical record, health record and medical chart are used somewhat interchangeably to describe the systematic documentation of a single patient's medical history and health care, care across time within one particular health care provide ...
s. The terms can also refer to the physical
privacy
Privacy (, ) is the ability of an individual or group to seclude themselves or information about themselves, and thereby express themselves selectively.
The domain of privacy partially overlaps with security, which can include the concepts of a ...
of patients from other patients and providers while in a
medical facility, and to
modesty in medical settings. Modern concerns include the degree of disclosure to
insurance companies
Insurance is a means of protection from financial loss in which, in exchange for a fee, a party agrees to compensate another party in the event of a certain loss, damage, or injury. It is a form of risk management, primarily used to protect ...
, employers, and other third parties. The advent of
electronic medical record
An electronic health record (EHR) is the systematized collection of electronically stored patient and population health information in a digital format. These records can be shared across different health care settings. Records are shared thro ...
s (EMR) and patient care management systems (PCMS) have raised new concerns about privacy, balanced with efforts to reduce duplication of services and
medical errors.
Most developed countries including Australia, Canada, Turkey, the United Kingdom, the United States, New Zealand, and the Netherlands have enacted laws protecting people's medical health privacy. However, many of these health-securing privacy laws have proven less effective in practice than in theory.
In 1996, the United States passed the
Health Insurance Portability and Accountability Act (HIPAA) which aimed to increase privacy precautions within medical institutions.
History
The history of medical privacy traces back to the Hippocratic Oath, which mandates the secrecy of information obtained while helping a patient.
Before the technological boom, medical institutions relied on the paper medium to file individual medical data. Nowadays, more and more information is stored within
electronic database
A bibliographic database is a database of bibliographic records. This is an organised online collection of references to published written works like journal and newspaper articles, conference proceedings, reports, government and legal publicati ...
s. Research indicates that storing information on paper is safer because it is more difficult to physically steal, whereas digital records are vulnerable to hacker access.
In the early 1990s, to address healthcare privacy issues, researchers explored using credit cards and smart cards to enable secure access to medical information, aiming to mitigate fears of data theft. The "smart" card allowed the storage and processing of information to be stored in a singular microchip, yet people were fearful of having so much information stored in a single spot that could easily be accessed.
This "smart" card included an individual's
social security number
In the United States, a Social Security number (SSN) is a nine-digit number issued to United States nationality law, U.S. citizens, Permanent residence (United States), permanent residents, and temporary (working) residents under section 205(c)(2 ...
as an important piece of identification that can lead to
identity theft
Identity theft, identity piracy or identity infringement occurs when someone uses another's personal identifying information, like their name, identifying number, or credit card number, without their permission, to commit fraud or other crimes. ...
if databases are breached.
Additionally, there was the fear that people would target these medical cards because they have information that can be of value to many different third parties, including employers, pharmaceutical companies, drug marketers, and insurance reviewers.
In response to the lack of medical privacy, there was a movement to create better medical privacy protection, but nothing has been officially passed. The
Medical Information Bureau was thus created to prevent insurance fraud, yet it has since become a significant source of medical information for over 750 life insurance companies; thus, it is very dangerous as it is a target of privacy breaches.
Although the electronic filing system of medical information has increased efficiency and administration costs have been reduced, there are negative aspects to consider. The electronic filing system allows for individual information to be more susceptible to outsiders; even though their information is stored on a singular card. Therefore, the medical card serves as a false sense of security as it does not protect their information completely.
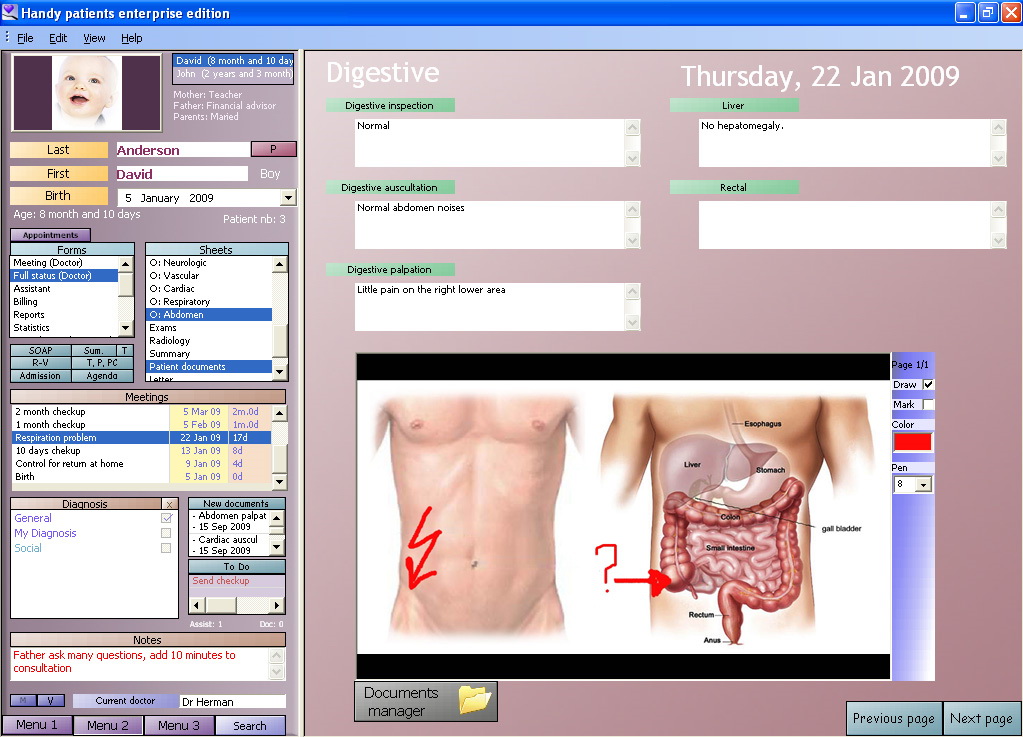
Patient care management systems (PCMS)
With the technological boom, there has been an expansion of the record filing system and many hospitals have therefore adopted new PCMS.
