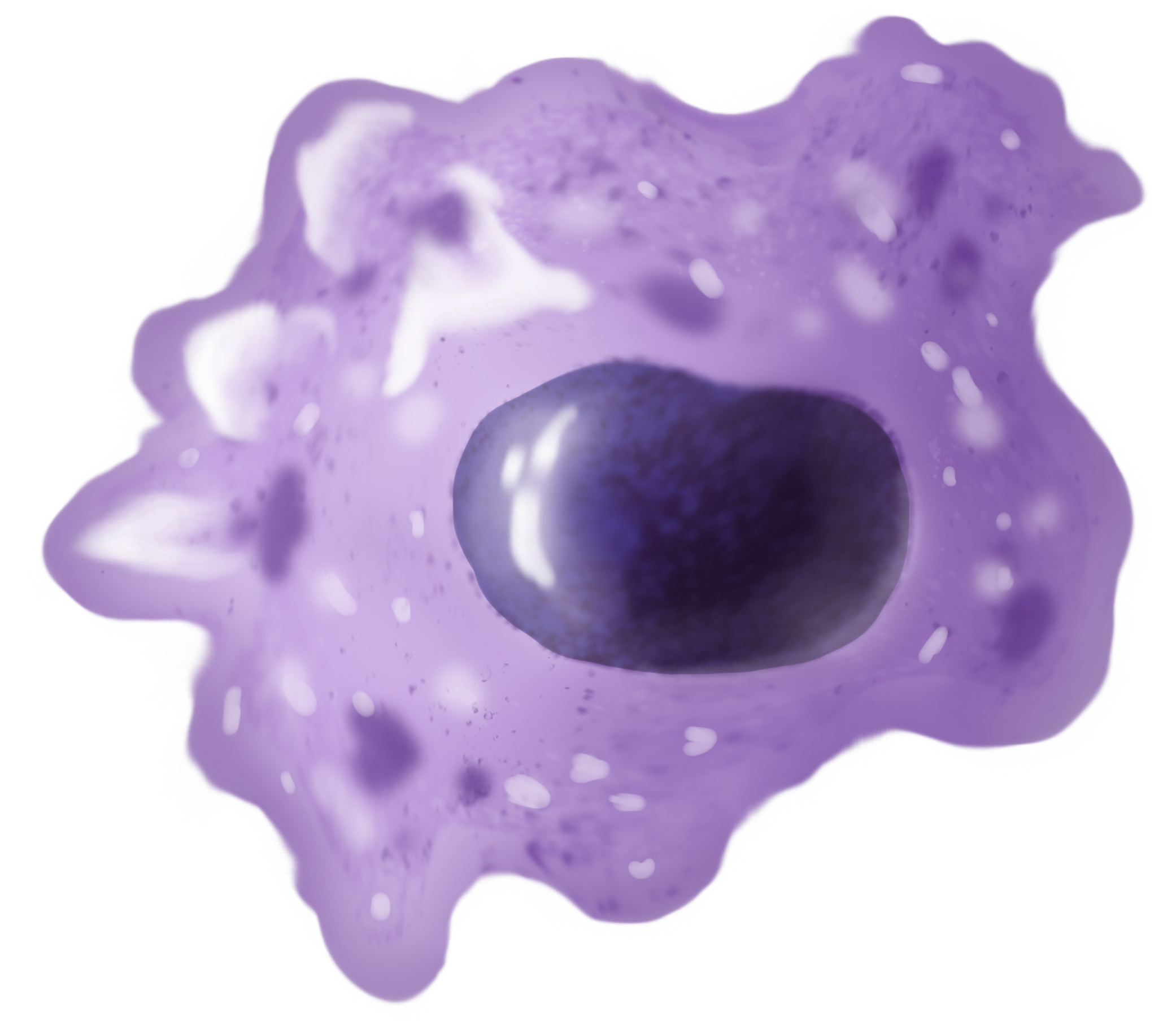
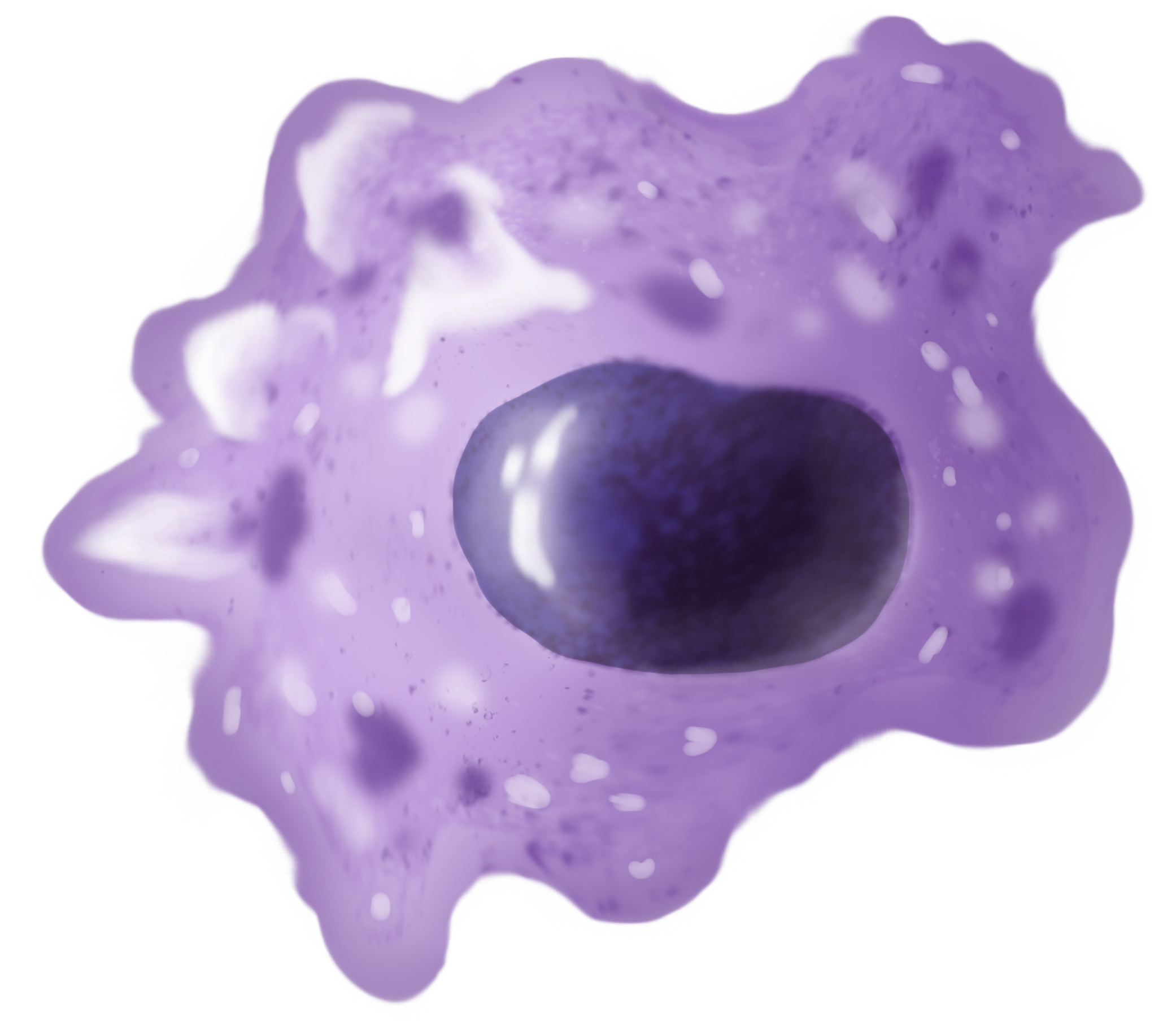
Macrophages (; abbreviated M
Žå, M╬” or MP) are a type of
white blood cell
White blood cells (scientific name leukocytes), also called immune cells or immunocytes, are cells of the immune system that are involved in protecting the body against both infectious disease and foreign entities. White blood cells are genera ...
of the
innate immune system
The innate immune system or nonspecific immune system is one of the two main immunity strategies in vertebrates (the other being the adaptive immune system). The innate immune system is an alternate defense strategy and is the dominant immune s ...
that engulf and digest pathogens, such as
cancer cells,
microbe
A microorganism, or microbe, is an organism of microscopic size, which may exist in its single-celled form or as a colony of cells. The possible existence of unseen microbial life was suspected from antiquity, with an early attestation in ...
s, cellular debris and foreign substances, which do not have proteins that are specific to healthy body cells on their surface.
This self-protection method can be contrasted with that employed by
Natural Killer cells. This process of engulfment and digestion is called
phagocytosis
Phagocytosis () is the process by which a cell (biology), cell uses its plasma membrane to engulf a large particle (Ōēź 0.5 ╬╝m), giving rise to an internal compartment called the phagosome. It is one type of endocytosis. A cell that performs ph ...
; it acts to defend the host against infection and injury.
Macrophages are found in essentially all tissues,
where they patrol for potential
pathogen
In biology, a pathogen (, "suffering", "passion" and , "producer of"), in the oldest and broadest sense, is any organism or agent that can produce disease. A pathogen may also be referred to as an infectious agent, or simply a Germ theory of d ...
s by
amoeboid movement. They take various forms (with various names) throughout the body (e.g.,
histiocytes,
Kupffer cells,
alveolar macrophage
An alveolar macrophage, pulmonary macrophage, (or dust cell, or dust eater) is a type of macrophage, a phagocytosis#Professional phagocytic cells, professional phagocyte, found in the airways and at the level of the pulmonary alveolus, alveoli in ...
s,
microglia
Microglia are a type of glia, glial cell located throughout the brain and spinal cord of the central nervous system (CNS). Microglia account for about around 5ŌĆō10% of cells found within the brain. As the resident macrophage cells, they act as t ...
, and others), but all are part of the
mononuclear phagocyte system
In immunology, the mononuclear phagocyte system or mononuclear phagocytic system (MPS), also known as the macrophage system, is a part of the immune system that consists of the Phagocyte, phagocytic cells located in reticular connective tissue. T ...
. Besides phagocytosis, they play a critical role in nonspecific defense (
innate immunity) and also help initiate specific defense mechanisms (
adaptive immunity) by recruiting other immune cells such as
lymphocyte
A lymphocyte is a type of white blood cell (leukocyte) in the immune system of most vertebrates. Lymphocytes include T cells (for cell-mediated and cytotoxic adaptive immunity), B cells (for humoral, antibody-driven adaptive immunity), an ...
s. For example, they are important as
antigen presenters to
T cell
T cells (also known as T lymphocytes) are an important part of the immune system and play a central role in the adaptive immune response. T cells can be distinguished from other lymphocytes by the presence of a T-cell receptor (TCR) on their cell ...
s. In humans, dysfunctional macrophages cause severe diseases such as
chronic granulomatous disease that result in frequent infections.
Beyond increasing
inflammation
Inflammation (from ) is part of the biological response of body tissues to harmful stimuli, such as pathogens, damaged cells, or irritants. The five cardinal signs are heat, pain, redness, swelling, and loss of function (Latin ''calor'', '' ...
and stimulating the immune system, macrophages also play an important
anti-inflammatory
Anti-inflammatory is the property of a substance or treatment that reduces inflammation, fever or swelling. Anti-inflammatory drugs, also called anti-inflammatories, make up about half of analgesics. These drugs reduce pain by inhibiting mechan ...
role and can decrease immune reactions through the release of
cytokines
Cytokines () are a broad and loose category of small proteins (~5ŌĆō25 kDa) important in cell signaling.
Cytokines are produced by a broad range of cells, including immune cells like macrophages, B cell, B lymphocytes, T cell, T lymphocytes ...
. Macrophages that encourage inflammation are called M1 macrophages, whereas those that decrease inflammation and encourage tissue repair are called M2 macrophages. This difference is reflected in their metabolism; M1 macrophages have the unique ability to metabolize
arginine
Arginine is the amino acid with the formula (H2N)(HN)CN(H)(CH2)3CH(NH2)CO2H. The molecule features a guanidinium, guanidino group appended to a standard amino acid framework. At physiological pH, the carboxylic acid is deprotonated (ŌłÆCO2ŌłÆ) a ...
to the "killer" molecule
nitric oxide
Nitric oxide (nitrogen oxide, nitrogen monooxide, or nitrogen monoxide) is a colorless gas with the formula . It is one of the principal oxides of nitrogen. Nitric oxide is a free radical: it has an unpaired electron, which is sometimes den ...
, whereas M2 macrophages have the unique ability to metabolize arginine to the "repair" molecule
ornithine
Ornithine is a non-proteinogenic ╬▒-amino acid that plays a role in the urea cycle. It is not incorporated into proteins during translation. Ornithine is abnormally accumulated in the body in ornithine transcarbamylase deficiency, a disorder of th ...
. However, this dichotomy has been recently questioned as further complexity has been discovered. Macrophages are widely thought of as highly plastic and fluid cells, with a fluctuating phenotype.