PCMS store large amounts of medical records, and hold the personal data of many individuals. These have become critical to the efficiency of storing medical information because of the high volumes of paperwork, the ability to quickly share information between medical institutions, and the increased mandatory reporting to the government.
PCMS have ultimately increased the productivity of data record utilization and have created a large dependence on technology within the medical field.
It has also led to social and ethical issues because basic
human rights
Human rights are universally recognized Morality, moral principles or Social norm, norms that establish standards of human behavior and are often protected by both Municipal law, national and international laws. These rights are considered ...
are considered to be violated by the PCMS, since hospitals and health information services are now more likely to
share information with third-party companies.
Thus, there needs to be a reformation to specify which hospital personnel have the access to medical records. This has led to the discussion of privacy rights and created safeguards that will help data keepers understand situations where it is ethical to share an individual's medical information, provide ways for individuals to gain access to their own records, and determine who has ownership of those records.
Additionally, it is used to ensure that a person's identity is kept confidential for research or statistical purposes and to understand the process to make individuals aware that their health information is being used.
Thus, a balance between privacy and confidentiality must be kept in order to limit the amount of information disclosed and protect patients' rights by safeguarding sensitive information from third parties.
Electronic Medical Records (EMR)
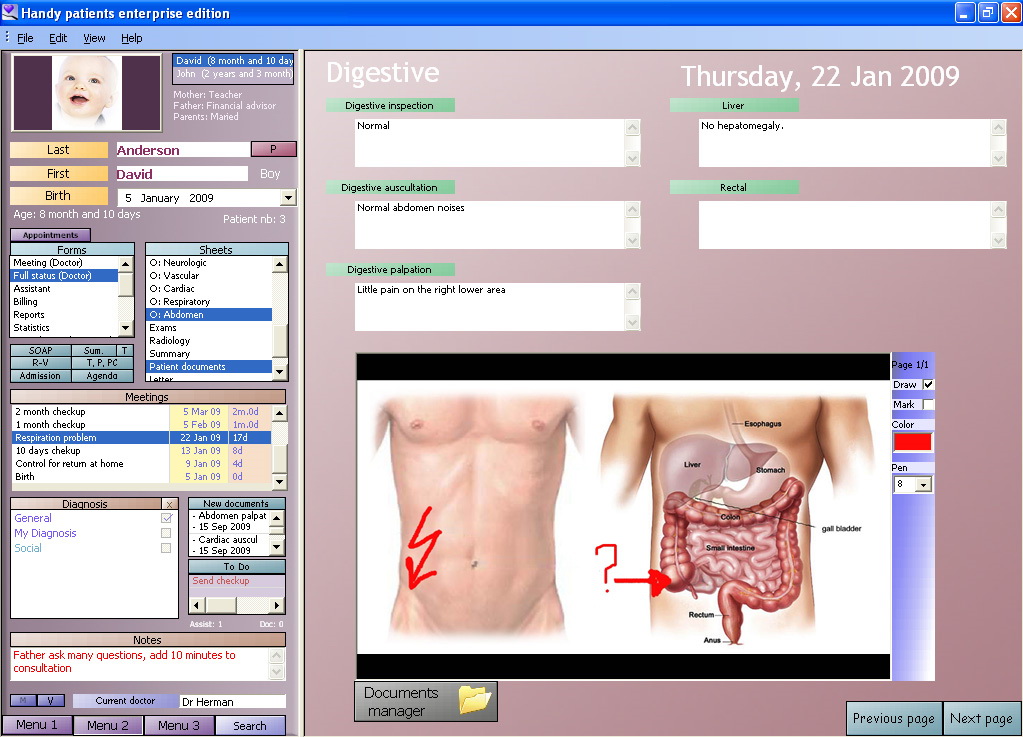
Electronic medical record
An electronic health record (EHR) is the systematized collection of electronically stored patient and population health information in a digital format. These records can be shared across different health care settings. Records are shared thro ...
s are a more efficient way of storing medical information, yet there are many negative aspects of this type of filing system as well. Hospitals are willing to adopt this type of filing system only if they are able to ensure that the private information of their patients is sufficiently protected.