Human macrophages are about in diameter and are produced by the differentiation of
monocyte
Monocytes are a type of leukocyte or white blood cell. They are the largest type of leukocyte in blood and can differentiate into macrophages and monocyte-derived dendritic cells. As a part of the vertebrate innate immune system monocytes also ...
s in tissues. They can be identified using
flow cytometry or
immunohistochemical staining by their specific expression of proteins such as
CD14
CD14 ( cluster of differentiation 14) is a human protein made mostly by macrophages as part of the innate immune system. It helps to detect bacteria in the body by binding lipopolysaccharide (LPS), a pathogen-associated molecular pattern (PAMP). ...
,
CD40,
CD11b,
CD64,
F4/80 (mice)/
EMR1 (human),
lysozyme
Lysozyme (, muramidase, ''N''-acetylmuramide glycanhydrolase; systematic name peptidoglycan ''N''-acetylmuramoylhydrolase) is an antimicrobial enzyme produced by animals that forms part of the innate immune system. It is a glycoside hydrolase ...
M,
MAC-1/MAC-3 and
CD68.
Macrophages were first discovered and named by
├ēlie Metchnikoff
Ilya Ilyich Mechnikov (; ŌĆō 15 July 1916), also spelled ├ēlie Metchnikoff, was a zoologist from the Russian Empire of Moldavian noble ancestry and alshereat archive.org best known for his research in immunology (study of immune systems) and ...
, a Russian Empire zoologist, in 1884.
Structure
Types
A majority of macrophages are stationed at strategic points where microbial invasion or accumulation of foreign particles is likely to occur. These cells together as a group are known as the
mononuclear phagocyte system
In immunology, the mononuclear phagocyte system or mononuclear phagocytic system (MPS), also known as the macrophage system, is a part of the immune system that consists of the Phagocyte, phagocytic cells located in reticular connective tissue. T ...
and were previously known as the reticuloendothelial system. Each type of macrophage, determined by its location, has a specific name:
Investigations concerning Kupffer cells are hampered because in humans, Kupffer cells are only accessible for immunohistochemical analysis from biopsies or autopsies. From rats and mice, they are difficult to isolate, and after purification, only approximately 5 million cells can be obtained from one mouse.
Macrophages can express
paracrine
In cellular biology, paracrine signaling is a form of cell signaling, a type of cellular communication (biology), cellular communication in which a Cell (biology), cell produces a signal to induce changes in nearby cells, altering the behaviour of ...
functions within organs that are specific to the function of that organ. In the
testis
A testicle or testis ( testes) is the gonad in all male bilaterians, including humans, and is Homology (biology), homologous to the ovary in females. Its primary functions are the production of sperm and the secretion of Androgen, androgens, p ...
, for example, macrophages have been shown to be able to interact with
Leydig cells by secreting
25-hydroxycholesterol, an
oxysterol
An oxysterol is a derivative of cholesterol obtained by Redox, oxidation involving enzymes and / or pro-oxidants. Such compounds play important roles in various biological processes such as cholesterol homeostasis, lipid metabolism (sphingolipids, ...
that can be converted to
testosterone
Testosterone is the primary male sex hormone and androgen in Male, males. In humans, testosterone plays a key role in the development of Male reproductive system, male reproductive tissues such as testicles and prostate, as well as promoting se ...
by neighbouring Leydig cells.
Also, testicular macrophages may participate in creating an immune privileged environment in the testis, and in mediating infertility during inflammation of the testis.
Cardiac resident macrophages participate in electrical conduction via
gap junction
Gap junctions are membrane channels between adjacent cells that allow the direct exchange of cytoplasmic substances, such small molecules, substrates, and metabolites.
Gap junctions were first described as ''close appositions'' alongside tight ...
communication with cardiac
myocyte
A muscle cell, also known as a myocyte, is a mature contractile Cell (biology), cell in the muscle of an animal. In humans and other vertebrates there are three types: skeletal muscle, skeletal, smooth muscle, smooth, and Cardiac muscle, cardiac ...
s.
Macrophages can be classified on basis of the fundamental function and activation. According to this grouping, there are
classically activated (M1) macrophages, wound-healing macrophages (also known as
alternatively-activated (M2) macrophages), and
regulatory macrophages (Mregs).
Development
Macrophages that reside in adult healthy tissues either derive from circulating
monocytes
Monocytes are a type of leukocyte or white blood cell. They are the largest type of leukocyte in blood and can differentiate into macrophages and monocyte-derived dendritic cells. As a part of the vertebrate innate immune system monocytes also i ...
or are established before birth and then maintained during adult life independently of monocytes. By contrast, most of the macrophages that accumulate at diseased sites typically derive from circulating monocytes.
Leukocyte extravasation describes
monocyte
Monocytes are a type of leukocyte or white blood cell. They are the largest type of leukocyte in blood and can differentiate into macrophages and monocyte-derived dendritic cells. As a part of the vertebrate innate immune system monocytes also ...
entry into damaged tissue through the
endothelium
The endothelium (: endothelia) is a single layer of squamous endothelial cells that line the interior surface of blood vessels and lymphatic vessels. The endothelium forms an interface between circulating blood or lymph in the lumen and the r ...
of
blood vessels
Blood vessels are the tubular structures of a circulatory system that transport blood throughout many animalsŌĆÖ bodies. Blood vessels transport blood cells, nutrients, and oxygen to most of the tissues of a body. They also take waste an ...
as they become macrophages. Monocytes are attracted to a damaged site by chemical substances through
chemotaxis
Chemotaxis (from ''chemical substance, chemo-'' + ''taxis'') is the movement of an organism or entity in response to a chemical stimulus. Somatic cells, bacteria, and other single-cell organism, single-cell or multicellular organisms direct thei ...
, triggered by a range of stimuli including damaged cells, pathogens and
cytokines
Cytokines () are a broad and loose category of small proteins (~5ŌĆō25 kDa) important in cell signaling.
Cytokines are produced by a broad range of cells, including immune cells like macrophages, B cell, B lymphocytes, T cell, T lymphocytes ...
released by macrophages already at the site. At some sites such as the testis, macrophages have been shown to populate the organ through proliferation. Unlike short-lived
neutrophils, macrophages survive longer in the body, up to several months.
Function

Phagocytosis
Macrophages are
professional phagocytes and are highly specialized in removal of dying or dead cells and cellular debris. This role is important in chronic inflammation, as the early stages of inflammation are dominated by neutrophils, which expend themselves and are ingested by macrophages.
Macrophages normally present themselves at the wound site within 2 days following the injury.
The neutrophils are at first attracted to a site, where they perform their function and die, before they or their
neutrophil extracellular traps are phagocytized by the macrophages.
[ The first wave of neutrophils acts for approximately 2 days at the site and signals to attract macrophages. These macrophages will then ingest the aged neutrophils.]lysosome
A lysosome () is a membrane-bound organelle that is found in all mammalian cells, with the exception of red blood cells (erythrocytes). There are normally hundreds of lysosomes in the cytosol, where they function as the cellŌĆÖs degradation cent ...
. Within the phagolysosome, enzymes
An enzyme () is a protein that acts as a biological catalyst by accelerating chemical reactions. The molecules upon which enzymes may act are called substrates, and the enzyme converts the substrates into different molecules known as pro ...
and toxic peroxides digest the pathogen. However, some bacteria (such as ''Mycobacterium tuberculosis
''Mycobacterium tuberculosis'' (M. tb), also known as Koch's bacillus, is a species of pathogenic bacteria in the family Mycobacteriaceae and the causative agent of tuberculosis.
First discovered in 1882 by Robert Koch, ''M. tuberculosis'' ha ...
)'' have become resistant to these methods of digestion. Typhoidal ''Salmonellae'' induce their own phagocytosis by host macrophages in vivo and inhibit digestion by lysosomal action, thereby using macrophages for their own replication and causing macrophage apoptosis. Macrophages are capable of engulfing and digesting many bacteria during their life. They can die eventually due to factors including pathogenic cytotoxicity, oxidative stress, and phagocytosis-induced apoptosis. Phagocytosis-induced apoptosis results from the powerful apoptotic stimulus of consuming bacteria and is observed in (at least) macrophages and neutrophils.
Role in innate immune response
When a pathogen invades, tissue resident macrophages are among the first cells to respond.
Phagocytosis of pathogens
 Macrophages can internalize antigens through receptor-mediated phagocytosis.
Macrophages can internalize antigens through receptor-mediated phagocytosis.toll-like receptor
Toll-like receptors (TLRs) are a class of proteins that play a key role in the innate immune system. They are single-pass membrane protein, single-spanning receptor (biochemistry), receptors usually expressed on sentinel cells such as macrophages ...
s (TLRs), scavenger receptors (SRs), C-type lectin receptors, among others, recognize pathogens for phagocytosis.
Chemical secretion
Recognition of MAMPs by PRRs can activate tissue resident macrophages to secrete proinflammatory cytokines that recruit other immune cells. Among the PRRs, TLRs play a major role in signal transduction leading to cytokine production.NF-╬║B
Nuclear factor kappa-light-chain-enhancer of activated B cells (NF-╬║B) is a family of transcription factor protein complexes that controls transcription (genetics), transcription of DNA, cytokine production and cell survival. NF-╬║B is found i ...
and results in transcription of the genes for several proinflammatory cytokines, including IL-1╬▓, IL-6, TNF-╬▒, IL-12B, and type I interferons such as IFN-╬▒ and IFN-╬▓. Systemically, IL-1╬▓, IL-6, and TNF-╬▒ induce fever and initiate the acute phase response in which the liver secretes acute phase proteins.Neutrophil
Neutrophils are a type of phagocytic white blood cell and part of innate immunity. More specifically, they form the most abundant type of granulocytes and make up 40% to 70% of all white blood cells in humans. Their functions vary in differe ...
s are among the first immune cells recruited by macrophages to exit the blood via extravasation and arrive at the infection site.
Role in adaptive immunity

Interactions with CD4+ T Helper Cells
Macrophages are professional antigen presenting cells (APC), meaning they can present peptides from phagocytosed antigens on major histocompatibility complex (MHC) II molecules on their cell surface for T helper cells.CD80
The Cluster of differentiation 80 (also CD80 and B7-1) is a B7, type I membrane protein in the immunoglobulin superfamily, with an extracellular immunoglobulin constant-like domain and a variable-like domain required for receptor binding. It is c ...
and CD86 (also known as B7) that binds to CD28
CD28 (Cluster of Differentiation 28) is a protein expressed on T cells that provides essential co-stimulation, co-stimulatory signals required for T cell activation and survival. When T cells are stimulated through CD28 in conjunction with the T- ...
on T helper cells to supply the co-stimulatory signal.IL-2
The Ilyushin Il-2 (Russian language, Russian: ąśą╗čīčÄ╠üčłąĖąĮ ąśą╗-2) is a Ground attack aircraft, ground-attack plane that was produced by the Soviet Union in large numbers during the World War II, Second World War. The word ''shturmov├Łk'' (C ...
signaling in T cells upregulates the expression of anti-apoptotic protein Bcl-2, but T cell production of IL-2 and the high-affinity IL-2 receptor IL-2RA both require continued signal from TCR recognition of MHC-bound antigen.
Activation
Macrophages can achieve different activation phenotypes through interactions with different subsets of T helper cells, such as TH1 and TH2.
= Classical
=
TH1 cells play an important role in classical macrophage activation as part of type 1 immune response against intracellular pathogens (such as intracellular bacteria) that can survive and replicate inside host cells, especially those pathogens that replicate even after being phagocytosed by macrophages. After the TCR of TH1 cells recognize specific antigen peptide-bound MHC class II molecules on macrophages, TH1 cells 1) secrete IFN-╬│ and 2) upregulate the expression of CD40 ligand (CD40L), which binds to CD40 on macrophages.nitric oxide
Nitric oxide (nitrogen oxide, nitrogen monooxide, or nitrogen monoxide) is a colorless gas with the formula . It is one of the principal oxides of nitrogen. Nitric oxide is a free radical: it has an unpaired electron, which is sometimes den ...
(NO) and superoxide
In chemistry, a superoxide is a compound that contains the superoxide ion, which has the chemical formula . The systematic name of the anion is dioxide(1−). The reactive oxygen ion superoxide is particularly important as the product of t ...
(O2-).Mycobacterium tuberculosis
''Mycobacterium tuberculosis'' (M. tb), also known as Koch's bacillus, is a species of pathogenic bacteria in the family Mycobacteriaceae and the causative agent of tuberculosis.
First discovered in 1882 by Robert Koch, ''M. tuberculosis'' ha ...
'', the pathogen is contained through the formation of granuloma
A granuloma is an aggregation of macrophages (along with other cells) that forms in response to chronic inflammation. This occurs when the immune system attempts to isolate foreign substances that it is otherwise unable to eliminate. Such sub ...
, an aggregation of infected macrophages surrounded by activated T cells.
= Alternative
=
TH2 cells play an important role in alternative macrophage activation as part of type 2 immune response against large extracellular pathogens like helminths.arginine
Arginine is the amino acid with the formula (H2N)(HN)CN(H)(CH2)3CH(NH2)CO2H. The molecule features a guanidinium, guanidino group appended to a standard amino acid framework. At physiological pH, the carboxylic acid is deprotonated (ŌłÆCO2ŌłÆ) a ...
to ornithine
Ornithine is a non-proteinogenic ╬▒-amino acid that plays a role in the urea cycle. It is not incorporated into proteins during translation. Ornithine is abnormally accumulated in the body in ornithine transcarbamylase deficiency, a disorder of th ...
and urea
Urea, also called carbamide (because it is a diamide of carbonic acid), is an organic compound with chemical formula . This amide has two Amine, amino groups (ŌĆō) joined by a carbonyl functional group (ŌĆōC(=O)ŌĆō). It is thus the simplest am ...