Researchers have found that U.S. state legislation and regulation of medical privacy laws reduce the number of hospitals that adopt EMR by more than 24%.
This is due to decreasing positive network externalities that are created by additional state protections.
With increases in restrictions against the diffusion of medical information, hospitals have neglected to adopt the new EMRs because privacy laws restrict health information exchanges. With decreasing numbers of medical institutions adopting the EMR filing system, the U.S. government's plan of a national health network has not been fully recognized.
The national network will ultimately cost US$156 billion in investments, yet in order for this to happen, the U.S. government needs to place a higher emphasis on protecting individual privacy.
Many politicians and business leaders find that EMRs allow for more efficiency in both time and money, yet they neglect to address the decreasing privacy protections, demonstrating the significant trade-off between EMRs and individual privacy.
Privacy and Electronic Health Records (EHR)
The three goals of
information security
Information security is the practice of protecting information by mitigating information risks. It is part of information risk management. It typically involves preventing or reducing the probability of unauthorized or inappropriate access to data ...
, including electronic information security, are
confidentiality
Confidentiality involves a set of rules or a promise sometimes executed through confidentiality agreements that limits the access to or places restrictions on the distribution of certain types of information.
Legal confidentiality
By law, la ...
,
integrity
Integrity is the quality of being honest and having a consistent and uncompromising adherence to strong moral and ethical principles and values.
In ethics, integrity is regarded as the honesty and Honesty, truthfulness or of one's actions. Integr ...
, and
availability
In reliability engineering, the term availability has the following meanings:
* The degree to which a system, subsystem or equipment is in a specified operable and committable state at the start of a mission, when the mission is called for at ...
. Organizations are attempting to meet these goals, referred to as the
C.I.A. Triad, which is the "practice of defending information from unauthorized access, use, disclosure, disruption, modification, inspection, recording or destruction."
In a 2004 editorial in the ''
Washington Post
''The Washington Post'', locally known as ''The'' ''Post'' and, informally, ''WaPo'' or ''WP'', is an American daily newspaper published in Washington, D.C., the national capital. It is the most widely circulated newspaper in the Washington m ...
'', U.S. Senators
Bill Frist
William Harrison Frist (born February 22, 1952) is an American physician, businessman, conservationist and policymaker who served as a United States Senator from Tennessee from 1995 to 2007. A member of the Republican Party, he also served as ...
and
Hillary Clinton
Hillary Diane Rodham Clinton ( Rodham; born October 26, 1947) is an American politician, lawyer and diplomat. She was the 67th United States secretary of state in the administration of Barack Obama from 2009 to 2013, a U.S. senator represent ...
supported this observation, stating "
atientsneed...information, including access to their own health records... At the same time, we must ensure the privacy of the systems, or they will undermine the trust they are designed to create". A 2005 report by the
California Health Care Foundation found that "67 percent of national respondents felt 'somewhat' or 'very concerned' about the privacy of their personal medical records".
The importance of privacy in electronic health records became prominent with the passage of the
American Recovery and Reinvestment Act
The American Recovery and Reinvestment Act of 2009 (ARRA) (), nicknamed the Recovery Act, was a stimulus package enacted by the 111th U.S. Congress and signed into law by President Barack Obama in February 2009. Developed in response to the G ...
(ARRA) in 2009. One of the provisions (known as the
Health Information Technology for Economic and Clinical Health
The Health Information Technology for Economic and Clinical Health Act, abbreviated the HITECH Act, was enacted under Title XIII of the American Recovery and Reinvestment Act of 2009 (). Under the HITECH Act, the United States Department of Health ...
ITECHAct) of the ARRA mandated incentives to clinicians for the implementation of electronic health records by 2015.Privacy advocates in the United States have raised concerns about unauthorized access to personal data as more medical practices switch from paper to electronic medical records. The
(ONC) explained that some of the safety measures that EHR systems can utilize are passwords and pin numbers that control access to such systems, encryption of information, and an audit trail to keep track of the changes made to records.
Providing patient access to EHRs is strictly mandated by HIPAA's Privacy Rule. One study found that each year there are an estimated 25 million compelled authorizations for the release of personal health records. . Researchers, however, have found new security threats open up as a result. Some of these security and privacy threats include hackers,
viruses
A virus is a submicroscopic infectious agent that replicates only inside the living cells of an organism. Viruses infect all life forms, from animals and plants to microorganisms, including bacteria and archaea. Viruses are found in almo ...
,
worms
The World Register of Marine Species (WoRMS) is a taxonomic database that aims to provide an authoritative and comprehensive catalogue and list of names of marine organisms.
Content
The content of the registry is edited and maintained by scien ...
, and the unintended consequences of the speed at which patients are expected to have their records disclosed while frequently containing sensitive terms that carry the risk of accidental disclosure.
These privacy threats are made more prominent by the emergence of "
cloud computing
Cloud computing is "a paradigm for enabling network access to a scalable and elastic pool of shareable physical or virtual resources with self-service provisioning and administration on-demand," according to International Organization for ...
", which is the use of shared computer processing power. Health care organizations are increasingly using cloud computing as a way to handle large amounts of data. This type of
data storage
Data storage is the recording (storing) of information (data) in a storage medium. Handwriting, phonographic recording, magnetic tape, and optical discs are all examples of storage media. Biological molecules such as RNA and DNA are con ...