.collagen
Collagen () is the main structural protein in the extracellular matrix of the connective tissues of many animals. It is the most abundant protein in mammals, making up 25% to 35% of protein content. Amino acids are bound together to form a trip ...
.
Interactions with CD8+ cytotoxic t cells
Another part of the adaptive immunity activation involves stimulating CD8+ via cross presentation of antigens peptides on MHC class I molecules. Studies have shown that proinflammatory macrophages are capable of cross presentation of antigens on MHC class I molecules, but whether macrophage cross-presentation plays a role in naïve or memory CD8+ T cell activation is still unclear.
Interactions with B cells
Macrophages have been shown to secrete cytokines BAFF and APRIL, which are important for plasma cell isotype switching. APRIL and IL-6 secreted by macrophage precursors in the bone marrow help maintain survival of plasma cells homed to the bone marrow.
Subtypes
There are several activated forms of macrophages.[ There is a phenotype shift from M1 to M2 macrophages in acute wounds, however this shift is impaired for chronic wounds. This dysregulation results in insufficient M2 macrophages and its corresponding growth factors that aid in wound repair. With a lack of these growth factors/anti-inflammatory cytokines and an overabundance of pro-inflammatory cytokines from M1 macrophages chronic wounds are unable to heal in a timely manner. Normally, after neutrophils eat debris/pathogens they perform apoptosis and are removed. At this point, inflammation is not needed and M1 undergoes a switch to M2 (anti-inflammatory). However, dysregulation occurs as the M1 macrophages are unable/do not phagocytose neutrophils that have undergone apoptosis leading to increased macrophage migration and inflammation.][
Both M1 and M2 macrophages play a role in promotion of ]atherosclerosis
Atherosclerosis is a pattern of the disease arteriosclerosis, characterized by development of abnormalities called lesions in walls of arteries. This is a chronic inflammatory disease involving many different cell types and is driven by eleva ...
. M1 macrophages promote atherosclerosis by inflammation. M2 macrophages can remove cholesterol from blood vessels, but when the cholesterol is oxidized, the M2 macrophages become apoptotic foam cells contributing to the atheromatous plaque of atherosclerosis.
Role in muscle regeneration
The first step to understanding the importance of macrophages in muscle repair, growth, and regeneration is that there are two "waves" of macrophages with the onset of damageable muscle useŌĆō subpopulations that do and do not directly have an influence on repairing muscle. The initial wave is a phagocytic population that comes along during periods of increased muscle use that are sufficient to cause muscle membrane lysis and membrane inflammation, which can enter and degrade the contents of injured muscle fibers.
Role in wound healing
Macrophages are essential for wound healing
Wound healing refers to a living organism's replacement of destroyed or damaged tissue by newly produced tissue.
In undamaged skin, the epidermis (surface, epithelial layer) and dermis (deeper, connective layer) form a protective barrier again ...
.[de la Torre J., Sholar A. (2006)]
Wound healing: Chronic wounds
Emedicine.com. Accessed 20 January 2008. They replace polymorphonuclear neutrophils as the predominant cells in the wound by day two after injury.monocyte
Monocytes are a type of leukocyte or white blood cell. They are the largest type of leukocyte in blood and can differentiate into macrophages and monocyte-derived dendritic cells. As a part of the vertebrate innate immune system monocytes also ...
s from the bloodstream enter the area through blood vessel walls.spleen
The spleen (, from Ancient Greek '' ŽāŽĆ╬╗╬«╬Į'', splßĖŚn) is an organ (biology), organ found in almost all vertebrates. Similar in structure to a large lymph node, it acts primarily as a blood filter.
The spleen plays important roles in reg ...
contains half the body's monocytes in reserve ready to be deployed to injured tissue.[Rosenberg L., de la Torre J. (2006)]
Wound Healing, Growth Factors
Emedicine.com. Accessed 20 January 2008. Macrophages may also restrain the contraction phase.oxygen
Oxygen is a chemical element; it has chemical symbol, symbol O and atomic number 8. It is a member of the chalcogen group (periodic table), group in the periodic table, a highly reactivity (chemistry), reactive nonmetal (chemistry), non ...
content of their surroundings to produce factors that induce and speed angiogenesis
Role in limb regeneration
Scientists have elucidated that as well as eating up material debris, macrophages are involved in the typical limb regeneration in the salamander.salamander
Salamanders are a group of amphibians typically characterized by their lizard-like appearance, with slender bodies, blunt snouts, short limbs projecting at right angles to the body, and the presence of a tail in both larvae and adults. All t ...
resulted in failure of limb regeneration and a scarring response.[
]
Role in iron homeostasis
As described above, macrophages play a key role in removing dying or dead cells and cellular debris. Erythrocytes
Red blood cells (RBCs), referred to as erythrocytes (, with -''cyte'' translated as 'cell' in modern usage) in academia and medical publishing, also known as red cells, erythroid cells, and rarely haematids, are the most common type of blood cel ...
have a lifespan on average of 120 days and so are constantly being destroyed by macrophages in the spleen and liver. Macrophages will also engulf macromolecule
A macromolecule is a "molecule of high relative molecular mass, the structure of which essentially comprises the multiple repetition of units derived, actually or conceptually, from molecules of low relative molecular mass." Polymers are physi ...
s, and so play a key role in the pharmacokinetics
Pharmacokinetics (from Ancient Greek ''pharmakon'' "drug" and ''kinetikos'' "moving, putting in motion"; see chemical kinetics), sometimes abbreviated as PK, is a branch of pharmacology dedicated to describing how the body affects a specific su ...
of parenteral irons.
The iron that is released from the haemoglobin is either stored internally in ferritin
Ferritin is a universal intracellular and extracellular protein that stores iron and releases it in a controlled fashion. The protein is produced by almost all living organisms, including archaea, bacteria, algae, higher plants, and animals. ...
or is released into the circulation via ferroportin. In cases where systemic iron levels are raised, or where inflammation is present, raised levels of hepcidin act on macrophage ferroportin channels, leading to iron remaining within the macrophages.