, however, is susceptible to
natural disaster
A natural disaster is the very harmful impact on a society or community brought by natural phenomenon or Hazard#Natural hazard, hazard. Some examples of natural hazards include avalanches, droughts, earthquakes, floods, heat waves, landslides ...
s,
cybercrime
Cybercrime encompasses a wide range of criminal activities that are carried out using digital devices and/or Computer network, networks. It has been variously defined as "a crime committed on a computer network, especially the Internet"; Cyberc ...
and
technological terrorism, and hardware failure. Health information breaches accounted for the 39 percent of all breaches in 2015. IT Security costs and implementations are needed to protect health institutions against security and data breaches.
Health screening cases
Although privacy issues with the
health screening
In medicine, screening is a strategy used to look for as-yet-unrecognised conditions or risk markers. This testing can be applied to individuals or to a whole population without symptoms or signs of the disease being screened.
Screening interv ...
is a great concern among individuals and organizations, there has been little focus on the amount of work being done within the law to maintain the privacy expectation that people desire.
Many of these issues lie within the abstractness of the term "privacy" as there are many different interpretations of the term, especially in the context of the law.
Prior to 1994, there had been no cases regarding screening practices and the implications towards an individual's medical privacy, unless it was regarding HIV and drug testing.
Within ''Glover v Eastern Nebraska Community Office of Retardation'', an employee sued her employer against violating her
4th amendment rights because of unnecessary
HIV testing.
The court ruled in favor of the employer and argued that it was unreasonable search to have it tested. However, this was only one of the few precedents that people have to use. With more precedents, the relationships between employees and employers will be better defined. Yet with more requirements, testing among patients will lead to additional standards for meeting health care standards.
has become a large indicator for diagnostic tools, yet there are concerns with the information that can be gained and subsequently shared with other people other than the patient and healthcare provider
Third party issues
One of the main dangers to an individual's privacy are private corporations because of the
profits they can receive from selling seemingly private information.
Privacy merchants are made up of two groups - one that tries to collect people's personal information while the other focuses on using client's information to market company products.
Subsequently, privacy merchants purchase information from other companies, such as
health insurance
Health insurance or medical insurance (also known as medical aid in South Africa) is a type of insurance that covers the whole or a part of the risk of a person incurring medical expenses. As with other types of insurance, risk is shared among ma ...
companies, if there is not sufficient information from their own research.
Privacy merchants target health insurance companies because, nowadays, they collect huge amounts of personal information and keep them in large databases. They often require patients to provide more information that is needed for purposes other than that of doctors and other medical workers.
Additionally, people's information can be linked to other information outside of the medical field. For example, many employers use insurance information and medical records as an indicator of work ability and ethic.
The selling of privacy information can also lead employers to make much money; however, this happens to many people without their consent or knowledge.
Within the United States, in order to define clear
privacy laws
Privacy law is a set of regulations that govern the collection, storage, and utilization of personal information from healthcare, governments, companies, public or private entities, or individuals.
Privacy laws are examined in relation to an ind ...
regarding medical privacy, Title 17 thoroughly explains the ownership of one's data and adjusted the law so that people have more control over their own property.
The Privacy Act of 1974 offers more restrictions regarding what corporations can access outside of an individual's consent.
States have created additional supplements to medical privacy laws. With HIPAA, many individuals were pleased to see the federal government take action in protecting the medical information of individuals. Yet when people looked into it, there was proof that the government was still protecting the rights of corporations.
Many rules were seen as more of suggestions and the punishment for compromising the privacy of its patients were minimal.
Even if release of medical information requires consent, blank authorizations can be allowed and will not ask for individuals for additional consent later on.
Although there is a large group of people who oppose the selling of individual's medical information, there are groups such as the Health Benefits Coalition, the
Healthcare Leadership Council, and the
Health Insurance Association of America that are against the new reforms for data protection as it can ruin their work and profits.
Previous controversies, such as Google's "Project Nightingale" in 2019 have demonstrated potential holes in regulations of patient data and medical information. Project Nightingale, a joint effort between Google and the healthcare network Ascension, saw to the selling of millions of patients' identifiable medical information without their consent. Though Google claimed that their process was legal in obtaining the information, there was concern between researchers on this claim.
Efforts to protect health information
With the lack of help from the Department of Health and Human Services there is a conflict of interest that has been made clear. Some wish to place individual betterment as more important, while others focus more on external benefits from outside sources. The issues that occur when there are problems between the two groups are also not adequately solved which leads to controversial laws and effects.
Individual interests take precedence over the benefits of society as a whole and are often viewed as selfish and for the gain of capital value. If the government does not make any more future changes to the current legislation, countless organizations and people will have access to individual medical information.
In 1999, the
Gramm-Leach-Billey Act (GLBA) addressed the insurance privacy debate regarding medical privacy.
Yet, there were many issues with the implementation. One issue was that there were inconsistent regulation requirements within the different states due to preexisting laws.
Secondly, it was difficult to combine the pre-existing laws with the new framework.
And thirdly, in order for the federal government to implement these new rules, they needed state legislature to pass it.
GLBA aimed to regulate financial institutions so that corporations could not affect people's insurance. Because of the difficulty of the implementation of the GLBA, state legislatures are able to interpret the laws themselves and create initiatives to protect the medical privacy.
When states are creating their own independent legislature, they create standards that understand the impact of the legislation.
If they stray from the standard laws, they must be valid and fair. The new legislation must protect the rights of businesses and allow them to continue to function despite federally regulated competition. Patients gain benefits from these new services and standards through the flow of information that is considerate with medical privacy expectations.
These regulations should focus more on the consumer versus the benefits and political exploitation. Many times, regulations are for the personal gain of the corporation, therefore, state legislatures be wary of this and try to prevent it to the best of their abilities.
Medical privacy is not a new issue within the
insurance industry
Insurance is a means of protection from financial loss in which, in exchange for a fee, a party agrees to compensate another party in the event of a certain loss, damage, or injury. It is a form of risk management, primarily used to protect ...
, yet the problems regarding exploitation continue to reoccur; there is more focus on taking advantage of the business environment for personal gain.
In 2001, President George W. Bush passed additional regulations to
HIPAA
The Health Insurance Portability and Accountability Act of 1996 (HIPAA or the Kennedy– Kassebaum Act) is a United States Act of Congress enacted by the 104th United States Congress and signed into law by President Bill Clinton on August 21, ...
in order to better protect the privacy of individual medical information.
These new regulations were supposed to safeguard health information privacy by creating extensive solutions for the privacy of patients. The new regulation goals included being notified once an individual's information is inspected, amend any medical records, and request communication opportunities to discuss information disclosure.
However, there are exceptions to when the disclosure of PHI can be inspected. This includes specific conditions among law enforcement, judicial and administrative proceedings, parents, significant others, public health, health research, and
commercial marketing.
These aspects of lack of privacy have caused an alarming number of gaps within privacy measures.
Ultimately, there is still an issue on how to ensure privacy securities; in response, the government has created new regulations that makes trade offs between an individual's privacy and public benefit. These new regulations, however, still cover individually identifiable health information - any data that contains information unique to an individual.
However, non-identifiable data is not covered as the government claims it will cause minimal damage to a person's privacy. It also covers all health care organizations and covers businesses as well.
Additionally, under new HIPAA additions, the state legislation is more protective than national laws because it created more obligations for organizations to follow. Ultimately, the new rules called for expansive requirements that created better safety measures for individuals.
Yet, there are still ways that businesses and healthcare organizations can be exempt from disclosure rules for all individuals. Thus, the HHS needs to find more ways to balance personal and public trade offs within medical laws. This creates a need for extra government intervention to enforce legislation and new standards to decrease the number of threats against an individual's privacy of health data.
The
COVID-19 pandemic
The COVID-19 pandemic (also known as the coronavirus pandemic and COVID pandemic), caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), began with an disease outbreak, outbreak of COVID-19 in Wuhan, China, in December ...
led to a global effort to use technologies, like contact tracing, to reduce the spread of the disease.
Contact tracing
In public health, contact tracing is the process of identifying people who may have been exposed to an infected person ("contacts") and subsequent collection of further data to assess transmission. By tracing the contacts of infected individua ...
involves notifying people that they have been in contact with an individual who has tested positive for the virus. This led to the general public being concerned about the privacy risks of this technology. In response, in April 2020 Apple and Google created a contact tracing API.
Effects of changing medical privacy laws
Physician-patient relationships
Patients want to be able to share medical information with their physicians, yet they worry about potential privacy breaches that can occur when they release financial and confidential medical information.
In order to ensure better protection, the government has created frameworks for keeping information confidential - this includes being transparent about procedures, disclosure and protection of information, and monitoring of these new rules to ensure that people's information.
Effects of Technological Advances
Recently physicians and patients have started to use email as an additional communication tool for treatment and medical interactions. This way of communication is not "new", but its effects on doctor patient relationships has created new questions regarding legal, moral, and financial problems.
The
American Medical Informatics Association has characterized medical emails as way to communicate "medical advice, treatment, and information exchanged professionally"; yet, the "spontaneity, permanence, and information power characterizing" role is significant because of its unknown affects.
However, the use of emails allows for increased access, immediate aid, and increased interactions between patients and doctors.
There are many benefits and negative aspects of using emails; doctors feel a new sense of negative responsibility to respond to emails outside of the office, but also find benefits with facilitating rapid responses to patient's questions.
Additionally, the use of email between physicians and their patients will continue to grow because of the increasing use of the Internet. With the Internet, patients are able to ask for medical advice and treatment, yet issues regarding confidentiality and legal issues come up.
Ultimately, emails between a physician and patient are supposed to be used as a supplement for face to face interactions, not for casual messages. If used properly, physicians could use emails as a way to supplement interactions and provide more medical aid to those who need it immediately.
Traditional beliefs on doctor-patient relationship
Although many people believe that the technological changes are the reason for fear of sharing medical privacy, there is a theory that states that institutional ideals between doctors and their patients have created the fear of sharing medical privacy information.