Role in pigment retainment
 Melanophages are a subset of tissue-resident macrophages able to absorb pigment, either native to the organism or exogenous (such as tattoos), from extracellular space. In contrast to dendritic juncional
Melanophages are a subset of tissue-resident macrophages able to absorb pigment, either native to the organism or exogenous (such as tattoos), from extracellular space. In contrast to dendritic juncional melanocyte
Melanocytes are melanin-producing neural-crest, neural crest-derived cell (biology), cells located in the bottom layer (the stratum basale) of the skin's epidermis (skin), epidermis, the middle layer of the eye (the uvea),
the inner ear,
vagina ...
s, which synthesize melanosomes and contain various stages of their development, the melanophages only accumulate phagocytosed melanin in lysosome-like phagosomes. This occurs repeatedly as the pigment from dead dermal macrophages is phagocytosed by their successors, preserving the tattoo in the same place.
Role in tissue homeostasis
Every tissue harbors its own specialized population of resident macrophages, which entertain reciprocal interconnections with the stroma and functional tissue. These resident macrophages are sessile (non-migratory), provide essential growth factors to support the physiological function of the tissue (e.g. macrophage-neuronal crosstalk in the guts), and can actively protect the tissue from inflammatory damage.
Nerve-associated macrophages
Nerve-associated macrophages or NAMs are those tissue-resident macrophages that are associated with nerves. Some of them are known to have an elongated morphology of up to 200╬╝m
Clinical significance
Due to their role in phagocytosis, macrophages are involved in many diseases of the immune system. For example, they participate in the formation of granuloma
A granuloma is an aggregation of macrophages (along with other cells) that forms in response to chronic inflammation. This occurs when the immune system attempts to isolate foreign substances that it is otherwise unable to eliminate. Such sub ...
s, inflammatory lesions that may be caused by a large number of diseases. Some disorders, mostly rare, of ineffective phagocytosis and macrophage function have been described, for example.
As a host for intracellular pathogens
In their role as a phagocytic immune cell macrophages are responsible for engulfing pathogens to destroy them. Some pathogens subvert this process and instead live inside the macrophage. This provides an environment in which the pathogen is hidden from the immune system and allows it to replicate.
Diseases with this type of behaviour include tuberculosis
Tuberculosis (TB), also known colloquially as the "white death", or historically as consumption, is a contagious disease usually caused by ''Mycobacterium tuberculosis'' (MTB) bacteria. Tuberculosis generally affects the lungs, but it can al ...
(caused by ''Mycobacterium tuberculosis
''Mycobacterium tuberculosis'' (M. tb), also known as Koch's bacillus, is a species of pathogenic bacteria in the family Mycobacteriaceae and the causative agent of tuberculosis.
First discovered in 1882 by Robert Koch, ''M. tuberculosis'' ha ...
'') and leishmaniasis
Leishmaniasis is a wide array of clinical manifestations caused by protozoal parasites of the Trypanosomatida genus ''Leishmania''. It is generally spread through the bite of Phlebotominae, phlebotomine Sandfly, sandflies, ''Phlebotomus'' an ...
(caused by ''Leishmania
''Leishmania'' () is a genus of parasitic protozoans, single-celled eukaryotic organisms of the trypanosomatid group that are responsible for the disease leishmaniasis. The parasites are transmitted by sandflies of the genus '' Phlebotomus'' ...
'' species).
In order to minimize the possibility of becoming the host of an intracellular bacteria, macrophages have evolved defense mechanisms such as induction of nitric oxide and reactive oxygen intermediates, which are toxic to microbes. Macrophages have also evolved the ability to restrict the microbe's nutrient supply and induce autophagy
Autophagy (or autophagocytosis; from the Greek language, Greek , , meaning "self-devouring" and , , meaning "hollow") is the natural, conserved degradation of the cell that removes unnecessary or dysfunctional components through a lysosome-depe ...
.
Tuberculosis
Once engulfed by a macrophage, the causative agent of tuberculosis, ''Mycobacterium tuberculosis'',
Leishmaniasis
Upon phagocytosis by a macrophage, the ''Leishmania'' parasite finds itself in a phagocytic vacuole. Under normal circumstances, this phagocytic vacuole would develop into a lysosome and its contents would be digested. ''Leishmania'' alter this process and avoid being destroyed; instead, they make a home inside the vacuole.
Chikungunya
Infection of macrophages in joints is associated with local inflammation during and after the acute phase of '' Chikungunya'' (caused by CHIKV or Chikungunya virus).
Others
Adenovirus
Adenoviruses (members of the family ''Adenoviridae'') are medium-sized (90ŌĆō100 nm), nonenveloped (without an outer lipid bilayer) viruses with an icosahedral nucleocapsid containing a double-stranded DNA genome. Their name derives from t ...
(most common cause of pink eye) can remain latent in a host macrophage, with continued viral shedding 6ŌĆō18 months after initial infection.
''Brucella spp.'' can remain latent in a macrophage via inhibition of phagosomeŌĆōlysosome
A lysosome () is a membrane-bound organelle that is found in all mammalian cells, with the exception of red blood cells (erythrocytes). There are normally hundreds of lysosomes in the cytosol, where they function as the cellŌĆÖs degradation cent ...
fusion; causes brucellosis
Brucellosis is a zoonosis spread primarily via ingestion of raw milk, unpasteurized milk from infected animals. It is also known as undulant fever, Malta fever, and Mediterranean fever.
The bacteria causing this disease, ''Brucella'', are small ...
(undulant fever).
''Legionella pneumophila
''Legionella pneumophila'', the primary causative agent for Legionnaires' disease, Legionnaire's disease, is an Aerobic organism, aerobic, pleomorphic, Flagellum, flagellated, non-spore-forming, Gram-negative bacteria, Gram-negative bacterium. ' ...
'', the causative agent of Legionnaires' disease
Legionnaires' disease is a form of atypical pneumonia caused by any species of ''Legionella'' bacteria, quite often ''Legionella pneumophila''. Signs and symptoms include cough, shortness of breath, high fever, myalgia, muscle pains, and headach ...
, also establishes residence within macrophages.
Heart disease
Macrophages are the predominant cells involved in creating the progressive plaque lesions of atherosclerosis
Atherosclerosis is a pattern of the disease arteriosclerosis, characterized by development of abnormalities called lesions in walls of arteries. This is a chronic inflammatory disease involving many different cell types and is driven by eleva ...
.
Focal recruitment of macrophages occurs after the onset of acute myocardial infarction
A myocardial infarction (MI), commonly known as a heart attack, occurs when Ischemia, blood flow decreases or stops in one of the coronary arteries of the heart, causing infarction (tissue death) to the heart muscle. The most common symptom ...
. These macrophages function to remove debris, apoptotic cells and to prepare for tissue regeneration. Macrophages protect against ischemia-induced ventricular tachycardia in hypokalemic mice.
HIV infection
Macrophages also play a role in human immunodeficiency virus
The human immunodeficiency viruses (HIV) are two species of ''Lentivirus'' (a subgroup of retrovirus) that infect humans. Over time, they cause AIDS, acquired immunodeficiency syndrome (AIDS), a condition in which progressive failure of th ...