Although levels of confidentiality are changing, individuals often feel the need to share more information with their doctors in order to get diagnosed correctly.
Because of this, people are concerned with how much information their physicians have. This information could be transferred to other third-party companies. However, there is a call for smaller emphasis on sharing and confidentiality in order to rid patients from their fears of information breaching.
There is a common belief that the confidentiality of one's information also only protects the doctors and not the patients, therefore there is a negative stigma towards revealing too much information.
Thus it causes patients to not share vital information relevant to their illnesses.
Standards and laws by country
Australia – eHealth
On July 1, 2012, the
Australian Government
The Australian Government, also known as the Commonwealth Government or simply as the federal government, is the national executive government of Australia, a federal parliamentary constitutional monarchy. The executive consists of the pr ...
launched the
Personally Controlled Electronic Health Record (PCEHR) (eHealth) system.
The full implementation incorporates an electronic summary prepared by nominated healthcare providers along with consumer-provided notes. Further, the summary includes information on the individual's allergies, adverse reactions, medications, immunizations, diagnoses, and treatments. The consumer notes operate as a personal medical diary that only the individual can view and edit.
The
opt-in
Opt-in email is a term used when someone is not initially added to an emailing list and is instead given the option to join the emailing list. Typically, this is some sort of mailing list, newsletter, or advertising. Opt-out emails do not ask ...
system gives people the option to choose whether to register for the eHealth record or not.
As of January 2016, the Commonwealth Department of Health changed the name PCEHR to My Health Record.
Privacy – governance
The Personally Controlled Electronic Health Records Act 2012 and
Privacy Act 1988
The ''Privacy Act 1988'' is an Australian law dealing with privacy.
Section 14 of the Act stipulates a number of privacy rights known as the Australian Privacy Principles (APPs). These principles apply to Australian Government and Australian C ...
governs how eHealth record information is managed and protected.
The PCEHR System Operator abides by the Information Privacy Principles in the Privacy Act 1988 (Commonwealth) as well as any applicable State or Territory privacy laws.
A Privacy Statement sets out the application of the collection of personal information by the System Operator. The statement includes an explanation of the types of personal information collected, what the information is used for, and how the information is stored. The statement covers measures in place to protect personal information from misuse, loss, unauthorized access, modification, and disclosure.
Privacy – security measures
Security measures include audit trails so that patients can see who has accessed their medical records along with the time the records were accessed. Other measures include the use of encryption as well as secure logins and passwords. Patient records are identified using an Individual Health Identifier (IHI), assigned by
Medicare, the IHI service provider.
[http://www.himaa.org.au/members/journal]
/ref>
Privacy – issues
A 2012 nationwide survey in Australia assessed privacy concerns on patients' health care decisions, which could impact patient care. Results listed that 49.1% of Australian patients stated they have withheld or would withhold information from their health care provider based on privacy concerns.
Canada
The privacy of patient information is protected at both the federal level and provincial level in Canada
Canada is a country in North America. Its Provinces and territories of Canada, ten provinces and three territories extend from the Atlantic Ocean to the Pacific Ocean and northward into the Arctic Ocean, making it the world's List of coun ...
. The health information legislation established the rules that must be followed for the collection, use, disclosure and protection of health information by healthcare workers known as "custodians". These custodians have been defined to include almost all healthcare professionals (including all physicians, nurses, chiropractors, operators of ambulances and operators of nursing homes). In addition to the regulatory bodies of specific healthcare workers, the provincial privacy commissions are central to the protection of patient information.
Turkey
The privacy of patient information is guaranteed by articles 78 and 100 of legal code 5510.
On the other hand, the Social Security Institution (SGK), which regulates and administers state-sponsored social security / insurance benefits, sells patient information after allegedly anonymizing the data, confirmed on October 25, 2014.
United Kingdom
The National Health Service
The National Health Service (NHS) is the term for the publicly funded health care, publicly funded healthcare systems of the United Kingdom: the National Health Service (England), NHS Scotland, NHS Wales, and Health and Social Care (Northern ...
is increasingly using electronic health record
An electronic health record (EHR) is the systematized collection of electronically stored patient and population health information in a digital format. These records can be shared across different health care settings. Records are shared thro ...
s, but until recently, the records held by individual NHS organisations, such as General Practitioners, NHS Trust
An NHS trust is an organisational unit within the National Health Services of England and Wales, generally serving either a geographical area or a specialised function (such as an ambulance service). In any particular location there may be several ...
s, dentists and pharmacies, were not linked. Each organization was responsible for the protection of patient data it collected. The care. data programme, which proposed to extract anonymised data from GP surgeries into a central database, aroused considerable opposition.
In 2003, the NHS made moves to create a centralized electronic registry of medical records. The system is protected by the UK's Government Gateway, which was built by Microsoft
Microsoft Corporation is an American multinational corporation and technology company, technology conglomerate headquartered in Redmond, Washington. Founded in 1975, the company became influential in the History of personal computers#The ear ...