(HIV) infection. Like T cells, macrophages can be infected with HIV, and even become a reservoir of ongoing virus replication throughout the body. HIV can enter the macrophage through binding of gp120 to CD4 and second membrane receptor, CCR5 (a chemokine receptor). Both circulating monocytes and macrophages serve as a reservoir for the virus. Macrophages are better able to resist infection by HIV-1 than CD4+ T cells, although susceptibility to HIV infection differs among macrophage subtypes.
Cancer
Macrophages can contribute to tumor growth and progression by promoting tumor cell proliferation and invasion, fostering tumor angiogenesis and suppressing antitumor immune cells.tumor necrosis factor
Tumor necrosis factor (TNF), formerly known as TNF-╬▒, is a chemical messenger produced by the immune system that induces inflammation. TNF is produced primarily by activated macrophages, and induces inflammation by binding to its receptors o ...
(TNF)-alpha released by the macrophages activate the gene switch nuclear factor-kappa B
Nuclear may refer to:
Physics
Relating to the nucleus of the atom:
* Nuclear engineering
* Nuclear physics
* Nuclear power
*Nuclear reactor
*Nuclear weapon
* Nuclear medicine
*Radiation therapy
*Nuclear warfare
Mathematics
* Nuclear space
* Nu ...
. NF-╬║B then enters the nucleus of a tumor cell and turns on production of proteins that stop apoptosis
Apoptosis (from ) is a form of programmed cell death that occurs in multicellular organisms and in some eukaryotic, single-celled microorganisms such as yeast. Biochemistry, Biochemical events lead to characteristic cell changes (Morphology (biol ...
and promote cell proliferation and inflammation. Moreover, macrophages serve as a source for many pro-angiogenic factors including vascular endothelial factor (VEGF), tumor necrosis factor-alpha
Tumor necrosis factor (TNF), formerly known as TNF-╬▒, is a chemical messenger produced by the immune system that induces inflammation. TNF is produced primarily by activated macrophages, and induces inflammation by binding to its receptors o ...
(TNF-alpha), macrophage colony-stimulating factor
The colony stimulating factor 1 (CSF1), also known as macrophage colony-stimulating factor (M-CSF), is a secreted cytokine which causes hematopoietic stem cells to differentiate into macrophages or other related cell types. Eukaryotic cells also ...
(M-CSF/CSF1) and IL-1 and IL-6, contributing further to the tumor growth.
Macrophages have been shown to infiltrate a number of tumors. Their number correlates with poor prognosis in certain cancers, including cancers of breast, cervix, bladder, brain and prostate. Some tumors can also produce factors, including M-CSF/CSF1, MCP-1/CCL2 and Angiotensin II
Angiotensin is a peptide hormone that causes vasoconstriction and an increase in blood pressure. It is part of the reninŌĆōangiotensin system, which regulates blood pressure. Angiotensin also stimulates the release of aldosterone from the ...
, that trigger the amplification and mobilization of macrophages in tumors. Additionally, subcapsular sinus macrophages in tumor-draining lymph nodes can suppress cancer progression by containing the spread of tumor-derived materials.
Cancer therapy
Experimental studies indicate that macrophages can affect all therapeutic modalities, including surgery
Surgery is a medical specialty that uses manual and instrumental techniques to diagnose or treat pathological conditions (e.g., trauma, disease, injury, malignancy), to alter bodily functions (e.g., malabsorption created by bariatric surgery s ...
, chemotherapy
Chemotherapy (often abbreviated chemo, sometimes CTX and CTx) is the type of cancer treatment that uses one or more anti-cancer drugs (list of chemotherapeutic agents, chemotherapeutic agents or alkylating agents) in a standard chemotherapy re ...
, radiotherapy
Radiation therapy or radiotherapy (RT, RTx, or XRT) is a treatment using ionizing radiation, generally provided as part of cancer therapy to either kill or control the growth of malignant cells. It is normally delivered by a linear particle ...
, immunotherapy and targeted therapy
Targeted therapy or molecularly targeted therapy is one of the major modalities of medical treatment (pharmacotherapy) for cancer, others being hormonal therapy (oncology), hormonal therapy and cytotoxic chemotherapy. As a form of molecular medici ...
.phagocytosis
Phagocytosis () is the process by which a cell (biology), cell uses its plasma membrane to engulf a large particle (Ōēź 0.5 ╬╝m), giving rise to an internal compartment called the phagosome. It is one type of endocytosis. A cell that performs ph ...
) following treatments that kill these cells; they can serve as drug depots for some anticancer drugs; they can also be activated by some therapies to promote antitumor immunity. Macrophages can also be deleterious in several ways: for example they can suppress various chemotherapies, radiotherapies and immunotherapies. Because macrophages can regulate tumor progression, therapeutic strategies to reduce the number of these cells, or to manipulate their phenotypes, are currently being tested in cancer patients. However, macrophages are also involved in antibody mediated cytotoxicity (ADCC) and this mechanism has been proposed to be important for certain cancer immunotherapy antibodies. Similarly, studies identified macrophages genetically engineered to express chimeric antigen receptors as promising therapeutic approach to lowering tumor burden.
Obesity
It has been observed that increased number of pro-inflammatory macrophages within obese adipose tissue contributes to obesity complications including insulin resistance and diabetes type 2.
The modulation of the inflammatory state of adipose tissue macrophages has therefore┬Ābeen considered a possible therapeutic target to treat obesity-related diseases. Although adipose tissue macrophages are subject to anti-inflammatory homeostatic control by sympathetic innervation, experiments using ADRB2 gene knockout mice indicate that this effect is indirectly exerted through the modulation of adipocyte function, and not through direct Beta-2 adrenergic receptor activation, suggesting that adrenergic stimulation of macrophages may be insufficient to impact adipose tissue inflammation or function in obesity.
Within the fat (adipose
Adipose tissue (also known as body fat or simply fat) is a loose connective tissue composed mostly of adipocytes. It also contains the stromal vascular fraction (SVF) of cells including preadipocytes, fibroblasts, Blood vessel, vascular endothel ...
) tissue of CCR2 deficient mice
A mouse (: mice) is a small rodent. Characteristically, mice are known to have a pointed snout, small rounded ears, a body-length scaly tail, and a high breeding rate. The best known mouse species is the common house mouse (''Mus musculus' ...
, there is an increased number of eosinophils, greater alternative macrophage activation, and a propensity towards type 2 cytokine
Cytokines () are a broad and loose category of small proteins (~5ŌĆō25 kDa) important in cell signaling.