. This program is known as the Electronic Records Development and the Implementation Programme (ERDIP). The NHS National Program for IT was criticized for its lack of security and lack of patient privacy. It was one of the projects that caused the Information Commissioner to warn about the danger of the country "sleepwalking" into a surveillance society. Pressure groups opposed to ID cards also campaigned against the centralized registry.
Newspapers feature stories about lost computers and memory sticks but a more common and longstanding problem is about staff accessing records that they have no right to see. It has always been possible for staff to look at paper records, and in most cases, there is no track of record. Therefore, electronic records make it possible to keep track of who has accessed which records. NHS Wales
NHS Wales () is the publicly-funded healthcare system in Wales, and one of the four systems which make up the National Health Service () in the United Kingdom.
NHS Wales was formed as part of the public health system for England and Wales crea ...
has created the National Intelligent Integrated Audit System which provides "a range of automatically generated reports, designed to meet the needs of our local health boards and trusts, instantly identifying any potential issues when access has not been legitimate". Maxwell Stanley Consulting will use a system called Patient Data Protect (powered by VigilancePro) which can spot patterns – such as whether someone is accessing data about their relatives or colleagues.
United States
Since 1974, numerous federal laws have been passed in the United States to specify the privacy rights and protections of patients, physicians, and other covered entities to medical data. Many states have passed its own laws to try and better protect the medical privacy of their citizens.
An important national law regarding medical privacy is the Health Insurance Portability and Accountability Act of 1996 (HIPAA), yet there are many controversies regarding the protection rights of the law.
Health Insurance Portability and Accountability Act of 1996 (HIPAA)
The most comprehensive law passed is the Health Insurance Portability and Accountability Act of 1996 (HIPAA), which was later revised after the Final Omnibus Rule in 2013. HIPAA provides a federal minimum standard for medical privacy, sets standards for uses and disclosures of protected health information (PHI), and provides civil and criminal penalties for violations.
Prior to HIPAA, only certain groups of people were protected under medical laws such as individuals with HIV or those who received Medicare aid.Congress
A congress is a formal meeting of the representatives of different countries, constituent states, organizations, trade unions, political parties, or other groups. The term originated in Late Middle English to denote an encounter (meeting of ...
passed the Genetic Information Nondiscrimination Act of 2008 (GINA), which aimed to prohibit genetic discrimination
Genetic discrimination occurs when people treat others (or are treated) differently because they have or are perceived to have a gene mutation(s) that causes or increases the risk of an inherited disorder. It may also refer to any and all discr ...
for individuals seeking health insurance and employment. The law also included a provision which mandated that genetic information held by employers be maintained in a separate file and prohibited disclosure of genetic information except in limited circumstances.
In 2013, after GINA was passed, the HIPAA Omnibus Rule amended HIPAA regulations to include genetic information in the definition of Protected Health Information (PHI). This rule also expanded HIPAA by broadening the definition of business associates to include any entity that sends or accesses PHI such as health IT vendors.
= Controversies
=
The Health Insurance Portability and Accountability Act (HIPAA) is critiqued for not providing strong medical privacy protections as it only provides regulations that disclose certain information.credit score
A credit score is a numerical expression based on a level analysis of a person's credit files, to represent the creditworthiness of an individual. A credit score is primarily based on a credit report, information typically sourced from credit bu ...
sharing or loss of insurance.
Hurricane Katrina
HIPAA does not protect the information of individuals as the government is able to publish certain information when they find it necessary. The government is exempted from privacy rules regarding national security. HIPAA additionally allows the authorization of protected health information (PHI) in order to aid in threats to public health and safety as long as it follows the good faith requirement - the idea that disclosing of information is necessary to the benefit of the public.Hurricane Katrina
Hurricane Katrina was a powerful, devastating and historic tropical cyclone that caused 1,392 fatalities and damages estimated at $125 billion in late August 2005, particularly in the city of New Orleans and its surrounding area. ...
, many people in Louisiana relied on Medicaid and their PHI was subsequently affected. People's medical privacy rights were soon waived in order for patient's to get the treatment they needed. Yet, many patients were unaware that their rights had been waived.
Medical data outside of HIPAA
Many patients mistakenly believe that HIPAA protects all health information. HIPAA does not usually cover fitness trackers, social media sites and other health data created by the patient. Health information can be disclosed by patients in emails, blogs, chat groups, or social media sites including those dedicated to specific illnesses, "liking" web pages about diseases, completing online health and symptom checkers, and donating to health causes. In addition, credit card payments for physician visit co-pays, purchase of over the counter
Over-the-counter (OTC) drugs are medicines sold directly to a consumer without a requirement for a prescription from a healthcare professional, as opposed to prescription drugs, which may be supplied only to consumers possessing a valid pres ...
(OTC) medications, home testing products, tobacco products, and visits to alternative practitioners are also not covered by HIPAA.
A 2015 study reported over 165,000 health apps available to consumers. Disease treatment and management account for nearly a quarter of consumer apps. Two-thirds of the apps target fitness and wellness, and ten percent of these apps can collect data from a device or sensor. Since the Food and Drug Administration
The United States Food and Drug Administration (FDA or US FDA) is a List of United States federal agencies, federal agency of the United States Department of Health and Human Services, Department of Health and Human Services. The FDA is respo ...