Cytokines are produced by a broad range of cells, including immune cells like macrophages, B cell, B lymphocytes, T cell, T lymphocytes ...
expression. Furthermore, this effect was exaggerated when the mice became obese from a high fat diet. This is partially caused by a phenotype switch of macrophages induced by necrosis of fat cells (adipocyte
Adipocytes, also known as lipocytes and fat cells, are the cell (biology), cells that primarily compose adipose tissue, specialized in storing energy as fat. Adipocytes are derived from mesenchymal stem cells which give rise to adipocytes through ...
s). In an obese individual some adipocytes burst and undergo necrotic death, which causes the residential M2 macrophages to switch to M1 phenotype. This is one of the causes of a low-grade systemic chronic inflammatory state associated with obesity.
Intestinal macrophages
Though very similar in structure to tissue macrophages, intestinal macrophages have evolved specific characteristics and functions given their natural environment, which is in the digestive tract. Macrophages and intestinal macrophages have high plasticity causing their phenotype to be altered by their environments. Like macrophages, intestinal macrophages are differentiated monocytes, though intestinal macrophages have to coexist with the microbiome
A microbiome () is the community of microorganisms that can usually be found living together in any given habitat. It was defined more precisely in 1988 by Whipps ''et al.'' as "a characteristic microbial community occupying a reasonably wel ...
in the intestines. This is a challenge considering the bacteria found in the gut are not recognized as "self" and could be potential targets for phagocytosis by the macrophage.
Role in disease
Intestinal macrophages have been shown to play a role in inflammatory bowel disease
Inflammatory bowel disease (IBD) is a group of inflammatory conditions of the colon and small intestine, with Crohn's disease and ulcerative colitis (UC) being the principal types. Crohn's disease affects the small intestine and large intestine ...
(IBD), such as Crohn's disease
Crohn's disease is a type of inflammatory bowel disease (IBD) that may affect any segment of the gastrointestinal tract. Symptoms often include abdominal pain, diarrhea, fever, abdominal distension, and weight loss. Complications outside of the ...
(CD) and ulcerative colitis
Ulcerative colitis (UC) is one of the two types of inflammatory bowel disease (IBD), with the other type being Crohn's disease. It is a long-term condition that results in inflammation and ulcers of the colon and rectum. The primary sympto ...
(UC). In a healthy gut, intestinal macrophages limit the inflammatory response in the gut, but in a disease-state, intestinal macrophage numbers and diversity are altered. This leads to inflammation of the gut and disease symptoms of IBD. Intestinal macrophages are critical in maintaining gut homeostasis
In biology, homeostasis (British English, British also homoeostasis; ) is the state of steady internal physics, physical and chemistry, chemical conditions maintained by organism, living systems. This is the condition of optimal functioning fo ...
. The presence of inflammation or pathogen alters this homeostasis, and concurrently alters the intestinal macrophages. There has yet to be a determined mechanism for the alteration of the intestinal macrophages by recruitment of new monocytes or changes in the already present intestinal macrophages.
Media
File:S4-J774 Cells with Conidia in Liquid Media.ogg, An active J774 macrophage is seen taking up four conidia
A conidium ( ; : conidia), sometimes termed an asexual chlamydospore or chlamydoconidium (: chlamydoconidia), is an asexual, non- motile spore of a fungus. The word ''conidium'' comes from the Ancient Greek word for dust, ('). They are also ...
in a co-operative manner. The J774 cells were treated with 5ng/ml interferon-╬│ one night before filming with conidia. Observations were made every 30s over a 2.5hr period.
File:S3-Alveolar Macrophages with Conidia in Liquid Medium.ogv, Two highly active alveolar macrophage
An alveolar macrophage, pulmonary macrophage, (or dust cell, or dust eater) is a type of macrophage, a phagocytosis#Professional phagocytic cells, professional phagocyte, found in the airways and at the level of the pulmonary alveolus, alveoli in ...
s can be seen ingesting conidia
A conidium ( ; : conidia), sometimes termed an asexual chlamydospore or chlamydoconidium (: chlamydoconidia), is an asexual, non- motile spore of a fungus. The word ''conidium'' comes from the Ancient Greek word for dust, ('). They are also ...
. Time lapse is 30s per frame over 2.5hr.
History
Macrophages were first discovered late in the 19th century by zoologist ├ēlie Metchnikoff
Ilya Ilyich Mechnikov (; ŌĆō 15 July 1916), also spelled ├ēlie Metchnikoff, was a zoologist from the Russian Empire of Moldavian noble ancestry and alshereat archive.org best known for his research in immunology (study of immune systems) and ...
. Metchnikoff revolutionized the branch of macrophages by combining philosophical insights and the evolutionary study of life. Later on, Van Furth during the 1960s proposed the idea that circulating blood monocytes in adults allowed for the origin of all tissue macrophages. In recent years, publishing regarding macrophages has led people to believe that multiple resident tissue macrophages are independent of the blood monocytes as it is formed during the embryonic stage of development. Within the 21st century, all the ideas concerning the origin of macrophages (present in tissues) were compiled together to suggest that physiologically complex organisms, from macrophages independently by mechanisms that don't have to depend on the blood monocytes.
See also
* Bacteriophage
A bacteriophage (), also known informally as a phage (), is a virus that infects and replicates within bacteria. The term is derived . Bacteriophages are composed of proteins that Capsid, encapsulate a DNA or RNA genome, and may have structu ...
* Dendritic cell
A dendritic cell (DC) is an antigen-presenting cell (also known as an ''accessory cell'') of the mammalian immune system. A DC's main function is to process antigen material and present it on the cell surface to the T cells of the immune system ...
* Histiocyte
* List of distinct cell types in the adult human body
References
{{Authority control
Phagocytes
Cell biology
Immune system
Human cells
Articles containing video clips
Connective tissue cells
Lymphatic system
 A majority of macrophages are stationed at strategic points where microbial invasion or accumulation of foreign particles is likely to occur. These cells together as a group are known as the
A majority of macrophages are stationed at strategic points where microbial invasion or accumulation of foreign particles is likely to occur. These cells together as a group are known as the  Macrophages can internalize antigens through receptor-mediated phagocytosis. Macrophages have a wide variety of pattern recognition receptors (PRRs) that can recognize microbe-associated molecular patterns (MAMPs) from pathogens. Many PRRs, such as
Macrophages can internalize antigens through receptor-mediated phagocytosis. Macrophages have a wide variety of pattern recognition receptors (PRRs) that can recognize microbe-associated molecular patterns (MAMPs) from pathogens. Many PRRs, such as 
 Melanophages are a subset of tissue-resident macrophages able to absorb pigment, either native to the organism or exogenous (such as tattoos), from extracellular space. In contrast to dendritic juncional
Melanophages are a subset of tissue-resident macrophages able to absorb pigment, either native to the organism or exogenous (such as tattoos), from extracellular space. In contrast to dendritic juncional