(FDA) only regulates medical devices and most of these applications are not medical devices, they do not require FDA approval. The data from most apps are outside HIPAA regulations because they do not share data with healthcare providers. "Patients may mistakenly assume that mobile apps are under the scope of HIPAA since the same data, such as heart rate, may be collected by an application that is accessible to their physician and covered by HIPAA, or on a mobile app that is not accessible to the physician and not covered by HIPAA.
Changes
In 2000, there was a new surge to add new regulations to HIPAA. It included the following goals: to protect individual medical information by providing secure access and control of their own information, improving healthcare quality by creating a more trust between consumers and their healthcare providers and third party organizations, and improve the efficiency of the medical system through new rules and regulations put forth by the local governments, individuals, and organizations.
Oregon-specific laws
The Oregon Genetic Privacy Act (GPA) states that "an individual's genetic information is the property of the individual".
Connecticut-specific laws
In order to solve HIPAA issues within Connecticut, state legislatures tried to create better provisions to protect the people living within the state.
California-specific laws
In California
California () is a U.S. state, state in the Western United States that lies on the West Coast of the United States, Pacific Coast. It borders Oregon to the north, Nevada and Arizona to the east, and shares Mexico–United States border, an ...
, the Confidentiality of Medical Information Act (CMIA), provides more stringent protections than the federal statutes. HIPAA expressly provides that more stringent state laws like CMIA, will override HIPAA's requirements and penalties. More specifically, CMIA prohibits providers, contractors and health care service plans from disclosing PHI without prior authorization.
These medical privacy laws also set a higher standard for health IT vendors or vendors of an individual's personal health record (PHR) by applying such statutes to vendors, even if they are not business associates of a covered entity. CMIA also outlines penalties for violating the law. These penalties range from liability to the patient (compensatory damages, punitive damages, attorneys' fees, costs of litigation) to civil and even criminal liability.
Likewise, California's Insurance Information and Privacy Protection Act (IIPPA) protects against unauthorized disclosure of PHI by prohibiting unapproved information sharing for information collected from insurance applications and claims resolution.
New Zealand
In New Zealand
New Zealand () is an island country in the southwestern Pacific Ocean. It consists of two main landmasses—the North Island () and the South Island ()—and List of islands of New Zealand, over 600 smaller islands. It is the List of isla ...
, th
Health Information Privacy Code (1994)
sets specific rules for agencies in the health sector to better ensure the protection of individual privacy. The code addresses the health information collected, used, held and disclosed by health agencies. For the health sector, the code takes the place of the information privacy principles.
Netherlands
The introduction of a nationwide system for the exchange of medical information and access to electronic patient records led to much discussion in the Netherlands
, Terminology of the Low Countries, informally Holland, is a country in Northwestern Europe, with Caribbean Netherlands, overseas territories in the Caribbean. It is the largest of the four constituent countries of the Kingdom of the Nether ...
.
Privacy for research participants
In the course of having or being part of a medical practice, doctors may obtain information that they wish to share with the medical or research community. If this information is shared or published, the privacy of the patients must be respected. Likewise, participants in medical research
Medical research (or biomedical research), also known as health research, refers to the process of using scientific methods with the aim to produce knowledge about human diseases, the prevention and treatment of illness, and the promotion of ...
that are outside the realm of direct patient care have a right to privacy as well.
Future research
While medical privacy remains an important right, it is also crucial to balance privacy with innovation. By limiting patient data in response to privacy violations, it potentially hinders data-driven innovation in medicine. In addition, keeping data secret for a competitive advantage also poses multiple concerns, potentially slowing advances in medical testing (e.g. Myriad Genetics).
See also
* STD notifications in dating services
* Electronic health record
An electronic health record (EHR) is the systematized collection of electronically stored patient and population health information in a digital format. These records can be shared across different health care settings. Records are shared thro ...
(EHR)
* Electronic medical record
An electronic health record (EHR) is the systematized collection of electronically stored patient and population health information in a digital format. These records can be shared across different health care settings. Records are shared thro ...
(EMR)
* Exemptions on the GDPR: national security
* Genetic privacy
Genetic privacy involves the concept of personal privacy concerning the storing, repurposing, provision to third parties, and displaying of information pertaining to one's genetic information. This concept also encompasses privacy regarding the abi ...
* Modesty in medical settings
* National Electronic Health Transition Authority (NEHTA)
* Personal health record
A personal health record (PHR) is a health record where health data and other information related to the care of a patient is maintained by the patient. This stands in contrast to the more widely used electronic medical record (EMR), which is oper ...
* Personally Controlled Electronic Health Record (PCEHR)
* Protected health information
Protected health information (PHI) under Law of the United States, U.S. law is any information about health status, provision of health care, or payment for health care that is created or collected by a Covered Entity (or a Business Associate of a ...
* Intentional contagion of infection
References
Further reading
*
External links
European Standards on Confidentiality and Privacy in Healthcare
Opt out of the NHS Spine
or the NHS Confidentiality campaign
Electronic Frontier Foundation on medical privacy
{{DEFAULTSORT:Medical Privacy
Medical privacy
Medical law
Data laws